Abstract
The efficacy and toxicity of high-dose chemotherapy and autologous stem cell transplantation (HDCT/ASCT) were investigated for improving the outcomes of patients with relapsed medulloblastoma. A total of 15 patients with relapsed medulloblastoma were enrolled in the KSPNO-S-053 study from May 2005 to May 2007. All patients received approximately 4 cycles of salvage chemotherapy after relapse. Thirteen underwent HDCT/ASCT; CTE and CM regimen were employed for the first HDCT (HDCT1) and second HDCT (HDCT2), respectively, and 7 underwent HDCT2. One transplant related mortality (TRM) due to veno-occlusive disease (VOD) occurred during HDCT1 but HDCT2 was tolerable with no further TRM. The 3-yr overall survival probability and event-free survival rates ±95% confidence intervals (CI) were 33.3±12.2% and 26.7% ±11.4%, respectively. When analysis was confined to only patients who had a complete response (CR) or partial response (PR) prior to HDCT, the probability of 3-yr overall survival rates ±95% CI was 40.0±15.5%. No patients with stable disease (SD) or progressive disease (PD) survived. Survival rates from protocol KSPNO-S-053 are encouraging and show that tumor status prior to HDCT/ASCT is an important factor to consider for improving survival rates of patients with relapsed medulloblastoma.
The survival rate of those with relapsed brain tumors remains poor although treatment methods have been improved by multimodality treatment, radiotherapy and chemotherapy, with surgery (1, 2). Intrinsic chemo-resistance of relapsed tumors and previous radiotherapy limit treatment options at the time of relapse. High-dose chemotherapy (HDCT) and autologous stem cell transplantation (ASCT) have recently been applied in patients with relapsed brain tumor in order to overcome these obstacles, eradicate residual tumor cells, and extend survival (3, 4). Single transplantation had been known as a potentially curative method in many high-risk and relapsed central nervous system (CNS) tumors. Tandem transplantation for treatment of pediatric solid tumors such as high-risk neuroblastoma and retinoblastoma has been tried (5, 6). Tandem transplantation in cases of relapsed CNS tumors has also been attempted but the effectiveness of this therapy has not been proven (7). The Korean Society of Pediatric Neuro-Oncology (KSPNO) established the protocol KSPNO-S-053 to treat children with relapsed brain tumor diagnosed as medulloblastoma in an effort to improve the survival of pediatric patients treated with HDCT/ASCT including tandem transplantation.
This study included patients under 25 yr of age who had relapsed CNS tumors diagnosed as medulloblastoma between May 2005 and May 2007. These patients had been treated with various chemotherapies, surgery, or radiotherapy prior to relapse. Relapsed tumors were diagnosed by pathology after surgery, radiological study, and/or cerebrospinal fluid examination. Patients who underwent previous stem cell transplantation were excluded. A total of 16 patients were initially enrolled in the KSPNO-S-053 protocol. A case that had violation without using salvage regimens recommended by this protocol was excluded during the course of review leaving 15 patients. This protocol was approved by each hospital's institutional review board and informed consent was obtained from parents or guardians of all patients (IRB No. H-0808-025-253). Analysis was completed on 13 of 15 patients who were able to do HDCT/ASCT including tandem transplantation.
Following a diagnosis of relapsed medulloblastoma, patients were treated by surgery, radiotherapy if possible, and salvage chemotherapy (SC). The KSPNO-S-053 protocol recommended SC, alternating regimens A and B for 4 cycles; however, application of these regimens was not mandatory. Regimen A consists of: cisplatin 60 mg/m2/day on day 0; etoposide 50 mg/m2/day, days 0, 1, and 2; cyclophosphamide 750 mg/m2/day, days 1 and 2; and vincristine 1.5 mg/m2/day days 0 and 7. Regimen B consists of: carboplatin 200 mg/m2/day, days 0 and 1; etoposide 50 mg/m2/day, days 0, 1, 2, 3, and 4; ifosfamide 750 mg/m2/day, days 0, 1, 2, 3, and 4; and vincristine 1.5 mg/m2/day, days 0 and 7. Other generally accepted chemotherapy agents could be added to the recommended SC or the dose of recommended SC drugs could be modified according to physicians' choice to avoid the toxicity derived from overlapping chemotherapy drugs when similar drugs were used prior to relapse. The goal of SC was to minimize tumor burden prior to HDCT so that tumor status could be considered as having complete response (CR) or partial response (PR) before HDCT1. For this reason, the numbers of cycles of SC could be added or abstracted. After HDCT1, if the tumor status shows CR, tandem transplantation was optional; but in the case of PR or stable disease (SD), tandem transplantation was obligatory, and if progressive disease (PD) was the result, the recommendation was to go off therapy (Fig. 1).
All participants followed the protocol for conditioning regimens; however, it was optional whether a patient proceeded to tandem HDCT/ASCT if tumor status was CR after HDCT1 but obligatory if status indicated PR. The HDCT1 was administered with CTE regimen (carboplatin 500 mg/m2/day, day -8, -7, -6; thiotepa 300 mg/m2/day, day -5, -4, -3; etoposide 250 mg/m2/day, day -5, -4, -3). HDCT2 was administered with CM regimen (cyclophosphamide 1,500 mg/m2/day, day -8, -7, -6, -5; mephalan 60 mg/m2/day, day -4, -3, -2). An interval 12 weeks was recommended between HDCT1 and HDCT2. The patients received standard supportive care according to the physicians' discretion at each hospital following HDCT. No additional tumor-directed therapy was given after ASCT unless there were further residual or recurrent tumors.
If the absolute neutrophil count (ANC) became higher than 500/µL after the first SC cycle, granulocyte colony stimulating factor (G-CSF) 10 µg/kg/day was injected subcutaneously until the morning of the last day of leukapheresis for mobilization of PBSC collection. Leukapheresis was initiated when the white blood cell count was beyond 1,000/µL and monocytes in peripheral blood were ready to appear. The aim was to collect more than 5×106 CD34+ cells per kg of PBSC for use in 2 rounds of ASCT because of the possibility of tandem transplantation.
Neutrophil engraftment was defined as the first day when neutrophil counts rose from trough to 500/µL or above for 3 consecutive days. Platelet engraftment was defined as having risen above 20,000/µL without platelet transfusion for 7 consecutive days. CR was defined as resolution of all initially demonstrable tumors without appearance of new areas of disease. PR was defined as greater than a 50% decrease in the product of the 2 largest perpendicular tumor diameters, SD as less than a 50% decrease and PD as greater than a 25% increase.
Grading of toxicity was based on the National Cancer Institution Common Toxicity Criteria. Event-free survival (EFS) was considered from the date of diagnosis of a relapsed tumor to the date of disease relapse or progression or treatment related mortality (TRM), whichever came first. The overall survival (OS) was assessed from the date of diagnosis of a relapsed tumor to the date of death. Both EFS and OS rates were estimated using the Kaplan-Meier method and were compared using the log-rank test. Continuous variables in the 2 groups were compared using the Mann-Whitney U test. Statistical significance was accepted as P<0.05. Statistical software R was used to conduct the entire survival analyses.
Fifteen pediatric patients, 10 males and 5 females, diagnosed as having relapsed medulloblastoma were enrolled in the KSPHO-S-053 protocol. The mean age of the patients at the time of diagnosis of tumor relapse was 10.9 (range: 2-23) yr. All patients received a median 5 (range: 2-7) cycles of salvage chemotherapy (Table 1). All patients received regimen A or B (or B+) to minimize the toxicity of chemotherapeutic drugs used before their tumor relapsed, according to their physician's discretion. Seven patients received regimen (B+) containing irinotecan, modified on the basis of regimen B. Two patients could not receive HDCT: patient #12 experienced rapid progression of disease during SC so his general condition did not permit HDCT, and patient #8 died due to sepsis in a neutropenic condition during SC. Thirteen patients received HDCT with single or tandem ASCT; 7 received tandem transplantation and 6 received single transplantation. In the case of the 7 tandem transplantations, the period between HDCT1 and HDCT2 was median 105 (range 83-119) days.
Hematopoietic stem cells were mobilized and collected in all 14 patients who completed the first cycle of SC. The source of hematopoietic stem cells was peripheral blood in all patients, collected during a median 2 rounds of leukapheresis (range 1-4). The median of the collected total nucleated cells (TNC) and CD34+ cells were 12.2 (range 3.0-37.5)×108 cells/kg and 13.5 (range 4.6-134.3)×106 cells/kg, respectively.
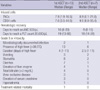
The median day of hematologic recovery after HDCT1, which required reaching an ANC over 500/µL and a platelet count over 20,000/µL without transfusion was 10 days (range 8-20) and 19 days (range 13-66), respectively. In patients who had undergone tandem transplantation, the median time of neutrophil and platelet count recovery after HDCT2 was 9 days (range 8-10) and 18 days (range 14-29), respectively (Table 2).
In this study, 2 patients died of TRM. Patient #8 died due to sepsis in a prolonged neutropenic state after the second cycle of SC. The other patient, #14, died of veno-occlusive disease (VOD) with septic shock during HDCT1 followed by ASCT. The most frequently developed grade 3 and 4 toxicities in 20 HDCTs were fever, stomatitis, diarrhea, elevated liver enzymes, and hyperbilirubinemia in order of frequency. There were no TRMs in the 7 patients who underwent HDCT2 (Table 2).
Three year OS and EFS rates of the total 15 patients from the time of relapse, were 33.3±12.2% and 26.7±11.4%, respectively (Fig. 2A). Of the 15 patients, 2 could not received HDCT(s) because 1 patient had rapidly progressive disease without preparing to do HDCT, and another patient died of sepsis during the period of SC. The 3-yr OS rate of the 13 patients who underwent HDCT(s) was 28.8±13.1% with a median follow-up of 21 months (range 9-44) after diagnosis of tumor relapse. Four patients are alive and event-free at 35, 38, 39 and 44 months since diagnosis of a relapsed tumor. Of 9 patients who had events, 8 experienced relapse or progression since HDCT1, and another had TRM at the time of HDCT1 and ASCT. Three-year EFS rates for these patients was 30.8±12.8% with a median follow-up of 16 months (range 7-44) after the diagnosis of relapsed tumor (Fig. 2B). There were no statistical differences in survival rates between the 2 groups of patients who received tandem (7 patients) or single (8 patients) transplantation (data not shown).
Of the 13 patients who underwent transplantation, there were 4 CRs, 6 PRs, 2 PDs and 1 SD pre-HDCT following SC. Three-year OS rates of 10 patients with status pre-HDCT of CR or PR was 40±15.5% with a median of 21 months (range 1-38) from HDCT1 (Fig. 2C), but 3 patients with SD or PD died due to disease progression with a median survival period of 7.5 months (range 6-16).
Of 4 patients with CR status pre-HDCT: one patient #2, who received optional HDCT2 and achieved CR status after HDCT1 as well as HDCT2, is alive. Another 3 patients, #1, #3 and #9, received single transplantation and maintained CR status after HDCT1 but 2 of them eventually experienced disease progressions to death leaving only 1 alive.
Of 6 patients with PR status pre-HDCT: 3 achieved CR status after HDCT1 and received optional HDCT2; 2 patients, #6 and #13 maintain CR status and are still alive. Patient #4, who achieved PR status after HDCT1 did not receive HDCT2 because the patient's guardian refused tandem transplantation. The disease of patient #15 progressed so he could not receive tandem transplantation, and patient #14 died of TRM at HDCT1 and ASCT (Fig. 3). These 3 patients who did not receive HDCT2 all died. The patients who were at PR status pre-HDCT could achieve long-term survival but patients who could not receive tandem transplantation died.
Three patients, 2 with PD and 1 with SD pre-HDCT that underwent HDCT2, all died of disease progression.
With the exception of 1 patient who died of TRM, 5 patients who could not reach CR status died due to disease progression or relapse irrespective of disease status after HDCT1. However, of 7 patients who reached CR after HDCT1, 3 of 4 who underwent tandem transplantation (4 optional indications) are alive, and only 1 of 3 (3 optional indications) who did not undergo tandem transplantation is alive, disease-free. This patient was in PR pre-HDCT, underwent SC, and achieved CR status after HDCT1, indicating that a second round of HDCT/ASCT might be helpful to patients who show a response to high-dose chemotherapy during HDCT1/ASCT.
Children with relapsed medulloblastoma have a dismal outcome with standard or alternative treatments (1). Two-year survival rates for relapsed medulloblastoma were reported to be below 20% (8). Recently, sequential cycles of dose-intensive chemotherapy or tandem transplantation have been tried in the treatment of chemo-sensitive high-risk or recurrent brain tumors, including recurrent medulloblastoma (9-11). The survival rate was reported as a broad range, 5-54%, by studies done in various different situations with regard to pre-transplant conventional chemotherapy, conditioning regimens, disease status prior to HDCT, and adjuvant therapy. Some studies did not separate recurrent medulloblastoma from high-risk medulloblastoma or other brain tumors types in their study group (8, 12). Grururangan et al. (13) reported a 3-yr overall survival rate of 14% in recurrent medulloblastoma patients who underwent HDCT/ASCT and received no irradiation before relapse, while no survival was found in those who underwent HDCT/ASCT receiving irradiation before relapse and in those who did not undergo HDCT/ASCT and received only standard SC. Our study, focusing on relapsed medulloblastoma, showed a 3-yr EFS and 3-yr OS of 31% and 29%, respectively (Fig. 2).
A few reports have shown that pre-HDCT disease status is most important when it comes to predicting survival rates in relapsed or high-risk brain tumor cases. The survival rate is highest in patients with previous CR status and less high in patients with minimal residual disease, but nearly absent in patients with bulky disease before ASCT (2, 10). Therefore, some reports that studied patients with relapsed brain tumor focused mainly on those with a PR or CR disease status prior to HDCT (10, 14). However, our study included data of PD or SD status, as well as CR or PR status, prior to HDCT1. In our study, the 3-yr OS rates in patients with PR or CR status prior to HDCT was 40%, compared to no survival in patients with PD or SD status (Fig. 2C).
Most recent reports of high-risk or relapsed brain tumors treated with HDCT/ASCT at CR status show favorable survival rates. Fagioli et al. (12) reported that patients with CR status following a poor prognosis brain tumor had a survival rate of 50.6% compare to 19.6% for those without CR status. Cheuk et al. (14) reported that long-term survival in CR patients before HDCT was 63% (5 out of 8 CR patients survived), but that 5 PR patients all died in the study of single transplantation in high-risk or recurrent CNS tumors. In our study, 4 patients who had both local and disseminated relapsed tumors achieved CR status at the time of their HDCT1. Two survived and were disease free with a 3-yr EFS rate of 50%. Relapsed patients with a previous CR status after multimodality salvage therapy, treated with HDCT/ASCT, are curable.
Some studies reported that patients with PR status before HDCT would die eventually from PD since the treatment of HDCT cannot eradicate their residual malignancies (12). The recent study by Cheuk et al. reported that 5 patients with PR disease status before HDCT, who had a median 8-month disease free period, did not survive a long-term (12, 14). However some researchers suggest that using multiple sequential intensive therapy or tandem transplantation has some benefit in this disease status before HDCT, because a single application of HDCT cannot eradicate the disease (9). Sung et al. (10) reported that of 9 patients with PR status before HDCT, whose tumors were high-risk or relapsed medulloblastoma and supratentorial primitive neuroectodermal tumor, 8 who received tandem transplantation were alive with a median follow-up of 18 month and 7 of those were disease free. In our study, 6 patients had PR status pre-HDCT; of those, 2 of 3 patients who received tandem transplantation were alive and disease free (44 and 38 months), but 3 patients who did not receive tandem transplantation died. These results show that tandem transplantation has the possibility of prolonging survival of relapsed pediatric medulloblastoma patients with PR status in response to upfront chemotherapy. In the future the role of tandem transplantation may need to be defined for patients with a status of PR after upfront chemotherapy before HDCT.
Of the total 15 patients, 4 who had no response or disease progression during the period of upfront SC died, although 3 were treated with tandem transplantation. Some other studies concerning the treatment of recurrent brain tumors using single or tandem transplantation showed similar results. Because the relapsed tumors achieved only PR or SD status after SC with or without surgery or irradiation, patients with PR or SD status at HDCT1 were not able to be cured with HDCT/ASCT, even with tandem transplantation.
Surgery, radiotherapy, and SC are common treatment methodologies used to reduce tumor burden prior to HDCT. Children diagnosed with relapsed medulloblastoma who were radiotherapy naïve and chemo-responsive were able to be cured. Butturini et al. (7) reported the 3-yr post-transplant EFS rate in unirradiated versus previously irradiated children to be 83% vs. 20% respectively, using a thiotepa based conditioning regimen. Our study had a similar result for 2 patients newly diagnosed before 3 yr of age who were unirradiated before relapse. These 2 patients, #2 and #13, received craniospinal irradiation following relapse and then received tandem transplantation and are now surviving disease-free.
Our study had 1 patient who died of VOD with sepsis at HDCT1 and ASCT, resulting in a TRM rate of 6.7%. Some reports, most of which had a conditioning regimen different from ours, showed that tandem or sequential courses of HDCT were tolerable in their toxicity (11). In our study, no TRM was seen in the cases of tandem transplantation and no elevation of liver enzymes was shown with tandem transplantation compared to single transplantation (Table 2). Rosenfeld et al. (15), who used the same conditioning regimens as our study at HDCT1 and HDCT2, reported 6 TRMs (32%) which included 4 cases of VOD, 4 incidences of sepsis, and 1 myelodysplastic syndrome in 19 patients who underwent single or tandem transplantation for treatment of recurrent CNS tumors including 9 medulloblastoma. The rate of VOD was 11% at HDCT1 using CTE regimen, and 18% at HDCT2 using CM regimen. The interval between HDCT1 and HDCT2 was approximately 50 days. While our study showed a VOD incidence rate similar to this report, the incidence was less at HDCT2 (only one patient; 14%) compared to HDCT1 (23%). Our study recommended HDCT2 be delayed about 12 weeks from HDCT1 according to reports that recommended 12 week intervals between HDCTs to prevent VOD (6). The longer intervals between HDCT1 and HDCT2 in our study may explain why we encountered less TRM and VOD at HDCT2 than reported by Rosenfeld.
This study was a multi-center trial; however, there were some limitations that should be addressed: first, it was impossible to compare the survival outcome between tandem and single transplantation because this study was not randomly compared; second, this study had a relatively short-term follow-up period so we could not formally evaluate long-term side effects using neuropsychological testing or quality of life assessment.
In conclusion, this study shows acceptable survival outcomes compared to other recent studies that utilized HDCT/ASCT in pediatric patients with relapsed medulloblastoma. Tandem transplantation is tolerated in pediatric patients with relapsed brain tumor. Patients with PD does not respond to tandem transplantation even following several courses of intensive SC, but this treatment may be helpful to prolong the survival of patients whose status was PR pre-HDCT and achieved CR after HDCT1. Therefore, it is suggested that active application of tandem transplantation, especially in patients with PR status prior to HDCT/ASCT, will be helpful to prolong survival in cases of relapsed medulloblastoma. The role of tandem transplantation for those with a PR status reached after SC should be defined by a larger scale study.
Figures and Tables
 | Fig. 1Overview of KSPNO-S-053 protocol for relapsed medulloblastoma.
CR, complete response; PR, partial response; PD, progressive disease; SD, stable disease.
|
 | Fig. 2(A) Event free and overall survival of all patients at 3 year survival from diagnosis of relapsed tumor (n=15). (B) Event free and overall survival of the patients who received HDCT from when diagnosis of relapsed tumor (n=13). (C) Overall survival of the patients who received HDCT in pre-HDCT CR or PR status vs. SD or PD status from 1st HDCT (n=10). |
 | Fig. 3Study progression following salvage chemotherapy (n=13).
*2nd HDCT was refused by a patient's guardian.
CR, complete response; PR, partial response; PD, progressive disease; SD, stable disease.
|
Table 1
Characteristics of patients with relapsed medulloblastoma (N=15)
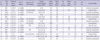
Pt. No., patient number; m, months; HDCT1, first high-dose chemotherapy; HDCT2, second HDCT; EFS, event free survival after relapse; OS, overall survival after relapse; S, surgery; RT, radiotherapy; CT, chemotherapy; p, primary site; m, metastatic site; Ds, disease; STR, subtotal resection; TRM, treatment related mortality; Radiation dose (Gy) for RT(craniospinal/primary/metastatic site); A, regimen A; B, regimen B; B+, modified regimen B including irinotecan.
References
1. Bouffet E, Doz F, Demaille MC, Tron P, Roche H, Plantaz D, Thyss A, Stephan JL, Lejars O, Sariban E, Buclon M, Zucker JM, Brunat-Mentigny M, Bernard JL, Gentet JC. Improving survival in recurrent medulloblastoma: earlier detection, better treatment or still an impasse? Br J Cancer. 1998. 77:1321–1326.

2. Finlay JL, Goldman S, Wong MC, Cairo M, Garvin J, August C, Cohen BH, Stanley P, Zimmerman RA, Bostrom B, Geyer JR, Harris RE, Sanders J, Yates AJ, Boyett JM, Packer RJ. The Children's Cancer Group. Pilot study of high-dose thiotepa and etoposide with autologous bone marrow rescue in children and young adults with recurrent CNS tumors. J Clin Oncol. 1996. 14:2495–2503.
3. Shih CS, Hale GA, Gronewold L, Tong X, Laningham FH, Gilger EA, Srivastava DK, Kun LE, Gajjar A, Fouladi M. High-dose chemotherapy with autologous stem cell rescue for children with recurrent malignant brain tumors. Cancer. 2008. 112:1345–1353.

4. Perez-Martinez A, Lassaletta A, Gonzalez-Vicent M, Sevilla J, Diaz MA, Madero L. High-dose chemotherapy with autologous stem cell rescue for children with high risk and recurrent medulloblastoma and supratentorial primitive neuroectodermal tumors. J Neurooncol. 2005. 71:33–38.

5. Lee SH, Yoo KH, Sung KW, Kim JY, Cho EJ, Koo HH, Chung SE, Kang SW, Oh SY, Ham DI, Kim YD. Tandem high-dose chemotherapy and autologous stem cell rescue in children with bilateral advanced retinoblastoma. Bone Marrow Transplant. 2008. 42:385–391.

6. Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, Lee SK, Kim J, Lim DH, Suh YL, Kim DW. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007. 40:37–45.

7. Butturini AM, Jacob M, Aguajo J, Vander-Walde NA, Villablanca J, Jubran R, Erdreich-Epstein A, Marachelian A, Dhall G, Finlay JL. High-dose chemotherapy and autologous hematopoietic progenitor cell rescue in children with recurrent medulloblastoma and supratentorial primitive neuroectodermal tumors. Cancer. 2009. 115:2956–2963.

8. Grodman H, Wolfe L, Kretschmar C. Outcome of patients with recurrent medulloblastoma or central nervous system germinoma treated with low dose continuous intravenous etoposide along with dose-intensive chemotherapy followed by autologous hematopoietic stem cell rescue. Pediatr Blood Cancer. 2009. 53:33–36.

9. Foreman NK, Schissel D, Le T, Strain J, Fleitz J, Quinones R, Giller R. A study of sequential high dose cyclophosphamide and high dose carboplatin with peripheral stem-cell rescue in resistant or recurrent pediatric brain tumors. J Neurooncol. 2005. 71:181–187.

10. Sung KW, Yoo KH, Cho EJ, Koo HH, Lim do H, Shin HJ, Ahn SD, Ra YS, Choi ES, Ghim TT. High-dose chemotherapy and autologous stem cell rescue in children with newly diagnosed high-risk or relapsed medulloblastoma or supratentorial primitive neuroectodermal tumor. Pediatr Blood Cancer. 2007. 48:408–415.

11. Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE, Woo S, Wheeler G, Ahern V, Krasin MJ, Fouladi M, Broniscer A, Krance R, Hale GA, Stewart CF, Dauser R, Sanford RA, Fuller C, Lau C, Boyett JM, Wallace D, Gilbertson RJ. Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol. 2006. 7:813–820.

12. Fagioli F, Biasin E, Mastrodicasa L, Sandri A, Ferrero I, Berger M, Vassallo E, Madon E. High-dose thiotepa and etoposide in children with poor-prognosis brain tumors. Cancer. 2004. 100:2215–2221.

13. Gururangan S, Krauser J, Watral MA, Driscoll T, Larrier N, Reardon DA, Rich JN, Quinn JA, Vredenburgh JJ, Desjardins A, McLendon RE, Fuchs H, Kurtzberg J, Friedman HS. Efficacy of high-dose chemotherapy or standard salvage therapy in patients with recurrent medulloblastoma. Neuro-oncol. 2008. 10:745–751.

14. Cheuk DK, Lee TL, Chiang AK, Ha SY, Chan GC. Autologous hematopoietic stem cell transplantation for high-risk brain tumors in children. J Neurooncol. 2008. 86:337–347.

15. Rosenfeld A, Kletzel M, Duerst R, Jacobsohn D, Haut P, Weinstein J, Rademaker A, Schaefer C, Evans L, Fouts M, Goldman S. A phase II prospective study of sequential myeloablative chemotherapy with hematopoietic stem cell rescue for the treatment of selected high risk and recurrent central nervous system tumors. J Neurooncol. 2010. 97:247–255.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download