Abstract
The purpose of our study was to evaluate the characteristics and the changes of low vision patients over ten years in Korea, and to establish useful data for planning low vision services, active care and rehabilitation. We conducted a retrospective study of 681 low vision patients who visited two low vision clinics in Seoul from 1995 to 2008. Age and sex distribution, cause of low vision, type of prescribed low vision aids, and changes of the characteristics were reviewed. In result, male were more than female. The age group between 11 and 20-yr-old (18.1%) was the largest age group. Optic atrophy (28.3%) was main causes of low vision. However, elderly low vision patients is increasing and macular degeneration is becoming a leading cause of low vision (P<0.05). One thousand five low vision aids (LVAs) were prescribed for 681 patients (1.46±0.62 aids for each patient). Near LVAs were prescribed more than distance LVAs. In most patients, the use of LVAs improved both near and distance visual function. This study is the first survey of a large number of low vision patients over a ten year period in Korea. On the base of this study, the planning of low vision services and more active rehabilitation for low vision patients, especially elderly patients, need in Korea.
According to a World Health Organization (WHO) consultation report, person with low vision is someone who has: an impairment of visual function, even after treatment or refractive correction; a visual acuity of less than 6/18 (20/60) to perception of light or a visual field of less than 10° in the better eye, but who uses, or is potentially able to use, vision for the planning and/or execution of a task (1). Low vision is one of the priorities in the global initiative, VISION 2020-The Right to Sight, along with cataract, trachoma, onchocerciasis, childhood blindness, and refractive error (2). In Korea, there are 216,881 patients on record as having visual impairment which includes low vision and binocular or monocular blindness (3). However, there has not been any clinical data collected from the large number of low vision patients in Korea. It is important to collect and analyze data from low vision patients in order to offer low vision care. Therefore, we investigated characteristics of low vision patients such as age and sex distribution, cause of low vision, type of prescribed low vision aids, and changes of the characteristics over a ten year period in Korea. We expect these data can be useful for planning low vision services, active care and rehabilitation.
We reviewed the medical records of 681 patients who visited the low vision clinic at either the National Medical Center or Chung-Ang University Hospital in Seoul, Korea, more than twice between May 1995 and December 2008.
At the initial visit, a detailed past medical history was obtained for each patient, and ocular examinations were performed. Ocular examinations included: measurement of visual acuity (VA); assessment of pupillary reaction; measurement of intraocular pressure (IOP) using Goldmann applanation tonometry; slitlamp biomicroscopic examination; fundus examination (with an indirect ophthalmoscope using a 20-diopter lens and with a slit lamp using a 90-diopter lens) after dilatation, unless contraindicated because of the risk of angle closure; color vision test; contrast sensitivity test; and visual field screening using the Humphrey Automated Field Analyzer (Swedish Interactive Thresholding Algorithm Standard 24-2). In addition, a visual evoked potential test and electroretinography were carried out in accordance with the cause of low vision. Distance and near VA were first measured for each eye without refractive correction using the Dr. Han's standard test chart at a distance of 5 m and a Light-house near chart at a distance of 40 cm under illumination from a 600 to 700 lux light source. The examination was repeated with full correction of refractive errors to obtain the distance and near best-corrected visual acuity (BCVA). If a patient's distance BCVA was under 20/200, the VA was measured using the Finebloom chart or low vision letter chart. On a second visit one to two weeks from the date of the initial visit, each patient was made to practice with more than two low vision aids (LVAs) for distance and near vision, in accordance with his or her test results and the daily activity that he or she wanted to achieve in the future. On the third visit, we prescribed the LVAs that were the easiest and most comfortable for the patient to use. Each patient revisited the clinic after one month, whereupon we determined if the LVA met his or her needs.
In order to investigate changes in the characteristics of low vision patients over time, we compared the data of 350 patients including age, the cause of low vision, and the prescription of LVAs from May 1995 to April 1999 with those of 331 patients from May 1999 to December 2008.
Statistical Package for the Social Sciences (SPSS) software program, version 16.0 (SPSS Inc., Chicago, IL, USA.), and results were considered statistically significant when the P value was <0.05.
Our study was approved by the Institutional Review Board of Chung-Ang University College of Medicine (IRB No. C2009091 [278]).
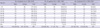
There were 440 (64.6%) men and 241 (35.4%) women, with an age range of 5 to 90 yr (mean age of 33.8 yr) included in this study. The largest age group was those between 10 and 19 yr of age (20.4%), followed by that between 20 and 29 yr of age (16.4%), and below 10 years of age (16%) (Table 1). When comparing the data from May 1995 to April 1999 with that from May 1999 to December 2008, the proportion of low vision patients under 20-yr-old decreased (43.1% to 20.9%) (Pearson's chi-square test, P<0.05). And the proportion of low vision patients over 60-yr-old increased (12.6% to 26.3%) significantly (Pearson's chi-square test, P<0.05). With regard to sex distribution, the proportion of women increased (31.7% to 39.3%) significantly. (Pearson's chi-square test, P<0.05)
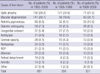
The most common cause of low vision was optic nerve atrophy (28.3%), followed by macular degeneration (20.8%). When comparing the data from 1995 to 1999 with those from 1999 to 2008, the proportion of optic atrophy, congenital cataract, and amblyopia decreased more than 1%, while the proportion of macular degeneration, diabetic retinopathy, and other diseases increased (Table 2).
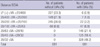
One thousand five LVAs were prescribed for 681 patients (1.46±0.62 aids for each patient) (Table 3). Among these, LVAs for near vision (39.2%, 394 aids) were prescribed more than LVAs for distance vision (60.8%, 611 aids). When comparing the data from 1995 to 1999 with those from 1999 to December 2008, the number of prescribed LVAs for each patient showed a significant increase (1.32±0.53 aids per patient to 1.64±0.77 aids per patient) (paired t-test, P<0.05). The prescribed proportion of telescope and spectacle-type LVAs decreased and that of magnifier LVAs increased. The prescription of prism lenses and electric LVAs including EYE FINE® (Nittoh & Kogaku, Nagano, Japan) and PocketViewer® (HumanWare, Christ Church, New Zealand) began in 2000.
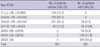
Before the use of LVAs, distance BCVA was typically worse than 20/100 (91.2%). There were 245 (36.0%) patients whose distance BCVA was between 20/200 and 20/100 (the largest group). After the use of LVAs, distance BCVA was typically better than 20/63 (88.2%), and there were 328 (48.2%) patients whose distance BCVA was better than 20/32 (the most prevalent group) (Table 4).
Near BCVA was also typically worse than 20/100 (88.0%), and there were 267 (39.2%) patients whose near BCVA was between 20/200 and 20/100 (the largest group) prior to the use of LVAs. After the use of LVAs, near BCVA was typically better than 20/63 (82.1%), and there were 376 (55.2%) patients whose near BCVA was better than 20/32 (the most prevalent group) (Table 5).
Low vision is a very important public health problem. Previous worldwide population-based studies have demonstrated consistently that the prevalence of low vision has been increasing significantly and that most low vision patients are elderly (4). In contrast, young patients accounted for a large proportion of the low vision patients (46.8% under 30-yr-old) in this study. This is possibly because low vision clinics and care have been largely unknown to the elderly and there are many young low vision patients detected from vision tests in schools. However, when comparing the data from May 1995 to April 1999 with those from May 1999 to December 2008, the proportion of low vision young patients, especially those under 20-yr-old, showed a significant decrease and the proportion of low vision elderly patients showed an obvious increase. An increasingly older population, increasing attention on the health, increasing social behaviors, and increasing concern and publicity regarding low vision are possible reasons for this changed trend. The increased number of low vision clinics (there are presently 11 low vision clinics in Korea) likely explains the decrease in the number of low vision patients from 1999 to 2008 compared to that of 1995 to 1999 in this study.
Concerning the causes of low vision, in this study, the most common cause was optic nerve atrophy, which is consistent with other low vision reports in Korea (5). However, since 1999, the most common cause of low vision has been macular degeneration including age-related macular degeneration and diabetic retinopathy which showed increased proportions. This may be related to the increase in elderly low vision patients. As congenital cataract, amblyopia, and corneal opacity are preventable with early treatment, the proportion of these low vision causes has decreased and may decrease further. The reason why other causes of low vision have increased is likely because unexplained optic atrophy or retinal degeneration have been more readily identified with advanced diagnostic methods.
Most low vision aids are used for near vision, and it is important to consider a patient's working distance and purposes when prescribing LVAs (6-8). So near LVAs like magnifiers and spectacle-type aids were more prescribed than distance LVAs like telescopes. This suggests that near vision activities, such as reading, have been more important for low vision patients. Recently, EYE FINE® (Nitto & Kogaku), which has an advantage of usability in both near and distance viewing by auto-focusing according to working distance and PocketViewer® (HumanWare), a compact portable hand-held electric magnifier, have been developed and put to use. These electric LVAs have been used by low vision patients since 2000. Prism lenses have been also used recently for eccentric viewing, visual field shift, or field expansion.
Although the detailed data were not shown in this paper, there were more prescribed LVAs in each cause of low vision. For example brown or pink colored tinted glasses and bifocal lens were used for albinism. But the kind of prescribed LVAs are mostly dependent upon visual function of each patient, not the causes of low vision. So each visual function should be considered first when prescribing the LVAs.
In most patients, both near and distance BCVA were much improved when using the LVAs. This suggests that LVAs are effective in the improvement of visual function.
In summary, although young patients still represent the majority of patients visiting the low vision clinics, we found that the number of elderly low vision patients is increasing and macular degeneration is becoming a leading cause of low vision. Rehabilitation using LVAs has improved the visual function of low vision patients. However, rehabilitation with LVAs is not yet sufficient in low vision patients. Even if this study does not fully represent the characteristics of all low vision patients in Korea, it is the first survey for a large number of low vision patients over ten years in Korea. We believe that more active care and rehabilitation of low vision patients, especially elderly patients, are important and need in Korea and that this study will help in the planning of low vision services in Korea.
Figures and Tables
ACKNOWLEDGMENTS
We would like to thank Jong Hwa Park, MD and the optometrists at Chung-Ang University Hospital for their comments and help with data collection.
References
1. World Health Organization. WHO/PBL/93.27. The Management of Low Vision in Children. Report of a WHO Consultation: Bangkok, July 1992. 1993. Geneva: World Health Organization.
2. World Health Organization. WHO/PBL/97.61. Global Initiative for the Elimination of Avoidable Blindness. 1997. Geneva: World Health Organization.
3. Ministry for Health, Welfare and Family Affairs. The Yearbook of Ministry for Health Welfare and Family Affairs Statics. 2008. 232.
4. Congdon N, O'Colmain B, Klaver CC, Klein R, Muñoz B, Friedman DS, Kempen J, Taylor HR, Mitchell P. Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004. 122:477–485.
6. Hyman L, Wu SY, Connell AM, Schachat A, Nemesure B, Hennis A, Leske MC. Prevalence and causes of visual impairment in the Barbados Eye Study. Ophthalmology. 2001. 108:1751–1756.
7. Michon JJ, Lau J, Chan WS, Ellwein LB. Prevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderly. Br J Ophthalmol. 2002. 86:133–139.

8. Moser CL, Martin-Baranera M, Vega F, Draper V, Gutiérrez J, Mas J. Survey of blindness and visual impairment in Bioko, Equatorial Guinea. Br J Ophthalmol. 2002. 86:257–260.

9. Tielsch JM, Sommer A, Witt K, Katz J, Royall RM. Blindness and visual impairment in an American urban population. The Baltimore Eye Survey. Arch Ophthalmol. 1990. 108:286–290.
10. Klein R, Klein BE, Linton KL, De Mets DL. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991. 98:1310–1315.

11. Baasanhu J, Johnson GJ, Burendei G, Minassian DC. Prevalence and causes of blindness and visual impairment in Mongolia: a survey of populations aged 40 years and older. Bull World Health Organ. 1994. 72:771–776.
12. Attebo K, Mitchell P, Smith W. Visual acuity and the causes of visual loss in Australia. The Blue Mountains Eye Study. Ophthalmology. 1996. 103:357–364.
13. Taylor HR, Livingston PM, Stanislavsky YL, McCarty CA. Visual impairment in Australia: distance visual acuity, near vision, and visual field findings of the Melbourne Visual Impairment Project. Am J Ophthalmol. 1997. 123:328–337.

14. Rubin GS, West SK, Munoz B, Bandeen-Roche K, Zeger S, Schein O, Fried LP. A comprehensive assessment of visual impairment in a population of older Americans. The SEE Study. Salisbury Eye Evaluation Project. Invest Ophthalmol Vis Sci. 1997. 38:557–568.
15. Klaver CC, Wolfs RC, Vingerling JR, Hofman A, de Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol. 1998. 116:653–658.
16. Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN, John RK, McCarty CA, Rao GN. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci. 2001. 42:908–916.
17. VanNewkirk MR, Weih L, McCarty CA, Taylor HR. Cause-specific prevalence of bilateral visual impairment in Victoria, Australia: the Visual Impairment Project. Ophthalmology. 2001. 108:960–967.
18. Liu JH, Cheng CY, Chen SJ, Lee FL. Visual impairment in a Taiwanese population: prevalence, causes, and socioeconomic factors. Ophthalmic Epidemiol. 2001. 8:339–350.

19. Murthy GV, Gupta S, Ellwein LB, Munoz SR, Bachani D, Dada VK. A population-based eye survey of older adults in a rural district of Rajasthan: I. Central vision impairment, blindness, and cataract surgery. Ophthalmology. 2001. 108:679–685.
20. Munoz B, West SK, Rodriguez J, Sanchez R, Broman AT, Snyder R, Klein R. Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002. 43:608–614.
21. Buch H, Vinding T, La Cour M, Appleyard M, Jensen GB, Nielsen NV. Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology. 2004. 111:53–61.
22. Dandona R, Dandona L, Srinivas M, Giridhar P, Nutheti R, Rao GN. Planning low vision services in India: a population-based perspective. Ophthalmology. 2002. 109:1871–1878.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download