Abstract
On June 14, 2008, an outbreak of gastroenteritis occurred among elementary school students in Incheon. We conducted an investigation to identify the source and described the extent of the outbreak. We performed a retrospective cohort study among students, teachers and food handlers exposed to canteen food in the elementary school. Using self-administered questionnaires we collected information on symptoms, days of canteen food eaten, food items consumed. Stool samples were collected from 131 symptomatic people and 11 food handlers. The catering kitchen was inspected and food samples were taken. Of the 1,560 people who ate canteen food, 117 were symptomatic cases, and the attack rate was 7.5%. Consumption of cucumber-crown daisy salad (RR=2.71), fresh cabbage mix (RR=2.23), dried radish salad (RR=3.04) and young radish kimchi (RR=2.52) were associated with illness. Sixty-four (45%) of the 142 stool specimens were positive for Norovirus. Norovirus was detected in 2 food handlers. Interviews with kitchen staff indicated the likelihood of contamination from an infected food handler to the dried radish salad during food processing. The excretion of Norovirus from asymptomatic food handlers may be an infection source of Norovirus outbreaks.
Norovirus (NV) is recognized as a worldwide cause of acute nonbacterial gastroenteritis (1). The virus is transmitted predominantly through ingestion of contaminated food as well as person-to-person by the fecal-oral route, airborne transmission, and contact with contaminated surfaces (2-4). For 348 outbreaks of NV gastroenteritis reported to the U.S. Centers for Disease Control and Prevention during 1996-2000, food was implicated in 39%, person-to-person contact in 12%, and water in 3%; 18% could not be linked to a specific transmission mode (5). Infected food handlers have been implicated repeatedly as the source of infection in several outbreaks (6-8). Asymptomatic NV infections of food handlers may play a role in transmission (9). Since 2003, there have been several large outbreaks of NV in Korea (10-12). However, few studies have linked the outbreaks with asymptomatic food handlers.
On June 14, 2008, a parent contacted the Incheon City school infirmary to report that her child had symptoms of diarrhea accompanied by an abdominal cramp. The school nurse reported to a regional public health office that mass food poisoning prevailed among students. The epidemiological investigation team in the public health office arrived at the school and started an epidemiological investigation. Additional students came down with symptoms after the epidemiological study had commenced. By June 16, a total of 131 people were afflicted with symptoms of the disease. On June 16, a second epidemiological investigation team was deployed to Incheon City to perform a field investigation. The objective of this study was to identify the source and describe the extent of the outbreak that occurred at an elementary school on June 14, 2008.
We did a retrospective cohort study among students, teachers and food handlers exposed to canteen food in the elementary school. Based on the typical incubation period of NV (24-48 hr) (5) and reports of peak incidence on June 13, exposure was most likely to have occurred during June 11-12. Self-administered paper questionnaires were distributed to students, teachers and food handlers on June 16 and information was collected on demographic details, symptoms, time of onset and duration of illness, the individual canteen food items consumed in the canteen during June 11-13. A case was defined as a confirmed case or a school member who consumed canteen food during June 11-13 and who developed vomiting, accompanied with one or more symptoms such as abdominal pain, headache, nausea and diarrhea after June 13.
We inspected the catering kitchen and interviewed kitchen staff about food handling practices and illness. Processed, unprocessed food and drinking water specimens were collected and examined by the public health office. Specimens of kitchen utensils were collected and investigated. Symptomatic people (including cases) and food handlers were asked to submit stool samples for standard bacteriological and virological analysis. We calculated food and water specific attack rates (AR), relative risks (RR), 95% confidence intervals (95% CI). We measured the association between the drinking water (or food) consumption and the risk of disease using chi-squared test or Fisher's exact test. Statistical analyses were made using SPSS (version 12.0.1).
This study was approved by the Institutional Review Board of Inha University (IRB No. 2010-0125).
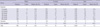
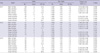
Of the 1,560 school members who consumed canteen food (1,485 students, 64 teachers, 11 food handlers), 1,522 (97.5%) returned questionnaires. Therefore, 1,522 questionnaires were included in the analysis. Among the 1,522 school members, 1,452 (95.4%) were students and 59 (3.8%) were teachers. Eleven (0.7%) of the 1,522 school members were food handlers. The median age in this cohort was 10 yr (range 5-60 yr), and 752 (49.4%) were male. One hundred and seventeen school members met the case definition. The overall attack rate was 7.5% (117/1,560). AR did not differ significantly among groups or among grades. However, the AR was higher significantly in females than males (P=0.03) (Table 1).
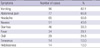
Day of illness onset for 88 cases is shown in Fig. 1; information on date of onset was missing for 29 cases. The epidemic curve showed characteristics of a single exposure route. The canteen food and drinking water were provided during lunch time (12:00-13:00). The first patient developed symptoms beginning at approximately 1 a.m. on June 13. After a slight increase beginning in the morning on June 13, the number of cases rose sharply to a distinct peak in the afternoon on June 13 and decreased then exponentially during the following 2 days. The cases' main symptoms were vomiting (82.1%) and abdominal pain (65.8%). Fever (29.1%) and tenesmus (12.0%) were less frequent (Table 2).
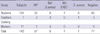
Of the 142 people who provided stool samples (Table 3, 4), 64 samples were positive for NV (45%), two of these samples were from food handlers. All NV genotypes were GII-4 except for 1 student, whose NV genotype was an unusual type. All sequences detected in this study closely matched the published sequences (Fig. 2). The GII-4 sequences shared 100% nucleotide similarity. This reveals that there was a single source of infection in this outbreak. The second stool examination was made on June 26 for the 2 food handlers (A, B) testing positive for NV. It came out that NV was positive in the food handler A. The third investigation was made for the food handler A on July 9. The result of the third investigation was negative for NV. Besides, other bacteria (Enterohemorrhagic Escherichia coli, Staphylococcus aureus) were detected simultaneously in 7 students testing positive for NV. However, the number of the protons of these bacteria was too small to be considered as the cause of the outbreak of this food poisoning. The results of the drinking water and environmental specimen all came out as non-detection (Table 3). The drinking water in the purifiers was not examined for NV. In order to detect NV in water with Korean technology, more than 100 L of water was required as a sample. The amount of the water stored in the water purifiers was not enough.
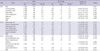
Upon menu analyses, the cucumber-crown daisy salad, fresh cabbage mix on June 11 and the dried radish salad, young radish kimchi on June 12 were statistically significant (Table 5). Consumption of drinking water on the 4th floor in main building (on June 11, 13) was associated with illness (Table 6). However, the number of cases consumed the water on the 4th floor in main building was so low for the cause of outbreak.
The food ingredients of the cucumber-crown daisy salad, the dried radish salad were cucumbers, crown daisies, dried radishes. All of them had been supplied by company A. The company A supplied the food ingredients as they received them from the cultivating farms without going through any washing processes. Among 112 schools supplied by the company A, there were no cases of food poisoning at the other schools. All vegetable ingredients supplied by the company A were chlorinated, with water chlorinated to the concentration rate of 100 ppm in the kitchen sink, so the chance that NV came in from food ingredients from supplier companies is low. Fresh cabbage mix and young radish kimchi were supplied by company B. The company B also supplied other schools (128 schools) with the same products and no food poisoning occurred in these schools.
The kitchen had water supplies and a water purifier. The water supplies were used in the process of preparing food. However, the water purifier was not used. The original water for the water purifier was supplied from water suppliers. The filters of the water purifiers in the school have been replaced with new ones once in 3-4 months. Water samples collected from the water purifiers in the school were tested on May 21 at private inspecting office and were negative for total coliform bacteria. As a result of measuring the residual chlorine concentration rates of the water pipes in the bathrooms in the kitchen, the main building, the annex building and outside the building, the concentration rates were more than 0.47 ppm and there was no evidence of underground water supplies. There was no evidence of underground water supplies in their water supplies and drainage tax receipts during the last three months. Also, drainage pipes were located outside the kitchen at intervals of about 1 meter. They looked unclean and smelled nasty. The school facilities had been worn out for more than 20 yr so there was a possibility of cross contamination between the water supply pipes and the drainage pipes. Considering the water supplies in the kitchen might have been contaminated, it was requested that the water supplies in the kitchen be investigated. However, the investigation had not been made because of terms in administrative procedures.
There were 11 food handlers (1 nutritionist, 8 food handlers, 2 food deliverers) at the school. One of the food handlers (C) had a medical history of going to a clinic due to flu-like symptoms. She had no other symptoms except sweating and myalgia. She had recovered after taking medication for 3 days. All the other food handlers stated that they had no related symptoms. A request was made to the National Health Insurance Corporation for medical records of 3 food handlers (A, B, C) from May 1 to June 14. There was no evidence of NV infection found on the record.
An Interview with a nutritionist revealed that food handler A participated in cooking dried radish salad. The food handler A washed dried radish after steeping them in water for 4-5 hr. Then, she dipped them in the red pepper sauce and stored them in the refrigerator. In the answer of questionnaire, the food handler A stated that she had no idea whether she ate dried radish salad or not. So, the food handler A might eat very few dried radish salad. The food handler B did not participate in any process of cooking dried radish salad or cucumber-crown daisy salad but ate both of them. The food handler C made cucumber-crown daisy salad. She stirred cucumber and crown daisy into salad sauce. In-depth interviews with the food handlers revealed that they had not had any symptoms within 1 month prior to the outbreak. Interviews with other food handlers revealed that food handler D participated in cooking (washing and cutting) cucumber-crown daisy salad and dried radish salad simultaneously. However, the stool sample of food handler D was negative for NV.
The results suggest that the vehicle of transmission in this outbreak was dried radish salad prepared by the food handler A and served to students of the elementary school on June 12. This finding is not surprising, given that approximately 50% of all NV outbreaks in the United States are linked to ill food-handlers (13). Ozawa et al. reported that the frequency of NV detection was 19% in outbreak facilities in Japan and that 73% of symptomatic food handlers and 7% of asymptomatic food handlers were positive for NV (14). They suggested that asymptomatic infections are common and contribute to the spread of the infection in areas of outbreak.
In the case of dried radish salad, there was a process of washing, steeping in water, dipping in red pepper sauce with the food handler A's hands. Additionally, there is a possibility that the food handler A did not have the dried radish salad. This means that food handler A might not be infected through the dried radish salad but through other routes. This suggests that the salad had been contaminated with NV through food handler A's hands. Considering the incubation period and the fact that the food handlers A, B did not participate in cooking cucumber-crown daisy salad, the chance is very low that the cucumber-crown daisy salad was a vehicle of transmission. Considering the fact that food handler D participated in cooking cucumber-crown daisy salad and dried radish salad simultaneously, it is possible that she contaminated both menus and did not excrete NV on the day of stool examination. However, additional evidence was not available.
Also, in case of fresh cabbage mix and young radish kimchi, finished products were used for the school meals only by unpacking the food. Therefore, there was no possibility that the products were contaminated by food handlers. Considering no occurrence of food poisoning in other schools supplied by the same company, Both of them could hardly be the vehicle of transmission.
It is known that the period that NV can be detected is usually from 2 days after the symptoms start to 2 weeks later after the recovery. However, Elise et al. reported that the period that the virus RNAs are detected in the stools of the patients turned out to be 28.7 days (13.5 days-44.5 days) on an average (15). Also, Atmar et al. reported the similar results (16). This reveals that the excretion of NV from food handler A can last longer than 2 weeks. Therefore, food handler A can be infected by NV before June 12 (dried radish salad was provided on June 12) and positive for NV until June 26.
Students stated that they usually drank water that they brought from home. They said they did not drink water from the water purifiers. Few students drank water from the water purifier near their classrooms. However, there is no chance that water purifiers might have been the source of infection, because the NV cases ranged across the grades. It is not plausible that all the purifiers installed on every floor were contaminated at once.
Food handlers used the water from the water supplies in the kitchen when making cucumber-crown daisy salad and dried radish salad. Drainage pipes outside the kitchen had been worn out and buried near the water supply pipes at intervals of about 50 cm. NV can survive below the residual chlorine concentration rate 10 ppm (17). However, there was no possibility of cross contamination between the water supply pipes and the drainage pipes. It is because pathogenic E. coli that suggest fecal contamination were not detected in the water from the water supplies in the kitchen. In terms of water supplies, the risk of cross contamination increases when it rains, but it did not rain within 1 week before the outbreak. Even though there was no replacement of the drainage pipes, additional outbreak has not occurred for a year since the outbreak.
In conclusion, NV is considered to be the cause of this outbreak. The findings in this report are subject to at least three limitations. First, it was impossible to detect NV in preserved foods and food ingredients due to technical limitations. In order to confirm the vehicle of transmission, it is necessary to detect NV in the suspected foods. Second, it appears that certain answers of questionnaires are inaccurate because the majority of respondents are children. The statistical result that four menus were significant simultaneously shows this possibility. Third, it was impossible to decide whether food handlers A, B were infected through the outbreak or not, because they ate the canteen foods. Despite these limitations, this outbreak in Incheon provides insights and lessons that the excretion of NV from asymptomatic food handlers may be an infection source of NV outbreaks, especially in a place where underground water is not used. For a better risk management, more focus should be put on asymptomatic food handlers.
Figures and Tables
Fig. 2
Phylogenetic relationships between the outbreak strains and reference strains of NV based on partial nucleotide sequence of capsid. Nucleotide sequences were aligned using Clustal W and a phylogenetic tree was constructed by Neighbor-Joining method. The numbers on each branch indicate the bootstrap values for the clusters supported by that branch. Branch lengths are proportional to the calculated genetic distances (scale shown). FH A indicates the food handler A.

References
1. Rockx B, De Wit M, Vennema H, Vinje J, De Bruin E, Van Duynhoven Y, Koopmans M. Natural history of human calicivirus infection: a prospective cohort study. Clin Infect Dis. 2002. 35:246–253.
2. Fretz R, Svoboda P, Luthi TM, Tanner M, Baumgartner A. Outbreaks of gastroenteritis due to infections with Norovirus in Switzerland, 2001-2003. Epidemiol Infect. 2005. 133:429–437.

3. Kuusi M, Nuorti JP, Maunula L, Minh Tran NN, Ratia M, Karlsson J, von Bonsdorff CH. A prolonged outbreak of Norwalk-like calicivirus (NLV) gastroenteritis in a rehabilitation centre due to environmental contamination. Epidemiol Infect. 2002. 129:133–138.

4. Marks PJ, Vipond IB, Regan FM, Wedgwood K, Fey RE, Caul EO. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol Infect. 2003. 131:727–736.

5. Parashar U, Quiroz ES, Mounts AW, Monroe SS, Fankhauser RL, Ando T, Noel JS, Bulens SN, Beard SR, Li JF, Bresee JS, Glass RI. "Norwalk-like viruses." Public health consequences and outbreak management. MMWR Recomm Rep. 2001. 50:1–17.
6. Iversen AM, Gill M, Bartlett CL, Cubitt WD, McSwiggan DA. Two outbreaks of foodborne gastroenteritis caused by a small round structured virus: evidence of prolonged infectivity in a food handler. Lancet. 1987. 2:556–558.

7. Kilgore PE, Belay ED, Hamlin DM, Noel JS, Humphrey CD, Gary HE Jr, Ando T, Monroe SS, Kludt PE, Rosenthal DS, Freeman J, Glass RI. A university outbreak of gastroenteritis due to a small round-structured virus. Application of molecular diagnostics to identify the etiologic agent and patterns of transmission. J Infect Dis. 1996. 173:787–793.

8. Reid JA, Caul EO, White DG, Palmer SR. Role of infected food handler in hotel outbreak of Norwalk-like viral gastroenteritis: implications for control. Lancet. 1988. 2:321–323.

9. Parashar UD, Dow L, Fankhauser RL, Humphrey CD, Miller J, Ando T, Williams KS, Eddy CR, Noel JS, Ingram T, Bresee JS, Monroe SS, Glass RI. An outbreak of viral gastroenteritis associated with consumption of sandwiches: implications for the control of transmission by food handlers. Epidemiol Infect. 1998. 121:615–621.

10. KCDC. Service DoEI. Epidemiological investigation report of mass food poisoning in the Metropolitan area, Korea, 2006. 2006-2007. Seoul: Korea Centers for Disease Control and Prevention;169–181.
11. Kim SH, Cheon DS, Kim JH, Lee DH, Jheong WH, Heo YJ, Chung HM, Jee Y, Lee JS. Outbreaks of gastroenteritis that occurred during school excursions in Korea were associated with several waterborne strains of norovirus. J Clin Microbiol. 2005. 43:4836–4839.

12. Lee HJ, Lee SW, Bang JH, Lim DJ, En SH, Park MS, Sin HJ. Service Do EI. Norwalk-virus food poisoning epidemiological investigation, Seoul, Korea, 2003. 2003-2004. Seoul: Korea Centers for Disease Control and Prevention;103–113.
13. Widdowson MA, Sulka A, Bulens SN, Beard RS, Chaves SS, Hammond R, Salehi ED, Swanson E, Totaro J, Woron R, Mead PS, Bresee JS, Monroe SS, Glass RI. Norovirus and foodborne disease, United States, 1991-2000. Emerg Infect Dis. 2005. 11:95–102.

14. Ozawa K, Oka T, Takeda N, Hansman GS. Norovirus infections in symptomatic and asymptomatic food handlers in Japan. J Clin Microbiol. 2007. 45:3996–4005.

15. Tu ET, Bull RA, Kim MJ, McIver CJ, Heron L, Rawlinson WD, White PA. Norovirus excretion in an aged-care setting. J Clin Microbiol. 2008. 46:2119–2121.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download