Abstract
Multiple epiphyseal dysplasia is caused by heterogenous genotypes involving more than six genes. Recessive mutations in the DTDST gene cause a phenotype of recessive multiple epiphyseal dysplasia (rMED). The authors report a 9-yr old Korean girl with the rMED phenotype having novel compound heterozygous mutations in the DTDST gene, which were inherited from both parents. This is the first Korean rMED case attributed to DTDST mutations, and expands the spectrum of diseases caused by DTDST mutations.
Multiple epiphyseal dysplasia is a heterogenous group of diseases, clinically characterized by a mild-to-moderate short stature, angular deformities of the extremities, short hands and feet, and precocious osteoarthritis. The severity of the disease varies case to case even in those with the same genotype, and the most severe cases are sometimes difficult to differentiate from pseudoachondroplasia (PSACH). Mutations in genes coding cartilage oligomeric matrix protein (COMP), type IX collagen alpha 1, 2, and 3 chains (COL9A1, COL9A2, COL9A3), and matrilin 3 (MATN3) cause the dominantly inherited forms of MED, while homozygous or compound heterozygous mutations in diastrophic dysplasia sulfate transporter (DTDST or SLC26A2) gene cause recessively inherited MED (rMED, EDM4 OMIM 226900) (1, 2). However, additional MED loci have been suggested, as many MED patients do not show any mutations in the above genes (1, 2). Superti-Furga et al. (3) first reported that a homozygous p.R279W mutation in the DTDST gene developed a phenotype resembling MED, rather than diastrophic dysplasia (DTD). Subsequently, more homozygous or compound heterozygous mutations in the DTDST gene were reported in rMED patients (4, 5). However, no rMED case caused by DTDST gene mutations has been reported in the Asian population (2). Only an intermediate phenotype of Desbuquois dysplasia, diastrophic dysplasia and rMED with compound heterozygotic mutation in DTDST gene was reported in a Japanese patient (6). In the present study, we identified novel compound heterozygous mutations in a Korean girl with the rMED phenotype.
A girl was born to non-consanguineous, healthy Korean parents after a normal pregnancy with a birth weight of 3.06 kg. Any family history of musculoskeletal system was denied. Her motor development was within normal limit. At age 9 yr, she visited our clinic due to an apparent foot deformity, which was first noticed at age 3 yr. She did not have any limitation in daily activity or joint pain, but was poor at sports. Her height was 131 cm (42th percentile) and her weight 37.9 kg (80th percentile). Her face, palate, and external ears were normal. Fingers and thumbs were short but in normal alignment. Both knees and ankles were in valgus alignment. Her forefeet were adducted, which was more severe on the right side (Fig. 1A-C). A radiographic examination showed small, dysplastic epiphyses at hips, knees, ankles, and wrists. Metacarpals and phalanges were short and had flat epi-physes, and premature physeal closure at the proximal and middle phalanges of both hands had resulted in brachydactyly. A lateral view of the knees revealed double layered patellae. Forefoot adduction deformity had been caused by deformed medial cuneiform bones and twisted metatarsals (Fig. 1D-G). The spine was normal in appearance and alignment. Detailed clinical and radiographic surveys were performed to the parents of proband. Her father's height was 174 cm and her mother's 160 cm. They did not show any deformity on physical examination.
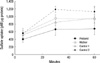
Genetic and biochemical study for this family was approved by the Institutional Review Board of Seoul National University Hospital. Direct sequencing analysis of PCR amplified DNA from the proband genomic DNA demonstrated no mutation in COMP, COL9A1, COL9A2, COL9A3, and MATN3. However, she had a compound heterozygous mutations in the DTDST gene, i.e., a c.485_486delTG, p.Val162GlyfsX12 mutation and a c.1153G>A, p.D385N mutation in exon 3, neither of which has been previously reported to be associated with any disease. Her mother's genomic DNA had a heterozygous c.485_486delTG mutation while her father's contained a heterozygous c.1153G>A (Fig. 2). None of 171 normal subjects (342 normal chromosomes) were shown to contain c.1153G>A variation. Interspecies amino acid sequence of p.D385 was conserved in all the species tested except Xenopus tropicalis (Fig. 3). Dermal fibroblast sulfate uptake assays (7) revealed 65-74% of the normal control level in the proband, but a near normal level in her mother (Fig. 4). Normal controls were dermal fibroblasts harvested during surgical procedure from previously healthy fracture patients of the same sage with index case. The father's dermal fibroblast was not available.
This case showed clinical and radiographic findings compatible with rMED, i.e., double layered patellae, flattened proximal femoral epiphyses, brachydactyly, feet deformity, and genu valgum. Full sequencing of the DTDST gene in the proband and both parents revealed two previously unreported mutations that had been inherited by the proband from both parents.
Hastbacka et al. (8) identified a gene for diastrophic dysplasia by linkage disequilibrium mapping. As encoded a novel sulfate transporter, it was named as DTDST, and later as SLC26A2. Undersulfation of proteoglycan, which was an important component of cartilage matrix, was found in DTD patient (9). Forlino et al. (10) showed impaired sulfate uptake in chondrocytes, osteoblasts and fibroblasts, significant proteoglycan undersulfation in cartilage, and reduced proliferation and/or lack of terminal chondrocyte differentiation in homozygous SLC26A2-mutant knock-in mice.
Recessive mutations in the DTDST gene cause a spectrum of osteochondrodysplasias, including achondrogenesis type IB, atelosteogenesis type II, and DTD. rMED has been reported to caused by homozygous or compound heterozygous mutations of the DTDST gene, containing either R-279W or C635S (3-5). Mikaye et al. (6) reported a case with an intermediate phenotype between rMED and DTD caused by a compound heterozygote of a novel p.T266I and a recurrent p.ΔV340 mutation. As missense mutation causing R178X was found in DTD patients (11), it is for sure that c.485_486delTG, p.Val162GlyfsX12 mutation from maternal allele in the proband will produce a truncated protein and contribute to development of the phenotype. The c.1153G>A, p.D385N mutation from paternal allele resides in the middle of sulfate transporter domain. No c.1153G>A variation was found in 171 normal subjects, and p.D385 was well conserved in other species, suggesting that c.1153G>A, p.D385N is not a polymorphism but a mutation. Hence, the compound heterozygous mutations in DTDST gene of the proband are cause of her phenotype. It is also supported by reduced uptake of sulfate in in vitro assay (Fig. 4).
As regards foot deformity, the proband had hindfoot valgus and metatarsus adductus, which should be described as skewfoot (12), rather than clubfoot. Ryoppy et al. (13) reported that 43% of their DTD cases had skewfoot deformity, and that only 29% had genuine clubfoot (equinovarus) deformity, and as was pointed by these authors the expression "clubfoot", as generally used to describe foot deformity in DTD, is a misnomer. A more specific description of foot deformity is required in patients with DTDST-associated diseases.
Figures and Tables
Fig. 1
The proband aged 9 yr. Mild genu valgum, forefoot adduction, and hindfoot valgus were noted (A-C). Radiographs showed genu valgum with flattening of epiphyses at the hips, knees, and ankles (D); double layered patella (E); shortening of the metacarpals and phalanges, premature physeal closure at the middle phalanges, cone-shaped epiphyses of the proximal phalanges (F); twisted, oblique arrays of the metatarsals, triangular medial cuneiforms (G).

References
1. Jakkula E, Makitie O, Czarny-Ratajczak M, Jackson GC, Damignani R, Susic M, Briggs MD, Cole WG, Ala-Kokko L. Mutations in the known genes are not the major cause of MED; distinctive phenotypic entities among patients with no identified mutations. Eur J Hum Genet. 2005. 13:292–301.

2. Itoh T, Shirahama S, Nakashima E, Maeda K, Haga N, Kitoh H, Kosaki R, Ohashi H, Nishimura G, Ikegawa S. Comprehensive screening of multiple epiphyseal dysplasia mutations in Japanese population. Am J Med Genet A. 2006. 140:1280–1284.

3. Superti-Furga A, Neumann L, Riebel T, Eich G, Steinmann B, Spranger J, Kunze J. Recessively inherited multiple epiphyseal dysplasia with normal stature, club foot, and double layered patella caused by a DTDST mutation. J Med Genet. 1999. 36:621–624.
4. Makitie O, Savarirayan R, Bonafe L, Robertson S, Susic M, Superti-Furga A, Cole WG. Autosomal recessive multiple epiphyseal dysplasia with homozygosity for C653S in the DTDST gene: double-layer patella as a reliable sign. Am J Med Genet A. 2003. 122:187–192.
5. Ballhausen D, Bonafe L, Terhal P, Unger SL, Bellus G, Classen M, Hamel BC, Spranger J, Zabel B, Cohn DH, Cole WG, Hecht JT, Superti-Furga A. Recessive multiple epiphyseal dysplasia (rMED): phenotype delineation in eighteen homozygotes for DTDST mutation R279W. J Med Genet. 2003. 40:65–71.

6. Miyake A, Nishimura G, Futami T, Ohashi H, Chiba K, Toyama Y, Furuichi T, Ikegawa S. A compound heterozygote of novel and recurrent DTDST mutations results in a novel intermediate phenotype of Desbuquois dysplasia, diastrophic dysplasia, and recessive form of multiple epiphyseal dysplasia. J Hum Genet. 2008. 53:764–768.

7. Imauchi Y, Lombes M, Laine P, Sterkers O, Ferrary E, Grayeli AB. Glucocorticoids inhibit diastrophic dysplasia sulfate transporter activity in otosclerosis by interleukin-6. Laryngoscope. 2006. 116:1647–1650.

8. Hastbacka J, de la Chapelle A, Mahtani MM, Clines G, Reeve-Daly MP, Daly M, Hamilton BA, Kusumi K, Trivedi B, Weaver A, Coloma A, Lovett M, Buckler A, Kaitila I, Lander ES. The diastrophic dysplasia gene encodes a novel sulfate transporter: positional cloning by fine-structure linkage disequilibrium mapping. Cell. 1994. 78:1073–1087.

9. Rossi A, Bonaventure J, Delezoide AL, Cetta G, Superti-Furga A. Undersulfation of proteoglycans synthesized by chondrocytes from a patient with achondrogenesis type 1B homozygous for an L483P substitution in the diastrophic dysplasia sulfate transporter. J Biol Chem. 1996. 271:18456–18464.

10. Forlino A, Piazza R, Tiveron C, Della Torre S, Tatangelo L, Bonafe L, Gualeni B, Romano A, Pecora F, Superti-Furga A, Cetta G, Rossi A. A diastrophic dysplasia sulfate transporter (SLC26A2) mutant mouse: morphological and biochemical characterization of the resulting chondrodysplasia phenotype. Hum Molec Genet. 2005. 14:859–871.

11. Hastbacka J, Superti-Furga A, Wilcox WR, Rimoin DL, Cohn DH, Lander ES. Atelosteogenesis type II is caused by mutations in the diastrophic dysplasia sulfate-transporter gene (DTDST): evidence for a phenotypic series involving three chondrodysplasias. Am J Hum Genet. 1996. 58:255–262.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download