Abstract
Gastroesophageal reflux disease (GERD) is caused by abnormal reflux of gastric contents into the esophagus. GERD can be divided into two groups, erosive esophagitis and non-erosive reflux disease (NERD). The aim of this study was to compare the clinical characteristics of patients with erosive esophagitis to those with NERD. All participating patients underwent an upper endoscopy during a voluntary health check-up. The NERD group consisted of 500 subjects with classic GERD symptoms in the absence of esophageal mucosal injury during upper endoscopy. The erosive esophagitis group consisted of 292 subjects with superficial esophageal erosions with or without typical symptoms of GERD. Among GERD patients, male gender, high body mass index, high obesity degree, high waist-to-hip ratio, high triglycerides, alcohol intake, smoking and the presence of a hiatal hernia were positively related to the development of erosive esophagitis compared to NERD. In multivariated analysis, male gender, waist-to-hip ratio and the presence of a hiatal hernia were the significant risk factors of erosive esophagitis. We suggest that erosive esophagitis was more closely related to abdominal obesity.
Gastroesophageal reflux disease (GERD) is one of the most common gastrointestinal diseases in Western countries. Recently, the frequency of GERD symptoms has been increasing now seen in approximately one-third of the adult population (1, 2). In contrast, the prevalence of GERD in East Asia is much lower than that seen in the West, ranging from 3% to 7% for people with at least weekly symptoms of heartburn and/or acid regurgitation (3-5). However, Korean society is becoming increasingly westernized, and it is expected that the prevalence of GERD will increase.
GERD is caused by abnormal reflux of gastric contents into the esophagus and is characterized by specific symptoms such as heartburn and acid regurgitation (6-8). However, on endoscopy, only about one-third to one-half of GERD patients has positive findings, such as erosions and ulcers. Most patients with GERD symptoms have no obvious mucosal breaks (9-11). Recently, the Montreal workshop report defined GERD as a disease which is associated with troublesome symptoms and/or complications on account of reflux of stomach contents into the esophagus (12). Therefore, GERD can be divided into two groups, erosive esophagitis and non-erosive reflux disease (NERD), according to the presence of esophageal mucosal breaks. The pathogenesis of these two categories of GERD is believed to be different. Differences in clinical characteristics between NERD and erosive esophagitis have not been well documented. In the present prospective study, we compared the clinical characteristics of patients with NERD and those with erosive esophagitis.
Between January 2004 and July 2006, 8,256 subjects underwent an upper endoscopy for a voluntary health check-up at Hanyang University Hospital. Among these subjects, a total of 792 subjects with GERD were analyzed. The NERD group consisted of 500 subjects with classic GERD symptoms in the absence of esophageal mucosal injury based on upper endoscopy findings. The erosive esophagitis group consisted of 292 subjects with superficial esophageal erosions, with or without typical symptoms of GERD. The severity of the erosive esophagitis was graded from A to D according to the LA classification. Minimal changes were classified as endoscopy-negative reflux disease in this study. Reflux symptoms were defined as having symptoms of heartburn or acid regurgitation at least once a week. Patients using a histamine-2-receptor antagonist or proton pump inhibitor were excluded. Gastroscopic findings such as hiatal hernia, Barrett's esophagus, gastric ulcer, and duodenal ulcer were also described.
The medical examination included a blood chemistry evaluation. A body composition analysis was conducted on the same day. To measure the level of obesity in the patients, we used body mass index (BMI), waist-to-hip ratio (WHR), and obesity degree (OD). BMI was calculated as the weight (kg) divided by the square of the height (m2). OD was calculated as the current weight divided by the ideal weight. Inbody 3 (Biospace, Seoul, Korea), a body composition analyzer device, automatically measured WHR and OD.
All subjects had a face-to-face interview with a nurse. In this interview, the study plan was explained and written informed consent was obtained from each patient. All of subjects were asked about their lifetime history of recurrent heartburn or regurgitation. We collected the following information on potential confounding factors: current smoking habits, current alcohol use, recent weight gain, and recent weight loss. Weight change was defined as a self-reported change in weight over the previous 6 months. Blood samples were collected from all subjects after 12 hr of fasting. Serum cholesterol and triglycerides (TG) were measured using enzymatic methods (Boehringer Mannheim, Mannheim, Germany). High density lipoprotein cholesterol (HDL-C) was measured directly with determiner HDL-C diagnostic kits (Kyowa Medex, Tokyo, Japan) using a Hitachi 747 automatic chemistry analyzer. Low density lipoprotein cholesterol (LDL-C) values were calculated from total cholesterol, HDL-C, and TG concentrations using the Friedewald formula. This study was approved by the institutional review board of our medical center (2008-26).
Values are expressed as the mean±standard deviation (SD). Categorical variables were compared using a chi-square test. Differences in mean values between the two groups were compared using unpaired t-tests. A multiple logistic regression analysis was used to evaluate the simultaneous effects of gender, BMI, WHR, OD, TG, hiatal hernia, and presence of gastric ulcer. We calculated the 95% confidence interval (CI) for each odds ratio (OR). All P values were 2-tailed. P values less than 0.05 were considered significant. Statistical analyses were performed using SPSS v13.0 for Windows.
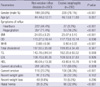
Table 1 shows the baseline characteristics of the two groups. The 292 subjects with erosive esophagitis were subdivided into four categories based on the severity of their disease. Two hundred sixteen subjects (74.0%) were placed in LA classification A. Sixty one (20.9%) were placed in LA classification B, while thirteen (4.5%) were placed in LA classification C. Two patients (0.7%) were placed in LA classification D. Among the erosive esophagitis group, twenty seven (9.3%) complained of heartburn, and fifty three (18.2%) complained of regurgitation. But, two hundred twenty subjects (75.3%) had not any symptom of GERD.
The prevalence of erosive esophagitis was significantly higher in males compared to females (P<0.001). Age was not significantly different between the two groups. The erosive esophagitis group had higher BMI (P<0.001), OD (P=0.036), and WHR (P<0.001) than the NERD group. There were no significant differences in total cholesterol, LDL, or HDL between the two groups. However, the erosive esophagitis group had a higher TG level (P=0.008) and more current alcoholics (P=0.009) and current smokers (P<0.001) than the NERD group. There was no difference in recent weight gain or loss between the two groups. In the endoscopic findings of the two groups, hiatal hernia (P<0.001) was more frequent in the erosive esophagitis group.
Crude odds ratios and multiple-adjusted odd ratios for erosive esophagitis compared to NERD are shown in Tables 2, 3. On univariate analysis, male gender (OR=5.389, 95% CI, 3.874-7.496), BMI (OR=1.716, 95% CI, 1.280-2.300), OD (OR=1.669, 95% CI, 1.229-2.267), WHR (OR=1.577, 95% CI, 1.170-2.125), TG (OR=1.383, 95% CI, 1.030-1.858), alcohol use (OR=1.540, 95% CI, 1.115-2.127), cigarette smoking (OR=2.387, 95% CI, 1.725-3.303), and the presence of hiatal hernia (OR=8.929, 95% CI, 5.613-14.204) were found to be risk factors for erosive esophagitis (Table 2).
After adjusting for gender, BMI, OD, WHR, TG, alcohol use, smoking, and hiatal hernia (Table 3), male gender was found to be at significantly increased risk for developing erosive esophagitis compared to female (OR=4.097, 95% CI, 2.647-6.343). WHR was found to be significantly associated with an increased risk for developing erosive esophagitis (OR=1.615, 95% CI, 1.026-2.541). However, other obesity-related factors, such as BMI and OD, were not associated with the risk of developing erosive esophagitis in the multiple-adjustment model. The presence of a hiatal hernia was found to be significantly associated with an increased risk of developing erosive esophagitis (OR=5.445, 95% CI, 3.286-9.020). TG level, alcohol consumption, and cigarette smoking were not significantly associated with the risk of developing erosive esophagitis in the multiple-adjustment model.
Several researchers have examined the characteristics of NERD and erosive esophagitis in the Asian population (13-16). In a recent study, Hiyama et al. (17) focused on the clinical and pathophysiologic differences between NERD and erosive esophagitis in Asian patients using both computerized and manual research of the available literature. The male to female ratio ranged from 0.59 to 1.65 in NERD patients. For erosive esophagitis patients, the male to female ratio ranged from 1.18 to 7.13. Patients with NERD in Asia were found to have a higher proportion of females, a lower frequency of hiatal hernias, a higher frequency of H. pylori infections, higher rates of severe glandular atrophy of the gastric mucosa, and frequent resistance to proton pump inhibitor therapy. These characteristics are similar to those seen in the Western NERD patients. However, there are several other characteristics commonly found in Western NERD patients, such as younger age and less obese (18). In a large study, Carlsson et al. (11) compared the clinical characteristics of patients with erosive esophagitis to those with NERD. The erosive esophagitis group was similar to the NERD group in regards to mean age, smoking and alcohol consumption, prevalence and duration of heartburn, and status of H. pylori infection. However, there were more male patients (59%) in the erosive esophagitis group. There was also an increased prevalence of hiatal hernia (56%) and an increase in the weight of both male and female patients (86 and 76 kg, respectively).
Among the risk factors mentioned above, the hypothesis of obesity as a potential cause of erosive esophagitis is biologically plausible. Obesity has been associated with increased intra-abdominal pressures (19), impaired gastric emptying (20), decreased lower esophageal sphincter pressure, and an increased frequency of transient sphincter relaxation (21, 22). All these factors can lead to increased esophageal acid exposure. In a retrospective analysis of 1,389 patients who had an upper endoscopy, excessive body weight was a significant independent risk factor for the presence of a hiatal hernia. Hiatal hernia is a significant risk factor for developing esophagitis (23). This study also showed that BMI is significantly associated with esophagitis largely through an increased incidence of hiatal hernia. In another study, an increase in BMI was associated with an increased risk for developing erosive esophagitis (24). Furthermore, obese patients (BMI ≥30) have been demonstrated to have a higher prevalence of erosive esophagitis (26.5%) compared to people with a normal weight (9.3%) (25).
Although several studies suggest that obesity is a risk factor for developing erosive esophagitis in Western GERD patients, there is a controversy over the role of obesity as a risk factor for developing erosive esophagitis in Asian countries. In the metaanalysis by Corley et al., there was an association between BMI and GERD in the United States but not in Asia (26). However, the life style of Koreans is becoming increasingly westernized. In a recent nationwide multicenter study in Korea, the significant risk factors for developing erosive esophagitis using a multivariate analysis included: male gender, regular alcohol consumption, BMI >25, hiatal hernia, and a history of H. pylori eradication (27). These results suggest that physical factors effect lower esophageal pressure or acid secretion are risk factors for developing erosive esophagitis. These findings differ from those of our study with respect to some points. In our study, erosive esophagitis group had a higher BMI and more current alcoholics, but these factors were not associated with erosive esophagitis in the multiple-adjustment model. In addition, different risk factors for developing erosive esophagitis and NERD have been reported in Japan. This supports the hypothesis that the pathogenesis for these two categories of GERD is different. Fujiwara et al. showed that female gender, low BMI, no smoking, absence of a hiatal hernia, and the severity of gastric atrophy were positively associated with NERD compared to erosive esophagitis among Japanese patients (13).
In our study, obesity-related factors such as BMI, OD, and WHR were all related to the development of erosive esophagitis. However, only WHR was significantly associated with an increased risk in the multiple-adjustment model. This suggests that a pattern of obesity could be more closely related to the development of erosive esophagitis. WHR is a tool for measuring abdominal obesity. We measured WHR automatically using a body composition analyzer device. In this study, abdominal obesity was a more significant risk factor for developing erosive esophagitis compared to BMI or OD. Visceral abdominal fat is metabolically active and has been closely associated with elevated serum levels of interleukin-6 and tumor necrosis factor-α (28-30). These cytokines are pro-inflammatory and have been shown in multiple studies to be over-expressed in patients with erosive esophagitis. Humoral factors, such as insulin and leptin, as well as growth factors or hormonal factors, such as estrogen related to adiposity, may also affect the risk for developing GERD.
The present study has limitations due to its cross sectional nature and the fact that it was conducted over a short period. Additionally, this study was conducted at only one center, which may limit the generalization. And the possibility of selection biases may be present as this study included the patients who underwent an upper endoscopy for a voluntary health check-up. The participants were interested in health and they were mostly well-off rich people. The patients with severe symptoms or economically poor populations were not included in this study. Moreover, data collected in this study did not include information on risk factors such as dietary composition, physical activity and life style, which are necessary to explain the similarity and differences in the clinical characteristics between Korean population and those in Western countries.
The clinical characteristics of the NERD and erosive esophagitis groups in the Korean population of this study were found to differ. These characteristics were similar to those seen in Western GERD patients. We demonstrated that male gender, high BMI, high OD, high WHR, high TG, alcohol intake, smoking, and presence of a hiatal hernia were positively related to the development of erosive esophagitis compared to NERD among Korean patients. The associations of male gender, high WHR, and presence of a hiatal hernia with the risk of developing erosive esophagitis persisted despite adjustments for gender, BMI, OD, WHR, TG, alcohol consumption, smoking, and hiatal hernia. This study found that obesity was associated with the increased risk of developing erosive esophagitis. This risk was specifically associated with increased abdominal obesity as measured by the WHR. Our study suggests that the pattern of obesity may be more important than BMI or OD. Further studies are needed to identify the possible mechanism by which abdominal fat increases the risk for developing erosive esophagitis.
Figures and Tables
References
1. Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Prevalence of gastro-oesophageal reflux symptoms and influence of age and sex. Scand J Gastroenterol. 2004. 39:1040–1045.
2. Bollschweiler E, Knoppe K, Wolfgarten E, Hölscher AH. Prevalence of reflux symptoms in the general population of Cologne. Z Gastroenterol. 2007. 45:177–181.
3. Wong WM, Lai KC, Lam KF, Hui WM, Hu WH, Lam CL, Xia HH, Huang JQ, Chan CK, Lam SK, Wong BC. Prevalence, clinical spectrum and health care utilization of gastro-esophageal reflux disease in a Chinese population: a population-based study. Aliment Pharmacol Ther. 2003. 18:595–604.
4. Fujiwara Y, Higuchi K, Watanabe Y, Shiba M, Watanabe T, Tominaga K, Oshitani N, Matsumoto T, Nishikawa H, Arakawa T. Prevalence of gastroesophageal reflux disease and gastroesophageal reflux symptoms in Japan. J Gastroenterol Hepatol. 2005. 20:26–29.
5. Cho YS, Choi MG, Jeong JJ, Chung WC, Lee IS, Kim SW, Han SW, Choi KY, Chung IS. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005. 100:747–753.

6. Howard PJ, Maher L, Pryde A, Heading RC. Symptomatic gastro-oesophageal reflux, abnormal oesophageal acid exposure, and mucosal acid sensitivity are three separate, though related, aspects of gastro-oesophageal reflux disease. Gut. 1991. 32:128–132.

7. Baldi F, Ferrarini F, Longanesi A, Ragazzini M, Barbara L. Acid gastroesophageal reflux and symptom occurrence. Analysis of some factors influencing their association. Dig Dis Sci. 1989. 34:1890–1893.
8. Weusten BL, Akkermans LM, vanBerge-Henegouwen GP, Smout AJ. Symptom, perception in gastroesophageal reflux disease is dependent on spatiotemporal reflux characteristics. Gastroenterology. 1995. 108:1739–1744.

9. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005. 54:710–717.

10. Jones RH, Hungin AP, Philips J. Gastro-oesophageal reflux disease in primary care in Europe: Clinical presentation and endoscopic findings. Eur J Gen Pract. 1995. 1:149–154.

11. Carlsson R, Dent J, Watts R, Riley S, Sheikh R, Hatlebakk J, Haug K, de Groot G, van Oudvorst A, Dalvag A, Junghard O, Wiklund I. International GORD Study Group. Gastro-oesophageal reflux disease in primary care: an international study of different treatment strategies with omeprazole. Eur J Gastroenterol Hepatol. 1998. 10:119–124.
12. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus paper. Z Gastroenterol. 2007. 45:1125–1140.
13. Fujiwara Y, Higuchi K, Shiba M, Yamamori K, Watanabe Y, Sasaki E, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am J Gastroenterol. 2005. 100:754–758.

14. Nakamura T, Shirakawa K, Masuyama H, Sugaya H, Hiraishi H, Terano A. Minimal change oesophagitis: a disease with characteristic differences to erosive oesophagitis. Aliment Pharmacol Ther. 2005. 21:Suppl 2. 19–26.

15. Mishima I, Adachi K, Arima N, Amano K, Takashima T, Moritani M, Furuta K, Kinoshita Y. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese. Scand J Gastroenterol. 2005. 40:1005–1009.

16. Wu JC, Cheung CM, Wong VW, Sung JJ. Distinct clinical characteristics between patients with nonerosive reflux disease and those with reflux esophagitis. Clin Gastroenterol Hepatol. 2007. 5:690–695.

17. Hiyama T, Yoshihara M, Tanaka S, Haruma K, Chayama K. Strategy for treatment of nonerosive reflux disease in Asia. World J Gastroenterol. 2008. 14:3123–3128.

18. Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007. 41:131–137.
19. Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD. Gastro-oesophageal reflux disease in obesity: pathophysiological and therapeutic considerations. Obes Rev. 2002. 3:9–15.

20. Maddox A, Horowitz M, Wishart J, Collins P. Gastric and oesophageal emptying in obesity. Scand J Gastroenterol. 1989. 24:593–598.

21. O'Brien TF Jr. Lower esophageal sphincter pressure (LESP) and esophageal function in obese humans. J Clin Gastroenterol. 1980. 2:145–148.
22. Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001. 111:Suppl 8A. S174–S177.

23. Wilson LJ, Ma W, Hirschowitz BI. Association of obesity with hiatal hernia and esophagitis. Am J Gastroenterol. 1999. 94:2840–2844.

24. Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk of gastroesophageal reflux disease and its complications. Ann Intern Med. 2005. 143:199–211.
25. Aro P, Ronkainen J, Talley NJ, Storskrubb T, Bolling-Sternevald E, Agréus L. Body mass index and chronic unexplained gastrointestinal symptoms: an adult endoscopic population based study. Gut. 2005. 54:1377–1383.

26. Corley DA, Kubo A, Zhao W. Abdominal obesity, ethnicity, and gastroesophageal reflux symptoms. Gut. 2007. 56:756–762.
27. Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS, Rew JS, Moon JS, Kim S, Park SH, Jung HC, Chung IS. H. pylori and Gerd Study group of Korean College of Helicobacter and upper gastrointestinal research. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008. 27:173–185.

28. Weinsier RL, Hunter GR, Gower BA, Schutz Y, Darnell BE, Zuckerman PA. Body fat distribution in white and black women: different patterns of intraabdominal and subcutaneous abdominal adipose tissue utilization with weight loss. Am J Clin Nutr. 2001. 74:631–636.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download