Abstract
This study was done to evaluate prospectively the clinical significance of colonic diverticulosis. In the 1,030 consecutive outpatients undergoing colonoscopy, the information on the demographics, the patterns of bowel symptoms, and the prevalence of colon polyp were analyzed according to the presence of colonic diverticulosis. The mean age of 1,030 patients were 52.2 yr and 59.3% were male. The prevalence of diverticulosis was 19.7% (203/1,030). Of 203 diverticulosis patients 85.2% were in proximal group, 5.4% in distal group and 9.4% in both group. Six (3.0%) patients were found to have diverticulitis. Multivariate logistic regression analysis showed that an old age, diabetes and the presence of polyp were significant factors associated with proximal or both diverticulosis. A significant difference was demonstrated between the patients of distal diverticular group and the controls for the symptom frequency scores within the previous 4 weeks. The items, which showed difference, were hard stool, urgency, flatus, chest discomfort and frequent urination. In conclusion, old age, diabetes and the presence of colon polyp were associated with proximal diverticulosis. The temporal symptoms were more frequent in distal diverticulosis than in proximal diverticulosis in the study subjects.
Colonic diverticulosis is commonly found in Western countries (1-3). The characteristics of diverticulosis are: the incidence is increased with age, the main lesion is generally located on the left colon, and the disease has a high complication rate (4). However, different characteristics of diverticulosis have been reported in Asian countries, such as its low incidence, main lesion generally limited to the right colon, a relatively small number of lesions, occurrence in young adults, and the lesions being mostly true diverticula (4). Nowadays, it seems that the adoption of a western lifestyle in Asian countries may result in a higher prevalence of diverticulosis (2).
The clinical significance of diverticulosis such as the patterns of symptoms or the association with colonic polyps has been studied during the last decades. Although the patients with diverticulosis are usually asymptomatic, one fourth of the patients was reported to suffer from various symptoms (2) ranging from irritable bowel syndrome (IBS)-type symptoms to disabling recurrent abdominal pain (3, 5). Although an association between diverticulosis and colorectal neoplasia has been suggested to exist in Western countries (6), there is limited literature reporting the association in Asia.
The present study was conducted to describe the patterns of bowel symptoms and the association with colonic polyps in patients with colonic diverticulosis, and to evaluate clinical significance of colonic diverticulosis.
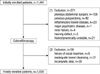
The protocol of this prospective study was approved by the Institutional Review Board of the Catholic University of Korea (VCMC08OT004). The study was conducted at St. Vincent's Hospital, a teaching hospital of the Catholic University School of Medicine. Informed consent was obtained from all the patients or their guardians before enrolled in the study. The consecutive outpatients, over 17 yr of age, who visited an endoscopic medical clinic from February 2008 and January 2009 for elective colonoscopy were eligible for study participation. The exclusion criteria were previous abdominal surgery, previous polypectomy, a past or current diagnosis of inflammatory bowel disease, major psychiatric disease, pregnancy or breast-feeding, failure of cecal insertion, incomplete data, a past or current diagnosis of renal failure (creatinine >2.5 mg/dL), inadequate bowel cleansing, hemodynamically unstable patients and the presence of a communication disorder such as a hearing defect.
The colonoscopic examinations were performed by five board-certified endoscopists via a single handed method and using a standard video colonoscope (a CF240 or CF260, Olympus Optical, Tokyo, Japan). The patients were instructed to take a polyethylene glycol-electrolyte powder (PEG-ES) (COLONLYTE POWD 4 L, Meditech Korea Pharm, Seoul, Korea) that was reconstituted with 4 L of water. The patients were advised to start the bowel cleansing at 7 a.m. and drink 250 mL every 10-15 min to at least until 11 a.m. All of colonoscopic examinations were conducted between 1:30 p.m. and 5:00 p.m. under conscious sedation using midazolam and meperidine as tolerated by the patients' cardiorespiratory parameters. A procedure was defined as successful if base of the cecum or observed end of the colon could be touched with tip of the colonoscope. We classified patients as the diverticular group and the controls according to the finding of colonoscopy.
The demographic data (age, gender and body mass index), comorbidities and a history of smoking or alcohol consumption were obtained before colonoscopy. The bowel symptoms enquired before the procedures, presence or absence of diverticulosis and colon polyps as found in the procedure were evaluated. The presence of diverticulosis and its association with the demographic characters, and the parameters of the other variables (colon polyps and bowel symptoms), were analyzed.
The number and location of diverticula were recorded during colonoscopy along the segment of the colon. The distal colon was defined as the portion of colon distal to the splenic flexure, including the descending colon, sigmoid colon and rectum. The proximal colon was all segments of the colon proximal to the splenic flexure (6). All the patients in diverticulosis groups were classified as proximal, distal and both diverticulosis according to their subsites. The number of diverticula were classified as three categories: "few" if found only one, "several" if found two to five, and "many" if found six or more diverticula. The complications of diverticulosis, diverticulitis were also examined.
The number and presence of colon polyps were evaluated according to the site of diverticulosis. In addition, advanced neoplasia was evaluated, which was defined as a tubular adenoma ≥1 cm in size, any polypoid lesion with a villous histology, high-grade dysplasia or cancer.
During the procedures, the quality of the colon cleansing was assessed using the validated Aronchick scale (7, 8). The scale is 1 (excellent preparation), when more than 90% of the mucosa was seen, mostly liquid stool and minimal suction was needed for adequate visualization; 2 (good preparation), when more than 90% of the mucosa seen, mostly liquid stool and significant suction was needed for adequate visualization; 3 (fair preparation), when more than 90% of the mucosa was seen, a mixture of liquid and semisolid stool could be suctioned and/or washed out; 4 (inadequate preparation), when less than 90% of the mucosa was seen, a mixture of semisolid and solid stool could not be suctioned or washed out.
Before the colonoscopic procedures, patients were asked about their bowel symptoms by questionnaire form (9), which included the Rome III criteria and additional questions concerning bowel symptoms. The Rome III criteria classified IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), mixed IBS (IBS-M) or the unsubtyped IBS (IBS-U). In addition, a total of thirteen bowel symptoms experienced in previous 4 weeks were asked (9). The asked bowel symptoms included abdominal discomfort, pain or cramps, hard or lumpy stools, loose or watery stools, straining during a bowel movement, having to rush to the toilet for a bowel movement (urgency), passing mucus (white material) during a bowel movement, abdominal fullness/bloating or swelling, passing gas, heartburn or chest pain, feeling full soon after starting a meal, passing urine frequently, and nausea. The severity of symptoms were evaluated by the total symptom score, which was defined the sum of the symptom frequency and the bothersomeness. The frequency of each symptom was assessed using a seven point scale: 0=never; 1=almost never; 2=seldom; 3=sometimes; 4=often; 5=almost always; 6=always. The bothersomeness of each symptom was assessed using a seven point scale: 0=not bothersome to 7=extremely bothersome. The possible range of scores for each frequency or bothersomeness was 0 to 78.
The primary end points of the study were the severity of bowel symptoms, and the frequency of colon polyps, according the presence and the location of diverticulosis. The secondary end points were the prevalence and the complications of diverticulosis according the location of diverticulosis. Continuous data was expressed as mean±SD and it was analyzed using independent samples t tests, whereas the categorical variables were expressed as quantities and they were analyzed using chi-squared tests. Multiple stepwise logistic regression analysis was used to identify the independent factors associated with diverticulosis. All the analyses were performed with a statistical software package (SPSS, version 15.0; SPSS Inc). A P value less than 0.05 was considered significant for all tests.
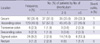
A total of 1,441 consecutive patients who underwent elective colonoscopy were enrolled during the study period. A total of 410 patients were excluded (Fig. 1). Finally, 1,030 patients were included in the analysis. The mean age of the patients was 52.2±11.2 yr (range: 19 to 86 yr) and 611 patients (59.3%) were male. The prevalence of the patients with colonic diverticulosis, as assessed by colonoscopy, was 19.7% (203/1,030). Among the 203 patients with diverticulosis (the diverticular group), 173 (85.2%) was proximal diverticular group, 11 (5.4%) was distal diverticular group and 19 (9.4%) was both proximal and distal diverticular group. On the univariate analysis, the male gender, an old age, smoking, diabetes, hypertension, dyslipidemia and cardiovascular disease were found to be significantly different between the total diverticular group and controls. The proximal diverticular group was associated with male gender, diabetes, cardiovascular disease and smoking, whereas the distal diverticular group was related with age, cardiovascular disease and alcohol consumption (Table 1). The total number of diverticula was 260. The number and type of diverticula according to each segment are shown in Table 2. In the "few" category patients, 95% (95/100) were located in the proximal colon and 5% (5/100) were in the distal colon. In the "several" or "many" category patients, 17.5% were in the distal colon and 82.5% were in the proximal colon. A significant difference was observed between the "few" and the "several" and "many" categories of diverticula according to the sites of diverticulosis (P<0.01) (Fig. 2). On colonoscopy, 6 (3.0%) patients were found to have diverticulitis, 4 cases of which were seen in the proximal colon.
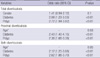
Prevalence of the patients with colonic polyps was 40.6% (418/1030). Of them 21.5% (90 patients) had advanced neoplasia. On the univariate analysis, the prevalence of colon polyps and advanced neoplasia in the diverticular group was found to be significantly higher than that in the controls. Irrespective of the site of diverticulosis, significantly higher rates of polyps or advanced neoplasia were demonstrated for all the patients with diverticulosis than that for the controls, except for the distal diverticular group with advanced neoplasia, and this group had only a high tendency (P=0.1) (Table 3).
The success rate of colonoscopic insertion to the terminal ileum was 95.7% (986/1,030). The score of the Aronchick scale was significantly higher for the diverticular group than that for the controls, irrespective of the site of diverticulosis (Table 3). Multivariate logistic regression analysis was performed with the variables such as gender, age, the body mass index, a history of diabetes or hypertension, smoking, alcohol consumption, the presence of polyp and the presence of IBS. Diabetes and the presence of polyp were the significant independent factors associated with the the total, both, and the proximal diverticulosis, respectively. Age was an additional associated factors for the proximal and both diverticulosis. None of the variables were associated with distal diverticulosis (Table 4).
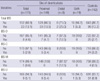
Of the 1,030 enrolled patients, 113 were excluded from the analysis of bowel symptoms due to the presence of diverticulitis, refusal to fill up the questionnaires. Therefore, the remaining 917 patients were finally analyzed for the associatied bowel symptoms. According to the presence of IBS or the subtypes of IBS, no significant differences were shown between all the kinds of diverticular groups and the controls except for distal diverticular group for type of IBS-M (Table 5). No significant differences were shown between the controls and all the diverticular groups for the bothersome symptoms or the total symptom score. However, for the symptom frequency scores, a significant difference was shown between the distal diverticular group and the controls (Fig. 3). On further analysis, the mean score of the symptom frequency for the patients in the distal diverticular group was significantly higher than that of the controls for the items of hard stool, urgency, flatus, chest discomfort and frequent urination (Fig. 4).
The prevalence of diverticulosis in Asia has gradually increased because of the reduced fiber diet; that is due to adapting a western life style (2, 10). However, the clinical significance of diverticulosis is not well known in Asia. The current study showed that colonic diverticulosis was associated with an old age, a high prevalence of colon polyp and diabetes. In view of the bowel symptoms, diverticulosis was not associated with IBS, yet recently developed low abdominal symptoms were associated with distal diverticulosis.
The diverticulosis in Asia have been known to show several distinct characteristics. And these are being limited in the right colon and to relatively young patients, being mostly true diverticula or congenital, a single lesion or up to a few lesions, a low incidence rate and a low complication rate (4, 5, 11). The distinct characteristic of diverticulosis, that is different between the West and Asia, is the predominant proximal location of the colon in Asia. Although the prevalence of diverticular disease in Asia has varied according to studies (2, 12, 13), our study showed that the prevalence of diverticulosis was 19.7%, which is one of the highest rates in Asia. The reason for this might be due to the prospective colonoscopic examination that recognized small diverticula. Another reason may be lifestyle changes of the westernized diet. The proportion of proximal colonic diverticulosis was 85.2%, and this was the highest rate as compared with those reports from Asia as well as those from West. Isolated proximal diverticulosis was common in our study, which was compatible with that of previous reports (11, 12). It is thought that the prevalence and number of cases of diverticulosis in Asia are still affected by a congenital factor despite that the diverticulosis occurs due to acquired factors. The prevalence of diverticulitis among the patients with diverticulosis was found 3%, which was slightly higher than previous reports (1-2.5%) (2, 14). Prevalence of diverticulitis has been considered overestimated because most of the subjects who visited referral hospitals for colonoscopy had abdominal symptoms and they had the chance to suffer from complicatied diverticulosis. Between 10 and 25% of the patients with symptomatic uncomplicated diverticular disease suffer from diverticulitis (15, 16).
Recently, the association between diverticulosis and colon polyps was evaluated according to the common mechanisms of slow colonic transit and low fiber diet consumption, but most of the reported studies have focused on distal diverticulosis (2, 6, 15, 17). In our study, the prevalence of colon polyp in the diverticular group was found to be significantly higher than those in the controls, and in the proximal diverticulosis group. In addition, we analyzed the subgroup with advanced neoplasia for the association with diverticulosis, which is actually more important in the clinic.
Factors associated with diverticulosis have been variably suggested; yet the relationship between diverticulosis and the demographic factors or the factors of the polyps have only partly demonstrated. Because the factors affecting diverticulosis have a common mechanism of slow colonic transit, which might allow the factors to cross-react, it was necessary to analyze all the factors related with diverticulosis together in order to find independent factors. On the multivariate analysis considering all the factors, the proximal diverticulosis was associated with such independent factors as the presence of diabetes, age and the presence of polyp.
In clinical practice, we encounter various kinds of abdominal symptoms in patients with diverticulosis, but the etiology of the symptoms is unknown in most cases (15, 18). Pathophysiology and clinical features of diverticulosis have been reported from the West (2, 5, 19, 20), while these types of studies are rare in Asia. At least one fourth of patients with diverticulosis are known to have a chance to develop symptoms (2), and some overlap exists between diverticular disease and IBS (21-23). Alterations in colonic transit were reported to be associated with abdominal pain in patients with colonic diverticulosis, and this has also been observed in patients with IBS (15, 24). The abdominal symptoms of the validated questionnaire were analyzed in this study. However, any difference in the prevalence of IBS between the diverticular group and the controls was not found. Prevalence of diverticulosis was reported to be not different between the IBS and the non-IBS group (25). Although the common mechanism of alterations in colonic transit was suggested, multiple factors could play a role in IBS and diverticulosis, and the Rome criteria was not a good tool to distinguish IBS (21). However, a difference of the symptom frequency scores experienced in previous 4 weeks was showed between the distal diverticular group and the controls. Interestingly, the frequency scores of the individual symptom items such as hard stool, urgency, flatus, frequent urination and chest discomfort in the distal diverticular group were higher than those in the controls, whereas the score of the proximal diverticular group was not different from that of the controls. This result was compatible with results of a previous report (26), which demonstrated that the diverticular group had a relatively short illness history on presentation. Although the reason why abdominal symptoms are distinct especially only in the distal diverticular group, is not well understood, whether the development of diverticulosis is congenital or acquired might be the clue. The distal diverticulosis is considered to be an acquired herniation (26, 27) that is due to the condition of pulsation. In addition, the colonic compliance of the patients in distal diverticular group was thought to be lower than that in the proximal diverticular group (12, 28). A report showed a temporal correlation between abdominal pain and colonic contractile activity in the patients with diverticulosis (24). Whatever, a short period of abdominal symptoms may be associated with distal diverticulosis.
The following factors were considered to heighten objective validity of our study. The diverticulosis was confirmed by colonoscopy. And we excluded patients with infection, inflammation, tumor and the complications of diverticulosis such as bleeding, and diverticulitis. A prospective controlled method was chosen to exclude the selection bias. Additionally, to find the clinical significance of diverticulosis, various factors related with diverticulosis were collected and analyzed together.
The potential limitation of our study is the small number of enrolled patients with distal diverticulosis, in which any significant independent factors were not demonstrated on the multivariate analysis. However, the independent factors of the both type of diverticulosis were demonstrated despite the small number of patients. Anyhow different characteristics between distal and proximal diverticulosis might exist.
In conclusion, old age, diabetes and the presence of colon polyp were associated with proximal diverticulosis. The temporal symptoms are more frequent in distal diverticulosis than in proximal diverticulosis in Koreans.
Figures and Tables
 | Fig. 2The prevalence between the types of few, and the other types (several and many) of diverticulosis according to the sites of diverticulosis (chi-square test, P<0.01). |
 | Fig. 4Symptom frequency score in the diverticular groups and control.
*P value <0.05; †P vaule <0.01.
|
References
1. Sheth AA, Longo W, Floch MH. Diverticular disease and diverticulitis. Am J Gastroenterol. 2008. 103:1550–1556.

2. Parra-Blanco A. Colonic diverticular disease: pathophysiology and clinical picture. Digestion. 2006. 73:Suppl 1. 47–57.

3. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007. 357:2057–2066.
4. Takano M, Yamada K, Sato K. An analysis of the development of colonic diverticulosis in the Japanese. Dis Colon Rectum. 2005. 48:2111–2116.

5. Simpson J, Neal KR, Scholefield JH, Spiller RC. Patterns of pain in diverticular disease and the influence of acute diverticulitis. Eur J Gastroenterol Hepatol. 2003. 15:1005–1010.

6. Kieff BJ, Eckert GJ, Imperiale TF. Is diverticulosis associated with colorectal neoplasia? A cross-sectional colonoscopic study. Am J Gastroenterol. 2004. 99:2007–2011.

7. Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G. A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc. 2000. 52:346–352.

8. Radaelli F, Meucci G, Imperiali G, Spinzi G, Strocchi E, Terruzzi V, Minoli G. High-dose senna compared with conventional PEG-ES lavage as bowel preparation for elective colonoscopy: a prospective, randomized, investigator-blinded trial. Am J Gastroenterol. 2005. 100:2674–2680.

9. Park JM, Choi MG, Kim YS, Choi CH, Choi SC, Hong SJ, Jeong JJ, Lee DH, Lee JS, Lee KJ, Son HJ, Sung IK. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009. 18:435–446.

10. Miura S, Kodaira S, Shatari T. Recent trends in diverticulosis of the right colon in Japan: retrospective review in a regional hospital. Dis Colon Rectum. 2000. 43:1383–1389.
11. Chia JG, Wilde CC, Ngoi SS, Goh PM, Ong CL. Trends of diverticular disease of the large bowel in a newly developed country. Dis Colon Rectum. 1991. 34:498–501.

12. Nakada I, Ubukata H, Goto Y, Watanabe Y, Sato S, Tabuchi T, Soma T, Umeda K. Diverticular disease of the colon at a regional general hospital in Japan. Dis Colon Rectum. 1995. 38:755–759.

13. Kim BH, Lee SH, Lee SS, Oh DJ, Chung ES, Lee SJ. Diverticular disease of the colon in Korea. Korean J Intern Med. 1987. 2:79–83.

14. Petruzziello L, Iacopini F, Bulajic M, Shah S, Costamagna G. Review article: uncomplicated diverticular disease of the colon. Aliment Pharmacol Ther. 2006. 23:1379–1391.

15. Parks TG. Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J. 1969. 4:639–642.

16. Imperiali G, Meucci G, Alvisi C. Segmental colitis associated with diverticula: a prospective study. Am J Gastroenterol. 2000. 95:1014–1016.

17. Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of western civilization. Br Med J. 1971. 2:450–454.

18. Simpson J, Scholefield JH, Spiller RC. Origin of symptoms in diverticular disease. Br J Surg. 2003. 90:899–908.

19. Humes DJ, Simpson J, Neal KR, Scholefield JH, Spiller RC. Psychological and colonic factors in painful diverticulosis. Br J Surg. 2008. 95:195–198.

20. Comparato G, Fanigliulo L, Aragona G, Cavestro GM, Cavallaro LG, Leandro G, Pilotto A, Nervi G, Soliani P, Sianesi M, Franzé A, Di Mario F. Quality of life in uncomplicated symptomatic diverticular disease: is it another good reason for treatment? Dig Dis. 2007. 25:252–259.

21. Kang JY, Melville D, Maxwell JD. Epidemiology and management of diverticular disease of the colon. Drugs Aging. 2004. 21:211–228.

22. Otte JJ, Larsen L, Andersen JR. Irritable bowel syndrome and symptomatic diverticular disease: different diseases? Am J Gastroenterol. 1986. 81:529–531.
23. Schoetz DJ Jr. Diverticular disease of the colon: a century-old problem. Dis Colon Rectum. 1999. 42:703–709.
24. Bassotti G, Battaglia E, De Roberto G, Morelli A, Tonini M, Villanacci V. Alterations in colonic motility and relationship to pain in colonic diverticulosis. Clin Gastroenterol Hepatol. 2005. 3:248–253.

25. Akhtar AJ, Shaheen MA, Zha J. Organic colonic lesions in patients with irritable bowel syndrome (IBS). Med Sci Monit. 2006. 12:CR363–CR367.

26. Domjan J, Blaquiere R, Odurny A. Is minimal preparation computed tomography comparable with barium enema in elderly patients with colonic symptoms? Clin Radiol. 1998. 53:894–898.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download