Abstract
We evaluated the therapeutic effects of tamsulosin for women with non-neurogenic voiding dysfunction. Women who had voiding dysfunctions for at least 3 months were included. Inclusion criteria were age ≥18 yr, International Prostate Symptom Score (IPSS) of ≥15, and maximum flow rate (Qmax) of ≥12 mL/sec and/or postvoid residuals (PVR) of ≥150 mL. Patients with neurogenic voiding dysfunction or anatomical bladder outlet obstruction were excluded. All patients were classified according to the Blaivas-Groutz nomogram as having no or mild obstruction (group A) or moderate or severe obstruction (group B). After 8 weeks of treatment, treatment outcomes and adverse effects were evaluated. One hundred and six patients were evaluable (70 in group A, 36 in group B). After treatments, mean IPSS, bother scores, Qmax, PVR, diurnal and nocturnal micturition frequencies and scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS-SF) were changed significantly. Eighty-nine patients (84%) reported that the treatment was beneficial. The proportion of patients reported that their bladder symptoms caused "moderate to many severe problems" were significantly decreased. No significant difference were observed between the groups in terms of IPSS, bother score, Qmax, PVR, micturition frequency, and BFLUTS-SF changes. Adverse effects related to medication were dizziness (n=3), de novo stress urinary incontinence (SUI) (n=3), aggravation of underlying SUI (n=1), fatigue (n=1). Tamsulosin was found to be effective in female patients with voiding dysfunction regardless of obstruction grade.
α-adrenoceptor (AR) antagonists were first used in the urologic field to treat patients with lower urinary tract symptoms suggestive of benign prostate hyperplasia (BPH). Subsequently, many trials have provided evidence of the efficacy and tolerability of α-AR antagonists in male patients with lower urinary tract symptoms (LUTS). However, although α1-AR antagonist therapy has become an established treatment method for LUTS in men, little is known about its effects in women.
Female voiding dysfunction encompasses those with difficulty emptying the bladder whether due to an inability to contract the detrusor effectively, bladder outflow obstruction, loss of detrusor-sphincter coordination, or a combination of these. The prevalence of voiding phase dysfunction in women has been reported to be 2-25.5% among women referred for the evaluation of lower urinary tract symptoms (1). Moreover, recent studies show that α1-AR antagonists effectively improve symptoms and voiding parameters in women with functional bladder outlet obstruction or detrusor underactivity (2-4). Because α1-ARs appear to play roles in lower urinary tract function at multiple sites and levels, including the bladder neck and external urethral sphincter, and because these non-prostate effects should be gender-independent, it seems logical that α1-AR antagonists could be used in women with voiding dysfunction (5-8). However, little clinical evidence is available to indicate that α1-AR antagonists are effective in female patients with voiding dysfunction. In this study, we evaluated the potential therapeutic effects of α1-AR antagonists using tamsulosin.
Female patients who had suffered from symptoms of voiding dysfunctions for at least 3 months were enrolled in this prospective, open label, multi-center study. The inclusion criteria used were; age ≥18 yr, international prostate symptom score (IPSS) ≥15, and maximum flow rate (Qmax) ≤12 mL/sec and/or postvoid residuals (PVR) ≥150 mL. Patients with possible neurogenic voiding dysfunction or anatomical bladder outlet obstruction (e.g., urethral stricture, bladder neck contracture, bladder calculi, bladder tumor, severe pelvic organ prolapse, previous incontinence surgery, urethral diverticulum, etc.) were excluded. Patients with active urinary tract infection (UTI), history of recurrent UTIs (symptomatic UTIs ≥4 times in the last year), suspected interstitial cystitis, previous surgical procedures related to incontinence or cystocele, medications of alpha-1 blockers and/or anticholinergics within 7 days before the enrollment, estrogen replacement started within 2 months, and the electrostimulation and/or bladder training within the 14 days proceeding the enrollment were excluded from this study. All patients were informed about the study purpose and protocol and provided consents.
A tamsulosin was initiated at 0.2 mg once daily and maintained for 8 weeks. Medications, such as cholinergic drugs (e.g. bethanechol chloride), and other α-AR antagonists, were not permitted throughout the 8 week trial period. Before treatment, all patients underwent an urological evaluation that included medical history taking, pelvic examination, a neurourologic examination, urinalysis, urine culture, and a pressure-flow study (PFS), and all patients maintained a 3-day voiding diary. Urodynamic studies were performed according to the recommendations of the International Continence Society (ICS) (9).
The efficacy analysis included all patients who received at least one dose of study drug, had efficacy data available from the baseline and at least one on-treatment visit, and were compliant with study medication more than 75%. Treatment outcomes were evaluated using IPSS, bother scores, Qmax, PVR, number of micturitions (including 24 hr-, diurnal and nocturnal frequencies), scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS-SF) (10), the patient's perception of bladder condition, and patient's global impression of improvement. The patient's perception of bladder condition was assessed by the use of a six point ordered categorical scale: no problems at all, some very minor problems, some minor problems, (some) moderate problems, severe problems, and many severe problems. The patient's perception of treatment benefit was assessed by the use of an ordered categorical scale. The investigator performed the assessment by questioning the patient in two steps. The first question asked was "Have you had any benefit from your treatment?" with the alternatives for the patient to answer 'yes' or 'no'. If the answer was 'yes', the patient was asked to grade the benefit into 'little benefit' or 'much benefit'. Tolerability was evaluated according to adverse event reports.
The Blaivas-Groutz nomogram was used to grade outflow obstruction (11), and study subjects were divided into two groups according to obstruction severity (Fig. 1). Patients with no or mild obstruction were allocated to group A and those with moderate or severe obstruction to group B. Treatment outcomes of these two groups were compared.
Statistical analyses were performed using the paired t-test for normally distributed data and using the Wilcoxon's signed-ranks test for skewed data to compare pre- to post-treatment changes in the following; IPSS, bother score, Qmax, PVR, micturition frequency, BFLUTS-SF. The Student's t-test was used to compare the results of the two groups at presentation and differences between them when data was normally distributed, and the Mann-Whitney test was used to analyze skewed data. Changes in the patient's perception of bladder condition after treatment were analyzed using non-parametric methods. P values of <0.05 were considered statistically significant.
One hundred and thirteen patients were screened and 106 patients were evaluated after 8 weeks of treatment. Mean patient age was 52.9 yr (range, 21-80 yr). Chief complaints were slow stream (79.3%), increased frequency (70.8%), feeling of incomplete emptying (48.1%), nocturia (34.9%), urgency (32.1%), and abdominal straining (21.7%). Twenty (18.9%) women had mild stress urinary incontinence (SUI). According to the Blaivas-Groutz nomogram, 30 patients had no obstruction (28.3%), 40 mild obstruction (37.7%), 30 moderate obstruction (28.3%), and 6 severe obstruction (5.7%), respectively (Fig. 1).
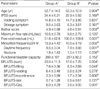
After 8-week of treatment, mean IPSS decreased significantly from 23.9±6.09 to 16.1±8.17 and storage symptoms and voiding symptoms were also improved (Table 1). In 72 patients (67.9%), IPSS decreased by more than 5 points. Bother scores changed significantly as well. Qmax was increased significantly from 10.2±2.79 to 13.5±5.65 and PVR was reduced (P<0.01). Thirty-five (33.0%) patients showed Qmax increases of more than 50%. According to 3-day voiding diaries, total, diurnal and nocturnal micturition frequencies were significantly reduced. However, functional bladder capacities were unchanged (Table 2). BFLUTS-SF total score was significantly decreased from 21.2 to 16.4 (P<0.001) and domain scores of voiding, filling, sexual function and quality of life were also decreased while domain scores of incontinence were not improved significantly (Table 3).
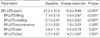
Table 4 shows the baseline parameters of patients in both groups according to the Blaivas-Groutz nomogram. Bother scores, PVR, total and diurnal micturition frequencies and BFLUTS-SF were more severe in patients with no or mild obstruction. Age, IPSS, Qmax, nocturnal micturition frequencies, and functional bladder capacity were not different in the two groups. Comparisons of percentage changes observed for continuous variables of the two groups are shown in Fig. 2. No significant differences between the two groups were observed in terms of changes in IPSS (including voiding and storage scores), bother scores, Qmax, PVR, total, diurnal or nocturnal micturition frequencies and BFLUTS-SF (including sub-domain scores).
In the patient's perception of bladder condition, the proportion of patients who reported that their bladder symptoms caused 'moderate to many severe problems' were 71.7% (76 cases) before treatment and significantly decreased to 46.2% (49 cases) after treatment (Fig. 3). In the patient's perception of treatment benefit, 89 patients (84.0%) reported that the treatment was beneficial (Fig. 4). Adverse effects related to medication were dizziness (3 cases), de novo stress urinary incontinence (3 cases), aggravation of underlying stress urinary incontinence (1 case), and fatigue (1 case). All the adverse effects disappeared after discontinuation of the medication. No other significant side effect possibly associated with the study drug was reported.
Our results show that the α1-AR antagonist tamsulosin has a beneficial effect on IPSS scores, bother scores, Qmax, PVR, diurnal and nocturnal frequencies, and BFLUTS-SF in women with non-neurogenic voiding dysfunction. This study also shows that the patient quality of life was improved by treatment and that the majority of patients felt a treatment benefit.
Although many urologists have empirically used α1-AR antagonists for the treatment of voiding phase dysfunction in women, little was known about their efficacies. The probable reasons for this are that no standard definition or guideline exists for the diagnosis of female voiding dysfunction and that its mechanism is poorly understood.
Several studies have suggested therapeutic rationales concerning the use α-AR antagonists for the treatment of voiding phase dysfunction in women. An animal study showed that the densities and affinities of α1-AR in male and female urethras are similar (6, 8). Nasu et al. (7) performed RNase protection assays and in situ hybridization to investigate ratios of α1-AR subtype mRNAs in human proximal urethra, and their localizations in urethral cross-sections. They found that α1A was the predominant mRNA subtype in both male and female urethral samples, and that α1D mRNA was present in only female samples. In situ hybridization studies showed no significant differences between male and female urethras in terms of the cross-sectional distributions of AR subtype mRNAs. These findings suggest that similar α1-adrenergic mechanisms control urethral tone in both sexes, and thus, it appears reasonable to consider the use of α1-AR antagonists in women with voiding dysfunction, because urethral resistance could be reduced during voiding. An early report described the effects of phenoxybenzamine, a nonselective α-AR antagonist, on women with a spastic striated external urethral sphincter. The authors found that symptoms were abolished, and that prolonged fluctuating flow curves were nearly normalized by phenoxybenzamine treatment (12). Some clinical trials have also suggested that α-AR antagonists may increase urine flow and decrease PVR in women with bladder outflow obstruction or a neurological bladder (13, 14). In the current study, we used tamsulosin (a selective α1A/1D-AR antagonist) to evaluate the potential therapeutic effects of α1-AR antagonists in female patients with voiding phase dysfunction because α1A and α1D was the predominant subtype in female urethras. Reitz et al. (15) demonstrated that tamsulosin had a significant relaxing effect on urethral tone in healthy females in vivo. In that study, microtip pressure transducer catheters were inserted into the bladder and urethral pressure profiles were obtained before and after the administration of tamsulosin. The oral administration of tamsulosin significantly reduced the mean and maximal urethral pressure acquired over the entire urethra. And there was a significant pressure reduction in all three segments when the proximal, middle and distal third of the urethra were analysed separately.
Recent literatures suggest that α-AR antagonists may provide an effective treatment option for female functional bladder outlet obstruction. Kumar et al. (16) reported that 50% of women with functional functional bladder outlet obstruction showed improvements in symptoms, Qmax, and PVR after treatment with α-AR antagonist alone. However, the other 50% of patients underwent bladder neck incision or remained on clean intermittent self-catheterization due to an inadequate response. Pischedda et al. (3) also reported on the efficacy of tamsulosin in female patients with functional bladder outlet obstruction. They used the following diagnostic criteria: Qmax <12 mL/sec, a detrusor voiding pressure at Qmax of >40 cm H2O, silent electromyographic activity of the external sphincter, inappropriate bladder neck funneling by fluoroscopy, a normal caliber urethra, and a PVR of ≥60 mL. Fifty-six percent of their study patients showed significant improvements in symptoms, Qmax, and PVR after being treated with tamsulosin (0.4 mg daily) for 1 month.
A small number of reports are available regarding the efficacy of α-AR antagonists for the treatment of detrusor underactivity. Yamanish et al. (4) reported that total IPSS decreased from 14.7 to 8.4 in female patients with detrusor underactivity after 4 weeks of α-AR antagonist treatment, and they also found that storage and voiding symptom scores were reduced. PVR was also significantly decreased from 135 mL to 87 mL.
Although no agreement has been reached concerning the diagnostic criteria of functional bladder outlet obstruction and detrusor underactivity, urodynamic studies, including pressure-flow studies with/without fluoroscopic examinations, are likely to be essential for determining bladder and urethral functions (1, 2, 4, 17). However, these evaluations appear too invasive to be performed routinely in women with LUTS and a low flow rate. Recently, two randomized placebo controlled trials-one for terazosin, one for tamsulosin-reported that α-AR antagonists could effectively reduce the LUTS in female patients without any urodynamic evaluations to clarify the etiology of LUTS (18, 19). In these studies, the inclusion criteria was just total IPSS 8 or greater in female adult. The baseline Qmax was more than 18.0 mL/sec in each study. The authors showed that IPSS was significantly improved in α-AR antagonists groups compared with placebo groups although there were no significant differences on Qmax between the two groups. The authors suggested that α-AR antagonists proved to be more effective than placebo in patients with female LUTS and that the improvement in IPSS may not be due to improvements in flow rates (18, 19). In a recent prospective study, Chang et al. (20) showed that tamsulosin could effectively improve both IPSS and Qmax in female patients with voiding difficulty. In 97 patients, IPSS was reduced from 20.2 to 14.8 and Qmax was increased from 10.4 mL/sec to 14.1 mL/sec (P<0.01) and a good therapeutic response was observed in 35.1% of patients after 6-week treatment. The authors also demonstrated that the improvements of IPSS and Qmax were not different between the bladder outlet obstruction (n=33) and detrusor underactivity group (n=52) in subgroup analysis. However, in that study, the inclusion criteria was obscure without the definition of voiding difficulty and much of the study patients had cormorbidities that might lead to voiding difficulties such as diabetes, Parkinsonism, herniation of intervertebral disc, etc. It suggests that the etiology of voiding difficulty was more diverse in that study.
The present study demonstrates that IPSS, bother score, Qmax, PVR, micturition frequency, and BFLUTS-SF were improved significantly after tamsulosin treatment in female patients with non-neurogenic voiding dysfunction who had LUTS and a low flow rate. This study also shows that changes in these parameters were similarly observed in those with different obstruction severities. Thus, the use of α1-AR antagonists in women with non-neurogenic voiding dysfunction appears reasonable, because they would reduce urethral resistance during micturition regardless of the degree of obstruction. In the current study, 72 (67.9%) patients showed an IPSS decrease of more than 5 points and 35 (33.0%) showed a Qmax increase of more than 50% with minimal adverse effects. We believe that this method represents a good therapeutic approach to female voiding dysfunction, before considering invasive tests, such as, pressure-flow studies and fluoroscopic examination, or more invasive treatment modalities, such as, clean intermittent self-catheterization and bladder neck incision. Nevertheless, tamsulosin treatment was found to be effective in some patients but not in others. Although we cannot provide a clear reason, this variability may be due to different underlying pathologies affecting micturition mechanisms.
The limitation of this study is that it was not a placebo-controlled study but an observational study, and thus, placebo effects may have affected symptom scores and subjective satisfaction ratings. However, we consider that this study is valuable because this study is performed for the relatively large scale of patients and shows that the α-AR antagonists is effective for the women with low flow rate and LUTS regardless of obstruction severity. Our findings indicate that α1-AR antagonists offer an initial treatment option for women with a non-neurogenic voiding dysfunction. To further determine the efficacy of α1-AR antagonists in women with voiding dysfunction a long-term, randomized, controlled study is required to compare the efficacy of α1-AR antagonists versus placebo treatment.
Tamsulosin demonstrated effectiveness in female patients with voiding dysfunction and its efficacies were independent of obstruction grade. A majority of patients showed subjective and objective improvements and were satisfied with treatment. Our findings suggest that α1-AR antagonists offer an initial treatment option for female non-neurogenic voiding dysfunction.
Figures and Tables
Fig. 1
Classification of the study subjects using a bladder outlet obstruction nomogram as devised by Blaivas and Groutz; Group A-no obstruction or mild obstruction, Group B-moderate obstruction or severe obstruction.
Pdetmax, maximum detrusor pressure; FreeQmax, maximum flow rate without catheter insertion.
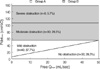
Fig. 2
Comparisons of changes in clinical parameters-IPSS (A), Qmax, PVR (B), micturition frequency, FBC (C), BFLUTS-SF (D)-pre- vs. post-treatment. Values are adjusted using baseline values as covariates. White bars represent group A and black bars group B.
P, group comparisons of improvement rates after treatment.
IPSS, International Prostate Symptom Score; Qmax, maximum flow rate; PVR, postvoid residual; FBC, functional bladder capacity; QoL, quality of life.

Fig. 3
Proportion of patients by the patient's perception of bladder condition-pre- vs. post-treatment. White bars include no problems at all, some very minor problems, and some minor problems. Black bars include (some) moderate problems, severe problems, and many severe problems.

Fig. 4
Proportion of patients by the patient's perception of treatment benefit-pre- vs. post-treatment.

Table 1
Changes in symptom scores including bother score and urodynamic parameters after 8 weeks treatment of tamsulosin

References
1. Groutz A, Blaivas JG. Non-neurogenic female voiding dysfunction. Curr Opin Urol. 2002. 12:311–316.

2. Kessler TM, Studer UE, Burkhard FC. The effect of terazosin on functional bladder outlet obstruction in women: a pilot study. J Urol. 2006. 176:1487–1492.

3. Pischedda A, Pirozzi Farina F, Madonia M, Cimino S, Morgia G. Use of alpha1-blockers in female functional bladder neck obstruction. Urol Int. 2005. 74:256–261.
4. Yamanishi T, Yasuda K, Kamai T, Tsujii T, Sakakibara R, Uchiyama T, Yoshida K. Combination of a cholinergic drug and an alpha-blocker is more effective than monotherapy for the treatment of voiding difficulty in patients with underactive detrusor. Int J Urol. 2004. 11:88–96.

5. Andersson KE, Lepor H, Wyllie MG. Prostatic alpha 1-adrenoceptors and uroselectivity. Prostate. 1997. 30:202–215.
6. Morita T, Latifpour J, O'Hollaren B, Wheeler MA, Weiss RM. Sex differences in function and distribution of alpha 1- and alpha 2-adrenoceptors in rabbit urethra. Am J Physiol. 1987. 252:F1124–F1128.

7. Nasu K, Moriyama N, Fukasawa R, Tsujimoto G, Tanaka T, Yano J, Kawabe K. Quantification and distribution of alpha1-adrenoceptor subtype mRNAs in human proximal urethra. Br J Pharmacol. 1998. 123:1289–1293.
8. Yablonsky F, Riffaud JP, Lacolle JY, Dausse JP. Alpha 1- and alpha 2-adrenoceptors in the smooth muscle of male and female rabbit urethra. Eur J Pharmacol. 1986. 121:1–8.
9. Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, Sterling AM, Zinner NR, van Kerrebroeck P. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002. 21:261–274.
10. Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004. 191:73–82.

11. Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn. 2000. 19:553–564.

12. Gerstenberg TC, Lykkegaard Nielsen M, Lindenberg J. Spastic striated external sphincter syndrome imitating recurrent urinary tract infection in females. Effect of long-term alpha-adrenergic blockade with phenoxybenzamine. Eur Urol. 1983. 9:87–92.
13. Kawabe K, Niijima T. Use of an alpha 1-blocker, YM-12617, in micturition difficulty. Urol Int. 1987. 42:280–284.
14. Yoshida O, Takeuchi H, Hida S, Tomoyoshi T, Arai Y, Okada K, Akino H, Isomatsu I, Okabe T, Fukuyama T, Komatsu Y, Fukuyama T, Takahashi Y, Nakamura KH, Sanada S, Ueda M, Inoue H, Matsuo M, Watanabe J, Hayashida H, Itokawa Y. Clinical efficacy and safety of long-term administration of YM617 for urinary obstruction of the lower urinary tract. Hinyokika Kiyo. 1991. 37:421–429.
15. Reitz A, Haferkamp A, Kyburz T, Knapp PA, Wefer B, Schurch B. The effect of tamsulosin on the resting tone and the contractile behaviour of the female urethra: a functional urodynamic study in healthy women. Eur Urol. 2004. 46:235–240.

16. Kumar A, Mandhani A, Gogoi S, Srivastava A. Management of functional bladder neck obstruction in women: use of alpha-blockers and pediatric resectoscope for bladder neck incision. J Urol. 1999. 162:2061–2065.
17. Akikwala TV, Fleischman N, Nitti VW. Comparison of diagnostic criteria for female bladder outlet obstruction. J Urol. 2006. 176:2093–2097.

18. Low BY, Liong ML, Yuen KH, Chee C, Leong WS, Chong WL, Khan NA, Cheah PY, Liong KK. Terazosin therapy for patients with female lower urinary tract symptoms: a randomized, double-blind, placebo controlled trial. J Urol. 2008. 179:1461–1469.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download