Abstract
Cutaneous lung tissue heterotopia is a very rare disorder where mature lung tissues develop in the skin. This is only the second known report of cutaneous lung tissue heterotopia, with the first by Singer et al. in 1998. A newborn infant had a hemangioma-like, freely movable mass connected to the anterior aspect of the sternal manubrium. Pathologic findings showed mature lung tissues with bronchi, bronchioles, and alveoli through the dermis and subcutis, and it was diagnosed as cutaneous lung tissue heterotopia. Cutaneous lung tissue heterotopia is hypervascular, so grossly it looks like a hemangioma. It can be differentiated from pulmonary sequestration, teratoma, bronchogenic cyst, and branchial cleft cyst by histology and the location of the mass. We describe the clinical, radiologic, and pathologic findings of a cutaneous lung tissue heterotopia, the first reported in Korea.
Cutaneous lung tissue heterotopia is a rare and peculiar disorder characterized by well-formed, mature lung tissue formation with bronchi, bronchioles, and alveoli in the skin. It looks like a hemangioma due to extensive vasculature, but is composed of mature lung tissue. The only other reported case was a 3-yr-old girl with lung heterotopia on the skin over the scapula (1). We describe the clinical, radiological, and pathological properties of a heterotopia of lung tissue in the skin over the anterior suprasternal area of the neck in a newborn infant. This is the first report of mature lung tissue in the skin reported in Korea.
A male newborn infant (date of birth July 6, 2009), weighing 3,480 g at 39 weeks and 2 days of gestation, was delivered by cesarean section due to a prenatally detected huge mass on the anterior aspect of the neck identified by pelvic magnetic resonance imaging at 19 weeks of gestation. He presented with a 4.2×3.5×1.0 cm reddish brown hemangioma-like protruding mass connected to the middle of the manubrium of the sternum by a band-like stalk. The surface of the mass was wrinkled, and vessel tissues were visible under the surface. The mass was freely movable, soft, and tender (Fig. 1). A chest computed tomographic scan revealed that an anterior chest wall mass that was lobulated, hypervascular, and highly enhanced, and contained two arteries and veins which crossed the middle of the manubrium of the sternum (Fig. 2A). These vessels inside the mass were connected to the internal mammary arteries and veins. Another 1.1×2.3 cm highly enhanced mass was located in the anterior mediastinum between the sternum and heart, and was similar to the anterior chest wall mass (Fig. 2B). On the 8th postnatal day, he underwent an excision operation of the mass under general anesthesia. The excised mass measured 4.2×3.5×1.0 cm, and the cut surface showed a tan to brownish, multi-lobulated, sponge-form lesion in the dermis and subcutis. The specimen was fixed in 10% formalin and routinely processed. On microscopic examination of hematoxylin-eosin stained slides, lobulated lung parenchymal tissue and a dilated bronchus with mature cartilages were seen in the dermis and subcutis (Fig. 3A). The lung parenchymal tissue showed small bronchioles lined by columnar cells and alveolar spaces containing alveolar macrophages (Fig. 3B). These columnar epithelia and alveolar epithelial cells revealed nuclear positivity on immunohistochemical stain for TTF-1 (anti-thyroid transcription factor-1, clone: 8G7G3/1, Glostrup, Denmark, Dako), marker of type II cell and Clara cell of the lung (Fig. 3C). The overlying skin and skin appendages were unremarkable, and no other unusual histologic components suggesting teratoma were present. Mesothelial cells were not seen. He is one month old now, has no respiratory symptoms, and is being followed at out- patient clinic.
Cutaneous lung tissue heterotopia is hypervascular and looks like a hemangioma grossly and radiologically. However, pathologic examination shows well-formed, mature lung tissue formation in the skin, namely bronchi consisted of cartilage, bronchioles, and alveoli through the dermis and subcutis (1). It was first reported in a 3-yr-old girl on the skin over the scapula by Singer (1). Mahler et al. (2) reported cutaneous ectopic respiratory epithelium, but not respiratory mucosa, on the anterolateral neck, suggesting a branchial cleft remnant. Alfadley et al. (3) described cutaneous ectopic respiratory mucosa on the arm, suggesting abnormal limb buds containing sequestrated cells from the branchial cleft. Cutaneous lung tissue heterotopia is easily differentiated from pulmonary sequestration, teratoma, bronchogenic cyst, and branchial cleft cyst by histology and the location of the mass. Pulmonary sequestration is a nonfunctioning lung tissue supplied by a systemic artery, not connected to bronchi, and containing a mesothelial cell layer (4, 5). We did not find a mesothelial cell layer in this case. Teratoma is composed of multiple cell types originating from more than one germ layer, and usually all three layers (6). Moreno et al. (7) reported cutaneous cystic teratoma with hair follicles, eccrine sweat glands and ducts, and ciliated respiratory epithelium with goblet cells in the middle of the back in a 5-yr-old girl. The larynx and trachea of the upper respiratory tract typically has ciliated pseudostratified columnar epithelium, so cutaneous bronchogenic cysts are lined by ciliated pseudostratified columnar epithelium with goblet cells and contain mesenchymal components such as smooth muscles and cartilage (8). It is usually found in the pre-sternal area around the sternal notch, but can occur over the scapula (9, 10). Branchial cleft cysts contain stratified squamous epithelium or occasionally ciliated pseudostratified columnar epithelium, and have continuity with a sebaceous gland. These cysts prominently have lymphoid nodules, but rarely have smooth muscle or cartilage, and are usually located in the anterolateral aspect of the neck (11). Bronchogenic cysts and branchial cleft cysts usually include cysts, sinuses, and fistulas, and can be differentiated from lung tissue heterotopias. Cutaneous bronchogenic cysts occur from impaired or delayed midline fusion of the mesenchymal bars of the sternum, so the accessory buds from the primitive tracheobronchial tree that originate from the ventral portion of the primitive foregut are sequestrated in the pre-sternal area (12). Cutaneous bronchogenic cysts are therefore located in the anterior of the sternal notch. The exact etiology of cutaneous lung tissue heterotopia is not known, and the development of lung tissue in the pre-sternal area in this case report is difficult to explain, but may involve a similar process as pre-sternal cutaneous bronchogenic cysts. Ectopic tissues in the skin such as cutaneous lung tissue heterotopias, pulmonary sequestration, bronchogenic cysts, branchial cleft cysts, thyroglossal duct cysts, or teratoma, generally require total excision because of the concern for potential malignancies. In conclusion, this report describes the first case of cutaneous lung tissue heterotopia in Korea, as confirmed and differentiated from pulmonary sequestration, bronchogenic cyst, branchial cleft cyst, and teratoma by pathologic findings.
Figures and Tables
Fig. 1
Reddish brown hamangioma-like mass on the sternal manubrium. (A, B) 4.2×3.5×1.0 cm hemangioma-like protruding mass was connected to the middle of sternal manubrium by a stalk. The surface of the mass was wrinkled and vessel-like tissue was visible under the surface. The mass was freely movable and soft.

Fig. 2
Chest CT images. (A) Chest CT showed the mass was lobulated, hypervascular, and highly enhanced, and contained two arteries and veins (arrow) that cross the middle of the sternal manubrium. (B) These vessels were connected to the internal mammary arteries and veins (arrow). A similar 1.1×2.3 cm highly enhancing mass (arrowhead) was located in the anterior mediastinum.
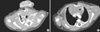
Fig. 3
Histologic findings. (A) Lobulated lung parenchymal tissue (arrow) and a dilated bronchus (arrowhead) with mature cartilages are seen in dermis and subcutis (H&E, ×40). (B) Lung parenchymal tissue is composed of bronchioles lined by columnar epithelia and alveolar spaces containing alveolar macrophages (H&E, ×200). (C) The columnar epithelia and alveolar lining cells are TTF-1 positive.

References
1. Singer G, Haag E, Anabitarte M. Cutaneous lung tissue heterotopia. Histopathology. 1998. 32:60–62.

2. Mahler V, Wurm J, Von den Driesch P. Ectopic respiratory epithelium associated with multiple malformations. Br J Dermatol. 1997. 136:933–934.

3. Alfadley A, Hainau B, Al Aboud K, Hamadah IR, Al Hawsawi K. Ectopic respiratory mucosa in the skin associated with skeletal malformation and polydactyly. J Am Acad Dermatol. 2000. 43:939–942.

4. Conran RM, Stocker JT. Extralobar sequestration with frequently associated congenital cystic adenomatoid malformation, type 2: report of 50 cases. Pediatr Dev Pathol. 1999. 2:454–463.

5. Zeidan S, Hery G, Lacroix F, Gorincour G, Potier A, Dubus JC, Guys JM, de Lagausie P. Intralobar sequestration associated with cystic adenomatoid malformation: diagnostic and thoracoscopic pitfalls. Surg Endosc. 2009. 23:1750–1753.

8. Fraga S, Helwig EB, Rosen SH. Bronchogenic cysts in the skin and subcutaneous tissue. Am J Clin Pathol. 1971. 56:230–238.

9. Tresser NJ, Dahms B, Berner JJ. Cutaneous bronchogenic cyst of the back: a case report and review of the literature. Pediatr Pathol. 1994. 14:207–212.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download