Abstract
We investigated the risk factors for resistance to ciprofloxacin, cefazolin, ampicillin and co-trimoxazole in Escherichia coli isolates from urine of Korean female patients with acute uncomplicated cystitis (AUC). A total of 225 patients and their E. coli isolates were prospectively and nationwidely enrolled between May and October, 2006. All the antimicrobials did not show any differences according to the age group. A higher rate of ciprofloxacin resistance was observed in the south (OR: 3.04, 95% CI: 1.19-7.80 for Chungcheong-do & Jeolla-do; OR: 3.04, 95% CI: 1.22-7.58 for Gyeongsang-do) compared to Gyeonggi-do. Two recurrences of AUC in the past year was an important risk factor for antimicrobial resistance (ciprofloxacin; OR: 6.71, 95% CI: 1.86-24.11 and cefazolin; OR: 5.72, 95% CI: 1.20-27.25). However, the resistance to co-trimoxazole and ampicillin was not associated with any of the risk factors. This study also revealed the pattern of multi-drugs resistance in ciprofloxacin resistant E. coli strains. In conclusion, for Korean patients with two more recurrences of AUC in the past year, it is strongly recommended to perform an antimicrobial sensitivity test with a urine sample before empirical treatment.
Acute uncomplicated cystitis (AUC) is the most commonly encountered bacterial infections in healthy women. The current management of AUC is usually a short course of empirical treatment with co-trimoxazole or fluoroquinolones in areas where resistance to co-trimoxazole is prevalent. This antibiotics are tried without performing a urine culture or susceptibility testing to guide therapy (1). However, there has been a significant increase in resistance of Escherichia coli strains to antimicrobials worldwide (2-8). The adverse consequences of using antimicrobials to treat a strain that is resistant to these antimicrobials may be a delay in resolution of the infection and the consequently increased social costs such as days lost from work or school for some women (9).
Fluoroquinolone or co-trimoxazole resistance by E. coli has been detected at a high rate in the Asia-Pacific region in recent years (2-5). Moreover, some countries in Asia do not currently consider fluoroquinolone as a first line treatment for recurrent cystitis (3, 6). Consequently, new therapeutic options in the setting of high resistance against fluroquinolone need to be found. Therefore, the clinicians in local areas, before deciding on the best empirical regimen to use for AUC in this era of increased drug resistance, they must know the patterns of drug resistance and assess the risk factors for drug resistance in their local area. However, there are not many studies on the drug resistance pattern of AUC in Korea (2, 3). The designs of the previously reported papers in Korea were retrospective studies and they were regionally confined as well. Additionally, the available studies were also a mix of data from patients with uncomplicated and complicated cystitis. Further, much of the data about antimicrobial resistance has often have come from western countries. Unfortunately, this western data may not accurately reflect the drug resistance patterns in Asia because the patterns may be different among different countries (2, 5, 6).
In this study, we described the four key antimicrobials susceptibility patterns of the E. coli strains from AUC patients who were prospectively collected from 22 different medical centers in Korea. We also assessed the risk factors for antimicrobial-resistant uropathogenic E. coli, and particularly their associations with fluoroquinolone resistance.
All the female patients between 18 and 65 yr old and who presented with symptoms of dysuria, urgency, frequency or a combination of these between May and October, 2006 were included in this study. The exclusion criteria were symptoms of or predisposing factors for complicated cystitis. The women who had received antimicrobial agents in the 4 weeks previous to the study and those who were hospitalized were also excluded. A clean-catch midstream urine sample was tested by microscopy for the presence of leukocytes, and then it was sent to a central laboratory for culture and sensitivity testing. Only one specimen per patient was examined. No mixed infections were included. The E. coli included in the study were from cultures yielding ≥103 colony forming units/mL and the urine displayed pyuria (2).
In total, 225 E. coli isolates were prospectively and consecutively collected from the urine samples of the female outpatients with uncomplicated cystitis in 22 hospitals of Korea. In Seoul, 62 samples were collected from 9 hospitals. In Gyeonggi-do, 102 samples were collected from 4 hospitals. In Chungcheong-do and Jeolla-do, 31 samples were collected from 5 hospitals. In Gyeongsang-do, 30 samples were collected from 4 hospitals.
The minimum inhibitory concentration (MIC) of ciprofloxacin resistance was determined by the agar dilution method on Mueller-Hinton agar (Becton Dickinson and Company, Franklin Lakes, NJ, USA), as recommended by the NCCLS (3). The number of cystitis episodes was classified into none, one and two recurrences in the previous year (2).
For easily handling of the data, we placed the intermediate resistant E. coli isolates into the resistant categories of each antimicrobial. This study was approved by the institutional review board of the Dankook University Medical Center (approval number: 0911-078).
Statistical analysis was performed by using Fisher's exact test, chi-square tests, Student's t-tests and the Mann-Whitney test. Multiple variables were assessed as predictors of the categorical outcomes by multivariable logistic regression analysis. P values ≤0.05 were considered statistically significant.
Determination of antimicrobials resistance was possible for more than 96.9% of the isolates (220 isolates to ampicillin, 221 to co-trimoxazole and ciprofloxacin and 218 to cefazolin of the total 225 isolates). The E. coli isolates more commonly exhibited resistance to ampicillin (66.3%) and co-trimoxazole (31.2%), followed by ciprofloxacin (26.7%) and cefazolin (7.3%).
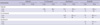
The association studies of the risk factors for antimicrobials resistance are shown in Table 1. The mean ages of the patients with sensitive and resistant isolates to ampicillin were 45.06±12.41 and 46.54±12.41 yr, respectively (P=0.40), those for co-trimoxazole were 45.30±12.38 and 47.37±12.66 yr (P=0.251), those for ciprofloxacin were 45.47±12.70 and 47.03±11.94 yr (P=0.42) and those for cefazolin were 45.85±12.42 and 48.87±13.14 yr (P=0.353), respectively. In the women aged older than 50 yr, the resistance rates to the four antimicrobials were not increased as compared to the women below that age (Table 1).
Some regional differences in ciprofloxacin resistance were shown. Of the E. coli isolates from Gyeongsang-do, 38.7% were ciprofloxacin resistant strains, whereas 20.6% of the E. coli isolates from Gyeonggi-do were ciprofloxacin resistant strains (OR: 2.43, 95% CI: 1.02-5.8, P=0.04). However, there were no significant differences in ciprofloxacin resistance among Seoul and the Chungcheong-do & Jeolla-do and Gyeongsang-do. In addition, there were no statistical differences in co-trimoxazole, ampicillin and cefazolin resistance among the four regions. Interestingly, two recurrences of ACU in prior year was associated with ciprofloxacin (OR: 4.44, 95% CI: 1.34-14.74, P=0.01) and cefazolin resistance (OR: 5.33, 95% CI: 1.24-22.84, P=0.02). One recurrence in previous year was not related with the antimicrobials resistance.
We analyzed trends for the risk of resistance to the four antimicrobials by performing multivariate analysis (Table 2). Resistance to the four antimicrobials did not vary greatly according to age group. However, the samples from the south-west (Chungcheong-do & Jeolla-do; OR: 3.04, 95% CI: 1.19-7.80, P=0.02), and from the south-east (Gyeongsang-do; OR: 3.04, 95% CI: 1.22-7.58, P=0.017) showed a risk for ciprofloxacin resistance when compared with the samples from the north (Gyeonggi-do), whereas the other antimicrobials did not reveal differences according to the different region. In addition, the patients with ciprofloxacin or cefazolin resistant E. coli isolates were significantly more likely to have histories of cystitis (two recurrences with ciprofloxacin resistant E. coli; OR: 6.71, 95% CI: 1.86-24.11, P=0.004 and two recurrences with cefazolin resistant E. coli; OR: 5.72, 95% CI: 1.20-27.25, P=0.028) in previous year as compared with the non-recurrent patients.
Resistance to one antimicrobial was usually associated with resistance to another antimicrobial (Table 3). For example, the E. coli strains with ciprofloxacin resistance were significantly associated with resistance to ampicillin (P<0.001), co-trimoxazole (P<0.001) and cefazolin (P=0.002).
The Korean Association of Urogenital Tract Infection and Inflammation (KAUTII) reported previously that the resistance rates of E. coli from AUC patients to ciprofloxacin, cefazolin, ampicillin and co-trimoxazole were 23.4%, 7.6%, 64.8 and 29.4%, respectively (2). They also reported that Gyeongsang-do showed a trend for a higher rate of resistance to ciprofloxacin as compared with other regions (2). We have recently re-evaluated the raw data and re-analyzed the data together with the patient characteristics to investigate the overall patterns and risk factors for resistance to ciprofloxacin, cefazolin, ampicillin and co-trimoxazole in the E. coli isolates from patients with AUC.
Interestingly, resistance to ampicillin, co-trimoxazole, cefazolin and ciprofloxacin did not significantly vary according to age group. However, it is a general rule that older aged patients are significantly associated with antimicrobial resistance. Moreover, some studies have also reported that older women with AUC show a higher chance for ciprofloxacin resistant E. coli than do the younger women (4, 6, 7). However, the four key antimicrobials did not show any differences in their resistance by age group in our study. There are some possible reasons for this difference between our study and our studies. First of all, we applied very strict criteria for selecting AUC patients. The exclusion criteria were patients with symptoms of or predisposing factors for complicated urinary tract infections, such as pregnancy, antimicrobial treatment within 2 weeks, symptoms lasting longer than 7 days, fever, known urological or nephrological problems and more than 3 recurrences in previous year (2). In addition, all the female patients in our study were between 18 and 65 yr old (mean±SD: 45.93±12.47 yr). The patients whose ages were over 66 were not included because of the risk of complicated cystitis. We also dichotomized patient age into 18-49 yr olds and 50-65 yr old, and re-analyzed the data. Clearly, the patient ages were not different in the dichotomized study.
The antimicrobial resistance was evaluated according to four geographic regions in Korea. Seoul is a big metropolitan city. Gyeonggi-do is also an urban area that surrounds Seoul. Chungcheong and Jeolla-do is in the south-west and Gyeongsang-do is in the south-east. Near all the hospitals included in this study are tertiary university hospitals, and the estimated populations around the hospitals are above a half million. There was no difference in the age factor among the four provinces. In addition, there was no statistical difference in ciprofloxacin resistance among 4 hospitals in Gyeonggi-do (P=0.2). Gyeongsang-do, Chungcheong-do and Jeolla-do revealed a significantly higher rate of ciprofloxacin resistance when compared with that of Gyeonggi-do (Table 2). Although previous use of antimicrobials may be involved in the regional differences of antimicrobial resistance, we must consider other factors such as the patients' characteristics or sampling bias and the social and geological factors that have not yet been defined.
A history of AUC in the previous 1 yr was the other independent variable for ciprofloxacin or cefazolin resistance. For the case of ciprofloxacin resistance, the results of our study were not surprising because fluoroquinolones has been prescribed empirically and habitually in this region over the past decade. In addition, an association between the increase in fluoroquinolones prescriptions and an increase in its resistance has been reported in several countries (8, 10, 11).
The risk of cefazolin resistance was also increased in E. coli isolates from patients with two bouts of recurrent AUC in past year. Although all the previous prescriptions for the patients were not analyzed, the first generation cephalosporins have rarely been used to empirically treat AUC in Korea. Moreover, a small decrease in cefazolin resistance was recognized in 2006 (7.6%) when compared with the same study in 2002 by KAUTII (7.8%) (2, 3). If previous exposure to cefazolin was an important factor for resistance in our study, it is reasonable to consider that the prevalence of cefazolin resistance will increase year by year.
The risk of cephalosporin resistance in the E. coli isolates from AUC patients has not been well documented around the world. However, to the best of our knowledge, many doctors may consider that the risk of cephalosporin resistance in the E. coli isolates from AUC patients is not high. The finding that the E. coli isolates from patients with recurrent AUC have a trend for cefazolin resistance is clinically very important because cephalosporins are considered as an empirical treatment for urinary tract infections in countries with a high prevalence of fluoroquinolones resistance.
E. coli strains with ciprofloxacin resistance were also significantly associated with resistance to ampicillin, co-trimoxazole, and cefazolin in our study.
Quinolone resistance is often associated with cross-resistance to many other structurally unrelated antimicrobials such as beta-lactams, puromycin, tetracyclines, nalidixic acid and chloramphenicol (12, 14). Its mechanism of the cross-resistance has not been clearly understood. Combinations of mutation in the topoisomerase-encoding genes, altered permeability and active efflux have been suggested as mechanisms. Altered permeability and active efflux would also contribute to the decreased susceptibility to beta-lactams (15).
Fluoroquinolones have a broad spectrum antibiotic for Gram positive and Gram negative bacteria. They are also convenient for oral intake and have few side effects. With these advantages, the empirical treatment with fluoroquinolones has been a standard treatment for urinary tract infections in Korea. Concurrently and perhaps consequently, urinary tract infections due to fluoroquinolones-resistant E. coli strains have continued to increase at an alarming rate. However, there are very few choices to replace fluoroquinolone for empirical AUC treatment. Clearly, we should make a plan to reduce the antimicrobials resistance and be more cautious in using antimicrobials for AUC treatment in Korea, especially fluoroquinolone. Therefore, urine culture and antimicrobial susceptibility testing should be considered for the Korean AUC patients who have risk factors for antimicrobial resistance.
Figures and Tables
Table 1
Univariate analysis of risk factors for E. coli resistance to ciprofloxacin, co-trimoxazole, ampicillin and cefazolin

ACKNOWLEDGMENTS
We would like to thank all KAUTII (Korean Association of Urogenital Tract Infection and Inflammation) members who were invited to this study for contributing valuable data and samples.
References
1. Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997. 11:551–581.

2. Kim ME, Ha US, Cho YH. Prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in female outpatients in South Korea: a multicentre study in 2006. Int J Antimicrob Agents. 2008. 31:Suppl 1. S15–S18.

3. Lee SJ, Cho YH, Kim BW, Lee JG, Jung SI, Lee SD, Lee SE, Kim ME, Choi YD, Rim JS, Sim BS, Cho IR, Ryu SB, Kim CS, Kim WJ, Lee TY. A multicenter study of antimicrobial susceptibility of uropathogens causing acute uncomplicated cystitis in woman. Korean J Urol. 2003. 44:697–701.
4. Arslan H, Azap OK, Ergönül O, Timurkaynak F. Urinary Tract Infection Study Group. Risk factors for ciprofloxacin resistance among Escherichia coli strains isolated from community-acquired urinary tract infections in Turkey. J Antimicrob Chemother. 2005. 56:914–918.

5. Akram M, Shahid M, Khan AU. Etiology and antibiotic resistance patterns of community-acquired urinary tract infections in J N M C Hospital Aligarh, India. Ann Clin Microbiol Antimicrob. 2007. 6:4.

6. Gobernado M, Valdés L, Alós JI, García-Rey C, Dal-Ré R, García-de-Lomas J. Spanish Surveillance Group for Urinary Pathogens. Antimicrobial susceptibility of clinical Escherichia coli isolates from uncomplicated cystitis in women over a 1-year period in Spain. Rev Esp Quimioter. 2007. 20:68–76.
7. Gobernado M, Valdés L, Alós JI, Garcia-Rey C, Dal-Ré R, García-de-Lomas J. Spanish Surveillance Group for E. coli Urinary Pathogens. Quinolone resistance in female outpatient urinary tract isolates of Escherichia coli: age-related differences. Rev Esp Quimioter. 2007. 20:206–210.
8. Hillier S, Roberts Z, Dunstan F, Butler C, Howard A, Palmer S. Prior antibiotics and risk of antibiotic-resistant community-acquired urinary tract infection: a case-control study. J Antimicrob Chemother. 2007. 60:92–99.

9. Butler CC, Hillier S, Roberts Z, Dunstan F, Howard A, Palmer S. Antibiotic-resistant infections in primary care are symptomatic for longer and increase workload: outcomes for patients with E. coli UTIs. Br J Gen Pract. 2006. 56:686–692.
10. Goettsch W, van Pelt W, Nagelkerke N, Hendrix MG, Buiting AG, Petit PL, Sabbe LJ, van Griethuysen AJ, de Neeling AJ. Increasing resistance to fluoroquinolones in Escherichia coli from urinary tract infections in the Netherlands. J Antimicrob Chemother. 2000. 46:223–228.

11. Steinke DT, Seaton RA, Phillips G, MacDonald TM, Davey PG. Prior trimethoprim use and trimethoprim-resistant urinary tract infection: a nested case-control study with multivariate analysis for other risk factors. J Antimicrob Chemother. 2001. 47:781–787.

12. Kahlmeter G, Menday P, Cars O. Non-hospital antimicrobial usage and resistance in community-acquired Escherichia coli urinary tract infection. J Antimicrob Chemother. 2003. 52:1005–1010.

13. Colgan R, Johnson JR, Kuskowski M, Gupta K. Risk factors for trimethoprim-sulfamethoxazole resistance in patients with acute uncomplicated cystitis. Antimicrob Agents Chemother. 2008. 52:846–851.

14. George AM, Levy SB. Amplifiable resistance to tetracycline, chloramphenicol, and other antibiotics in Escherichia coli: involvement of a non-plasmid-determined efflux of tetracycline. J Bacteriol. 1983. 155:531–540.

15. Miró E, Vergés C, García I, Mirelis B, Navarro F, Coll P, Prats G, Martínez-Martínez L. Resistance to quinolones and beta-lactams in Salmonella enterica due to mutations in topoisomerase-encoding genes, altered cell permeability and expression of an active efflux system. Enferm Infecc Microbiol Clin. 2004. 22:204–211.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download