Abstract
The purpose of this study is to evaluate the predictive capability of anorectal physiologic tests for unfavorable outcomes prior to the initiation of biofeedback therapy in patients with dyssynergic defecation. We analyzed a total of 80 consecutive patients who received biofeedback therapy for chronic idiopathic functional constipation with dyssynergic defecation. After classifying the patients into two groups (responders and non-responders), univariate and multivariate analyses were performed to determine the predictors associated with the responsiveness to biofeedback therapy. Of the 80 patients, 63 (78.7%) responded to biofeedback therapy and 17 (21.3%) did not. On univariate analysis, the inability to evacuate an intrarectal balloon (P=0.028), higher rectal volume for first, urgent, and maximal sensation (P=0.023, P=0.008, P=0.007, respectively), and increased anorectal angle during squeeze (P=0.020) were associated with poor outcomes. On multivariate analysis, the inability to evacuate an intrarectal balloon (P=0.018) and increased anorectal angle during squeeze (P=0.029) were both found to be independently associated with a lack of response to biofeedback therapy. Our data show that the two anorectal physiologic test factors are associated with poor response to biofeedback therapy for patients with dyssynergic defecation. These findings may assist physicians in predicting the responsiveness to therapy for this patient population.
Dyssynergic defecation has been recognized as a major cause of chronic functional constipation (1). Dyssynergic defecation entails failure of relaxation of the puborectalis and external anal sphincter muscles, or their paradoxical contraction during straining to defecate, and is associated with difficult or impossible defecation. It was frequently termed anismus (1) or spastic pelvic floor syndrome, or pelvic outlet obstruction. Pelvic floor is a complex muscular apparatus that serves three important functions: defecation, micturition, and sexual function. All-encompassing terms, such as "pelvic floor dyssynergia" or "pelvic outlet obstruction", imply that this problem affects most of the pelvic floor, and possibly all of its functions. Most constipated patients do not report sexual or urinary symptoms. Hence, these terms are not suitable. A consensus report from an international group of experts has recommended that the term "dyssynergic defecation" most aptly describes this form of constipation; we also used it in this study (2, 3).
Biofeedback therapy is considered an effective treatment for chronic constipation, particularly in patients with dyssynergic defecation compared to those with slow transit time, and is widely employed (4). Since Bleijenberg and Kuijpers first described the use of biofeedback therapy to treat dyssynergic defecation in 1987 (5), many other authors have reported improvements of dyssynergic defecation following therapy in their patients (6). Despite these encouraging reports, a significant proportion of patients with dyssynergic defecation still fail to respond. To date, there have been only a few reports regarding those clinical factors that may predict unfavorable outcomes. Several factors, such as a long history of constipation (7), anal canal hypertonia (8), and a long anal canal with increased rectal maximum tolerable volume (9), are known to be associated with poor response to biofeedback therapy; however, no current consensus exists and more studies are needed to clarify these risk factors for unfavorable outcomes. Accordingly, the aim of this study is to evaluate the predictive capability of the balloon expulsion test, anorectal manometry, and defecogram for unfavorable outcomes in biofeedback prior to the initiation of therapy in patients with dyssynergic defecation.
Among 180 consecutive patients who underwent biofeedback therapy at Yonsei University Hospital, Seoul, Korea between October 2004 and April 2009, 36 patients complained of only fecal incontinence and 22 complained of both dyssynergic defecation and fecal incontinence. Because fecal incontinence can influence results of anorectal manometry, we excluded these patients. Fifteen patients who had only delayed colonic transit time or organic disease such as Hirschsprung's disease were also excluded (10). The other 27 patients did not received enough biofeedback therapy (more than four occasions) (11). The remaining 80 patients with dyssynergic defecation were included in this study. Constipation was defined using the Rome III diagnostic criteria and the diagnosis of dyssynergic defecation was confirmed based on one or more of the following criteria: 1) impaired anal relaxation during straining by manometric evaluation (1, 12), 2) no increase in anorectal angle during defecation, and 3) incomplete evacuation of barium on defecogram (10, 13, 14).
All patients were evaluated by history, physical, and laboratory studies to exclude secondary causes of constipation, including hypothyroidism, rheumatologic disorders, or drug side effects. This study was approved by the Institutional Review Board of Severance Hospital (2-2009-0348).
A 3.5 cm latex balloon filled with 50 mL of warm water was inserted into the lower rectum through 3 mm-diameter tubing attached to the balloon. The patient was asked to attempt to expel the balloon in the left lateral decubitus position or into a toilet. Inability to evacuate the intrarectal balloon was defined as an attempt with expulsion failure for five minutes.
Anorectal manometry was performed using a standard low-compliance water perfusion system (0.1 mL/min perfusion rate; Mui Scientific, Missisauga, Ontrario, Canada) and an eight-channel catheter (Zinetics Manometric Catheter, Medtronic Inc., Minneapolis, MN, USA) with a latex balloon (Arndorfer Inc., Greendale, WI, USA) on its tip. The catheter (4.5 mm external diameter) had four radial channels below the balloon and four spiral channels. The performance protocol included the stationary pull-through technique in 1 cm increments while recording anal canal length, resting anal sphincter pressure, and maximal squeezing pressure. Pressures were recorded using a computerized recording device (POLYGRAM NET, Medtronic Inc., Minneapolis, MN, USA). Rectal volume was examined by balloon distension in the rectum. A balloon was inserted into the rectum and inflated in 20 mL increments, up to 250 mL, to assess the threshold volume for the first and urgent sensation to defecate as well as maximal tolerable sensation. The recto-anal inhibitory reflex was also assessed to exclude Hirschsprung's disease.
With the patient in the left lateral decubitus position, the rectum was filled with barium paste, and the patient was seated upright on a specially designed commode before being asked to empty the rectum as rapidly and completely as possible. Plain radiography were taken under fluoroscopic control. Anorectal angles during rest, squeeze, and defecation were measured using the central axis method. Perineal descent was measured as the vertical distance between the anorectal junction and the pubococcygeal line. Anal diameter during defecation was also measured. A normal defecographic pattern was defined as rapid and complete evacuation of contrast material with both increased anorectal angle and normal opening of the anal canal (8).
Biofeedback therapy was performed using the Kontinence™ Clinical HMT2000 (HMT Inc., Seoul, Korea) with anorectal electromyography (EMG) sensor and surface electrodes. The treatment protocol included twice weekly sessions, lasting longer than 40 min each, for five weeks in the outpatient clinic. A deta-iled description of the procedure follows. While the patient was seated on a commode, an anorectal EMG electrode was placed in the anus to monitor muscular activity in the external anal sphincter and puborectalis muscle during rest, squeezing, and relaxing. Surface electrodes were attached to the abdominal wall to detect abdominal wall muscle contraction. The electrical activity of the sphincter appeared as a fluctuating light bar. Patients were taught to squeeze and relax their anal muscles while watching the EMG signals on the monitor. Episodes of bowel movements, satisfaction score and incomplete defecation score were evaluated by a questionnaire prior to each session (15). The satisfaction score was scaled from 0 (dissatisfaction) to 10 (full satisfaction) (15). The incomplete defecation score was scaled from 0 (absent incomplete defecation) to 10 (severe incomplete defecation). Biofeedback therapy was considered successful, and patients were considered responders, if the following criteria were satisfied: 1) bowel frequency increased to three or more episodes per week (9) and 2) increase of satisfaction score of five or more, or 3) decrease of incomplete evacuation score of five or more (15). After classifying the patients into responders and non-responders, as assessed by subjective and objective parameters, univariate and multivariate analyses were performed to evaluate predictors associated with the responsiveness of biofeedback therapy.
Statistical analysis was performed with SPSS 12.0 (Statistical Package for the Social Sciences for Windows, Chicago, IL, USA) using the independent t-test for continuous variables and the chi-square and Fisher's exact tests for dichotomous variables (univariate analysis). Logistic regression was used for multivariate analysis. P values <0.05 were considered to be statistically significant.
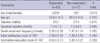
The mean symptom duration of the 80 patients was 7.2 yr (range, 1-25 yr) and the mean bowel movement frequency was 2.3 per week. No significant biofeedback related complications were identified. Of the 80 patients (32 male, 48 female), 63 (78.7%) responded to biofeedback therapy and 17 (21.3%) did not. There was no significant difference in demographic profiles or other characteristics, including symptom duration and bowel movement frequency, between responders and non-responders (Table 1).
Of the 39 patients who successfully expelled the balloon, four (10.3%) did not respond to biofeedback therapy. Of the 41 patients who failed to expel the balloon, 13 (31.7%) did not respond to biofeedback therapy. The inability to evacuate an intrarectal balloon on the balloon expulsion test was significantly related to failure of biofeedback therapy (P=0.028).
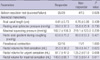
The response to biofeedback therapy was not influenced by anal canal length, resting anal sphincter pressure, maximal squeezing pressure, or recto-anal gradient during coughing (Table 1). Paradoxical contraction also did not influence the results of biofeedback therapy. However, the rectal volume for first, urgent, and maximal sensation was significantly higher in non-responders than responders (59.4±44.7 vs. 35.0±36.2 mL; P=0.023, 125.2±61.0 vs. 87.7±47.0 mL; P=0.008, 197.5±64.4 vs. 149.0±66.1 mL; P=0.011, respectively) (Table 2).
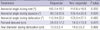
The anorectal angle during the squeeze increased in non-responders compared to responders (106.4±32.8° vs. 89.2±20.6°; P=0.020). The anorectal angles during rest and defecation were not significantly different between groups. Neither perineal descent nor anal diameter during defecation were related to the response to biofeedback (Table 3).
Multivariate analysis was performed for those variables significant in univariate analysis. Inability to evacuate an intrarectal balloon (odds ratio=7.51, P=0.018) and increased anorectal angle during squeeze (odds ratio=1.03, P=0.029) were found to be the factors independently associated with failure to respond to biofeedback therapy.
In defining dyssynergia defecation, most published studies have used arbitrary or symptomatic diagnostic criteria. The recent criteria for dyssynergic defecation (3, 16) appears more suitable for selecting dyssynergic defecation patients because the presence of constipation symptoms together with dyssynergic pattern of defecation and at least one additional abnormal test (e.g., prolonged balloon expulsion time, prolonged colonic transit, or excessive barium retention with defecography) shows a high diagnostic yield in identifying dyssynergic defecation (3, 17). Although most patients enrolled in our study satisfied Rome III criteria and demonstrated dyssynergia on manometric examination, we acknowledge that this is a retrospectively designed study and our enrollment criteria correspond to the criteria used in many previous studies, but not the recent criteria. There were some patients who did not undergo a colon transit time study or barium evacuation study during defecogram. Moreover, the criteria for the balloon expulsion test was 5 min in our study like many other studies (4). Recently, 5 min criteria also changed to those with 1 min (3). These recent criteria will definitely play an important role in designing the next prospective study because they define dyssynergic defecation more properly.
Biofeedback therapy is an effective treatment option for chronic constipation. Prior to the introduction of biofeedback therapy, anal myectomy, subtotal colectomy, and colostomy had been attempted with limited success. Since Bleijenberg and Kuijpers (5) initially reported the resolution of symptoms in patients with dyssynergic defecation following biofeedback therapy, numerous subsequent studies have reported good outcomes with this therapy (18, 19). Biofeedback therapy may be performed in the hospital setting (10) or in the home to reinforce the initial training for an extended period (6). We performed EMG-based biofeedback, which was reported to be more effective than other methods (20), in the outpatient clinic. Home therapy was not offered due to limited equipment availability. Instead, patients were instructed to perform exercises twice daily for ten minutes, alternating five-second squeeze and ten-second resting intervals. We included 80 patients who performed biofeedback therapy on more than four occasions as the success rate has been shown to improve significantly after five or more sessions. According to the study of Gililand et al. (11), only 18% of patients who had between two and four sessions achieved complete success, compared to 44% of those who had five or more.
Many studies have reported an improvement of symptoms, including degree of straining, bowel satisfaction and effective straining following biofeedback therapy, and have considered these to be criteria for success. Recently, there have been randomized prospective trials about biofeedback therapy in constipation. Chiarioni et al. (21) used the degree of global improvement of symptom as a response criteria (primary outcome) and classified it into five grades (worse, no improvement, mild, fair, and major improvement). Heymen et al. (22) asked patients whether they had experienced adequate relief of constipation and used it as a primary outcome. Rao et al. (23) included not only the grade of global satisfaction, but also the number of complete spontaneous bowel movements, balloon expulsion time, and presence of dyssynergia measured by physiologic tests in primary response criteria. In these recent studies, one of the main response criteria of biofeedback was global symptom improvement which was measured in different scales. Considering that constipation is a symptom-based disorder, these criteria appear reasonable and we also included the degree of symptom improvements (satisfaction score and incomplete defecation score) in our main response criteria for dyssynergic defecation. However, only symptom-based criteria are entirely dependent on patients' subjective measurements and may therefore be arbitrary. Thus, many previous studies have compared bowel frequencies before and after treatment (14) and considered a bowel frequency increase up to three or more episodes per week as an objective criterion (9). Accordingly, in the present study, biofeedback therapy was considered successful (responders) if both subjective (satisfaction score or incomplete evacuation score) and objective parameters (bowel frequency ≥3/week) were satisfied like other studies.
In the current study, there were no significant differences between responders and non-responders in demographic or clinical characteristics. The results showed that the inability to evacuate an intrarectal balloon on the balloon expulsion test was related to the failure of biofeedback therapy. Several previously published studies using various expulsion tests have also demonstrated that impaired expulsion capacity is related to poor treatment outcomes (24, 25). The reason for these results is unclear; however, because the severity of defecatory dysfunction was evaluated by means of the balloon expulsion test (25), we speculate that severe defecatory dysfunction prior to biofeedback therapy is related to treatment failure. According to Mckee et al. (26), biofeedback was not helpful in patients who had deranged pelvic floor physiology. These patients probably sustained neurological damage to the pelvic floor during childbirth. Snooks et al. (27) described the separate innervations of the puborectalis and external sphincter, and suggested that damage to more than one innervations in some constipated patients may occur rather than pudendal neuropathy alone. This study indicates that differential damages to the nerves and muscles of the pelvic floor can occur, leading to problems with defecation due to disordered pelvic floor contraction in some individuals. If this damage is severe, it may not be possible to improve the situation with biofeedback training. It also seems to be logical that biofeedback is unsuccessful in patients with severely blunted rectal sensation since functioning sensory afferents are presumably required to detect rectal fullness and the need for defecation. The findings above are consistent with our findings that more severe patients responded less frequently to biofeedback therapy. In the current study, the results suggest that many patients who fail to expel the balloon are likely to be non-responders and should therefore be recommended more intensive biofeedback therapy or alternative treatments. There have also been several reports suggesting that the balloon expulsion test does not predict the responsiveness to biofeedback therapy (4, 9). The difference in results among studies seems to be related to heterogenous patient populations, different success criteria, and varying biofeedback techniques. Further studies regarding the relationship between the balloon expulsion test and biofeedback therapy are needed.
Compared with previous studies suggesting that parameters of defecogram were not related to outcomes of biofeedback therapy (8, 16), our study showed that the anorectal angle duringsqueeze (106.4±32.8°) significantly increased in non-responders. Normally, the anorectal angle on defecogram at rest has a range of 92-114° and is more obtuse during defecation (110-180°) and more acute during squeeze (75-90°) (28). The results suggest that the anorectal angle duringsqueeze reflects the possibility of improvement in the puborectalis muscle following biofeedback therapy.
Rhee et al. (9) reported that anal canal length and rectal maximum tolerable volume were associated with poor response to biofeedback therapy. In that study, anal canal length was longer and rectal maximal tolerable volume increased in non-responders compared to responders (9). However, in the current study, anal canal length yielded no predictive value. The rectal maximal tolerable volume, as well as rectal volume for first and urgent sensation, was significant upon univariate analysis, but did not remain so upon multivariate analysis. The term rectal hyposensitivity, defined as the elevation of sensory thresholds beyond the normal range, relates to impaired or blunted rectal sensory function. Although the mechanism for the development of constipation in patients with rectal hyposensitivity is not entirely clear, it has been classified as one of the principal physiologic abnormalities in patients with functional constipation (29). Jung et al. (30) reported that patients with a more hyposensitive rectum showed non-response to biofeedback more frequently, suggesting rectal hyposensitivity was an important factor in biofeedback therapy responsiveness. Our results also showed the rectal volumes were higher in non-responders upon univariate analysis and further studies regarding the relationship between rectal hyposensitivity and biofeedback therapy are needed.
It has previously been reported that a long duration of constipation (7) and basal anal hypertonia (8) are associated with a poor response to biofeedback therapy in constipated patients. However, there were no significant differences between responders and non-responders in the current study and several reports are in agreement with our findings (15, 25).
The present study has several limitations. First, it was a retrospective analysis which may potentially lead to limitations due to the investigational design. Second, a relatively small sample size was included in this study. Finally, although the biofeedback training procedures used in this study are representative of what has been described in the literature, techniques and equipment used by some laboratories differ from ours. To overcome these limitations, a large-scale prospective study with a standard method and equipment is warranted.
In conclusion, our data show that the inability to evacuate an intrarectal balloon and increased anorectal angle during squeeze are associated with poor response to biofeedback therapy for patients with dyssynergic defecation. These findings may assist physicians in predicting the responsiveness to therapy for this patient population.
Figures and Tables
Table 1
Comparison of the clinical characteristics of responders and non-responders with dyssynergic defecation
References
2. Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterlogy. 2006. 130:1510–1518.

3. Rao SS. Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am. 2008. 37:569–586.

4. Chiarioni G, Salandini L, Whitehead WE. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology. 2005. 129:86–97.

5. Bleijenberg G, Kuijpers HC. Treatment of the spastic pelvic floor syndrome with biofeedback. Dis Colon Rectum. 1987. 30:108–111.

6. Kawimbe B, Papachrysostomou M, Binnie N. Outlet obstruction constipation (anismus) managed by biofeedback. Gut. 1991. 32:1175–1179.

7. Siproudhis L, Dautreme S, Ropert A, Briand H, Renet C, Beusnel C, Juguet F, Rabot AF, Bretagne JF, Gossenlin M. Anismus and biofeedback: who benefits? Eur J Gastroenterol Hepatol. 1995. 7:547–552.
8. Park UC, Choi SK, Piccirillo MF, Verzaro R, Wexner SD. Patterns of anismus and the relation to biofeedback therapy. Dis Colon Rectum. 1996. 39:768–773.

9. Rhee PL, Choi MS, Kim YH, Son HJ, Kim JJ, Koh KC, Paik SW, Rhee JC, Choi KW. An increased rectal maximum tolerable volume and long anal canal are associated with poor short-term response to biofeedback therapy for patients with anismus with decreased bowel frequency and normal colonic transit time. Dis Colon Rectum. 2000. 43:1405–1411.

10. Papachrysostomou M, Smith AN. Effects of biofeedback on obstructive defecation-reconditioning of the defecation reflex? Gut. 1994. 35:252–256.

11. Gilliland R, Heymen S, Altomare DF, Park UC, Vickers D, Wexner SD. Outcome and predictors of success of biofeedback for constipation. Br J Surg. 1997. 84:1123–1126.

12. Jones PN, Lubowski DZ, Swash M, Henry MM. Is paradoxical contraction of puborectalis muscle of functional importance? Dis Colon Rectum. 1987. 30:667–670.

13. Wexner SD, Cheape JD, Jorge JM, Heymen S, Jagelman DG. Prospective assessment of biofeedback for the treatment of paradoxical puborectalis contraction. Dis Colon Rectum. 1992. 35:145–150.

14. Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol. 1998. 93:1042–1050.

15. Park DH, Myung SJ, Yoon IJ, Kwon OR, Ko JE, Chang HS, Yang SK, Kim TH, Song HK, Lee JH, Jung HY, Hong WS, Kim JH, Min YI. Clinical factors associated with response to biofeedback therapy for patients with chronic constipation. Korean J Gastroenterol. 2003. 42:289–296.
16. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006. 130:1480–1491.

17. Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastroenterol Clin North Am. 2007. 36:687–711.

18. Turnbull GK, Ritvo PG. Anal sphincter biofeedback relaxation treatment for women with intractable constipation symptoms. Dis Colon Rectum. 1992. 35:530–536.

19. Fleshman JW, Dreznik Z, Meyer K. Outpatient protocol for feedback therapy of pelvic floor outlet obstruction. Dis Colon Rectum. 1992. 35:1–7.
20. Bleijenberg G, Kuijpers HC. Biofeedback treatment of constipation: a comparison of two methods. Am J Gastroenterol. 1994. 89:1021–1026.
21. Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006. 130:657–664.

22. Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007. 50:428–441.

23. Rao SS, Seaton K, Miller M, Brown K, Nygaard I, Stumbo P, Zimmerman B, Schulze K. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007. 5:331–338.

24. Loening-Baucke V. Factors determining outcome in children with chronic constipation and faecal soiling. Gut. 1989. 30:999–1006.

25. Fernandez-Fraga X, Azpiroz F, Casaus M, Aparici A, Malagelada JR. Responses of anal constipation to biofeedback treatment. Scand J Gastroenterol. 2005. 40:20–27.
26. McKee RF, McEnroe L, Anderson JH, Finlay IG. Identification of patients likely to benefit from biofeedback for outlet obstruction constipation. Br J Surg. 1999. 86:355–359.

27. Snooks SJ, Barnes PR, Swash M, Henry MM. Damage to the innervations of the pelvic floor musculature in chronic constipation. Gastroenterology. 1985. 89:977–981.
28. Brennan D, Williams G, Kruskal J. Practical performance of defecography for the evaluation of constipation and incontinence. Semin Ultrasound CT MR. 2008. 29:420–426.

29. Gladman MA, Lunniss PJ, Scott SM, Swash M. Rectal hyposensitivity. Am J Gastroenterol. 2006. 101:1140–1151.

30. Jung KW, Myung SJ, Byeon JS, Yoon IJ, Ko JE, Seo SY, Yoon SM, Do MY, Kim DH, Kwon SH, Ye BD, Jung HY, Yang SK, Kim JH. Response to biofeedback therapy for pateints with rectal hyposensitivity. Intest Res. 2008. 6:56–69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download