Abstract
To characterize the association between chronic kidney disease (CKD), mortality, severity of coronary artery disease (CAD), treatment modality of CAD, and type of coronary stents among patients undergoing coronary angiography (CAG), we retrospectively reviewed the electronic medical records of the patients who underwent CAG at Seoul National University Bundang Hospital in Korea between May 2003 and January 2006. CKD was staged using an estimated glomerular filtration rate (eGFR) from the creatinine value prior to CAG. There were 3,637 patients included. The presence of CAD was 48% in CKD stage 1, 61% in stage 2, 73% in stage 3, 87% in stage 4, and 81% in stage 5. Survival rate gradually diminished for patients with decreasing renal function. No significant differences in all-cause and cardiac mortality were observed by medical treatment, PCI or CABG, in CKD patients with an eGFR less than 60 mL/min/1.73 m2. CKD patients with drug-eluting stents showed significantly lower all-cause mortality (5.4% vs. 13.3%) and incidence of myocardial infarction (1.7% vs. 10%) than those with bare metal stents. In conclusion, an eGFR is a strong independent prognostic marker among patients undergoing CAG and the severity of CAD increases progressively with worsening renal function.
It is well known that cardiovascular disease is the number one cause of death among patients with end-stage renal disease (1). In Korea, cardiovascular disease accounted for over 30% of the 1,256 overall deaths among dialysis patients in 2005 (2). However, cardiovascular risk is not limited to end-stage renal disease, and risk of cardiovascular mortality begins to increase with even mild impairment of kidney function (3, 4). This increased risk of cardiovascular mortality in patients with chronic kidney disease (CKD) seems to be caused by non-traditional risk factors such as anemia, altered calcium phosphorus metabolism, inflammation and oxidative stress, as well as traditional risk factors such as hypertension, smoking, diabetes, dyslipidemia and left ventricular hypertrophy (5).
Most studies showing an association between kidney function and mortality have assessed renal function by measuring only serum creatinine without an estimate of the glomerular filtration rate (eGFR) (6, 7) or have provided a rough categorization of renal function based on the eGFR (8). Furthermore, in previous studies patients were not stratified by the severity of coronary artery disease (CAD) to determine the independent effect of renal function on mortality. Therefore, a graded relationship between cardiovascular risk and eGFR needs to be defined after adjustment for the severity of CAD.
High prevalence of coronary artery plaques in dialysis patients has been documented (9, 10). However, few prior studies have examined the direct association between coronary anatomy and CKD that does not require dialysis. One meta-analysis suggested that there was no association (11), while some other studies suggested there was a relationship (12, 13). It is important to explore whether the severity of CKD is associated with the severity of CAD.
The optimal therapeutic modality in CKD patients with CAD has not been defined. Despite established awareness of high cardiovascular risk in CKD patients, these patients encounter "therapeutic nihilism", in which there is a lack of appropriate medication and intervention (14). Some retrospective analyses showed improved long-term survival and reduced rates of repeated revascularization procedures by using a coronary artery bypass graft (CABG) rather than percutaneous coronary intervention (PCI) in patients with CKD (15-17). Although long-term mortality is increased, it appears that the results of PCI in CKD patients are now comparable to the results in the general population (18). It is important to investigate the clinical outcomes of CKD patients with CAD across treatment strategies. Moreover, the efficacy of drug-eluting stents for the treatment of CAD in CKD patients remains unproven.
The purpose of this study is to investigate the relationship between renal function and clinical outcome among patients undergoing coronary angiography (CAG), using categorized adjustments in the classification of renal function according to CKD stage in compliance with the National Kidney Foundation K/DOQI guidelines (19). In addition, we investigated whether CKD stage affected severity in the pathology of CAD. Finally, we evaluated the clinical outcomes of CKD patients with an eGFR less than 60 mL/min/1.73 m2 stratified according to treatment modality and type of stent.
The electronic medical records of patients who underwent CAG for the evaluation of CAD at Seoul National University Bundang Hospital in Korea between May 2003 and January 2006 were retrospectively reviewed. Patients with valvular heart disease, congenital heart disease, or cardiomyopathy were excluded from this analysis.
Clinical characteristics at the time of CAG were collected: a number of clinical risk factors, including age, sex, smoking, and the presence of the following medical conditions: hypertension, dyslipidemia, cerebrovascular disease, peripheral vascular disease, congestive heart failure, diabetes, and prior myocardial infarction. Laboratory data and current medications were also reviewed. The presence of regional wall motion abnormality was determined, and left ventricular ejection fraction (EF) was measured by echocardiography. The extent of vessel disease was defined by the number of major coronary arteries with luminal narrowing ≥50% by visual estimation. Major coronary arteries included left anterior descending artery, left circumflex artery, and right coronary artery. Assignment to either PCI or CABG was made on the basis of the initial revascularization procedure after CAG. Patients whose initial treatment did not include either PCI or CABG were referred to medical therapy. The primary clinical outcome of this study was all-cause mortality. Major adverse cardiac events (MACE), such as restenosis at a follow-up CAG, myocardial infarction, or target vessel revascularization (TVR), were also examined. Subgroup analysis was also performed for patients with an eGFR less than 60 mL/min/1.73 m2. In these patients, clinical outcomes were compared depending on the treatment modality or the type of stent implanted.
The most recent creatinine measurement prior to CAG was used (average, 31.7±91.8 days). Renal function was calculated by the simplified Modification of Diet in Renal Disease (MDRD) equation (20) and categorized according to CKD stage in compliance with the National Kidney Foundation K/DOQI guidelines (19). Patients in CKD stage 1 had normal renal function. Patients with CKD indicated those belonged to CKD stage 3, 4, and 5 with an eGFR less than 60 mL/min/ 1.73 m2.
The clinical characteristics of the patients are presented as mean±SD for continuous variables and as percentages for categorical variables. ANOVA and chi-square analyses were performed for continuous and categorical variables, respectively. p value less than 0.05 were considered statistically significant. Survival time was calculated from the date of CAG to the date on which the data were censored or all-cause mortality occurred. Data were censored if follow-up ended or the patient was still alive at the end of the study. The cumulative survival rates in each CKD stage were estimated by the Kaplan-Meier method, and the differences in survival rates between stages were evaluated by log-rank (Mantle-Cox) method. Cox proportional hazards analysis was used to determine the effect of renal function on survival after adjusting for other risk factors. Variables univariately associated with the outcome (p< 0.05) were entered into the multivariable model using stepwise selection. Statistical analyses were performed using SPSS (version 15.0. for Windows; SPSS Inc, Chicago, IL, U.S.A.).
Three thousand, seventy hundred thirty eight cases of CAG were performed during this period. Ninety seven cases were repeated CAGs in the same patients. Four patients had no measurement of serum creatinine. A total of 3,637 patients were included in this analysis. Baseline clinical characteristics are shown in Table 1. Of all the patients included, 1,102 patients belonged to CKD stage 1 with normal renal function, 1,632 patients were in stage 2, 838 were in stage 3, 61 were in stage 4, and 104 patients were in stage 5. In total, 27.6% of the patients were included in CKD stages 3/4/5 with an eGFR less than 60 mL/min/1.73 m2. Compared with patients with normal renal function, patients with CKD were older, more often female, and more likely to have comorbid medical conditions such as hypertension, cerebrovascular disease, peripheral vascular disease, congestive heart failure, diabetes, and prior myocardial infarction. In the echocardiographic findings, more frequent regional wall motion abnormality and lower left ventricular EF were observed as renal function worsened. In the laboratory findings, patients with CKD showed lower hemoglobin, lower albumin, and lower cholesterol levels. However, C-reactive protein level increased as CKD stage increased. Among patients with normal renal function, 68.2% were managed medically, 27.8% underwent PCI, and only 4% were treated with CABG. As the severity of CKD increased, PCI and CABG were chosen more often than medical treatment. Erythropoietin, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers were prescribed more frequently to the patients in CKD stages 4/5 than to the patients in CKD stages 1/2.
The presence of CAD with involvement of more than one vessel was 48% in CKD stage 1, 61% in stage 2, 73% in stage 3, 87% in stage 4, and 81% in stage 5 (Table 2). A significant tendency for the presence of CAD was revealed as eGFR declined. Although the effects were not statistically significant across patients in different CKD stages, three-vessel disease and left main disease seemed to be more frequent in patients in CKD stages 4/5 than those in CKD stage 1/2.
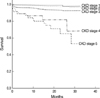
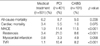
Fig. 1 shows the survival curve of the patients by stage of CKD. Mean duration of follow-up in theses patients was eleven months. Survival rate was greatest for patients with normal renal function and gradually decreased for patients with decreasing renal function. A Cox stepwise multivariate analysis showed that high CKD stage, old age, presence of diabetes, low serum albumin level and high number of involved coronary arteries were independent predictors of all-cause mortality (Table 3). Risk of death increased more than six-fold in patients with stage 5, more than three-fold in patients with stage 4, and 2.5-fold in patients with stage 3 as compared to patients with normal renal function. Stage 2 CKD seemed to be associated with increasing risk of mortality, but the relationship did not reach statistical significance as an independent predictor.
Clinical outcomes stratified according to each treatment modality in CKD patients with an eGFR less than 60 mL/min/1.73 m2 were evaluated (Table 4). PCI was done in 401 patients, CABG was done in 101 patients, and 501 patients received medical treatment only. No significant differences in all-cause and cardiac mortality were observed among these three groups. The frequency of MACE, including restenosis and TVR, was statistically higher in the PCI and CABG groups than in the medical treatment group.
Next, we investigated whether the type of stent used affected clinical outcomes in CKD patients with an eGFR less than 60 mL/min/1.73 m2 (Table 5). In this group of patients, drug-eluting stents were implanted much more frequently than bare metal stents (312 vs. 60). CKD patients with drug-eluting stents showed significantly lower rates of all-cause mortality than those with bare metal stents (5.4% vs. 13.3%). However, there were no statistically significant differences by type of stent for cardiac mortality. For MACE, only the incidence of myocardial infarction was significantly less frequent in the drug-eluting stents group than in the bare metal stents group (1.7% vs. 10%).
We characterized the severity of CAD and clinical outcome according to the degree of kidney function based on the data from more than 3,600 patients. Our results revealed that patients with the higher-stage CKD had more severe CAD and worse clinical outcomes than those in the lower stages of CKD. CKD stage was the strongest predictor of all-cause mortality in patients who underwent CAG. Treatment with PCI or CABG was associated with more adverse cardiovascular events than medical treatment in CKD patients with an eGFR less than 60 mL/min/1.73 m2. In this group of patients, drug-eluting stents significantly reduced all-cause mortality and recurrence of myocardial infarction as compared with bare metal stents.
From the baseline characteristics of the more than 3,600 patients in this study, patients with decreased renal function tended to have more comorbid medical conditions and more severe cardiac dysfunction. These findings are consistent with previous studies (5, 16, 21). This clustering of significant cardiovascular risk factors and comorbidities in CKD patients likely contributed to the severity of CAD and elevated mortality. Lower hemoglobin levels in CKD stages 4/5 patients seemed to be caused by reduced production of erythropoietin as renal function deteriorates. High C-reactive protein in our CKD patients suggests a proinflammatory state, which is associated with increased cardiovascular risk (22, 23). The laboratory findings in this study might represent an association between non-traditional cardiovascular risk factors and poor outcomes in CKD (24, 25). Erythropoietin was prescribed to our CKD patients due to renal anemia. Some studies reported that CKD patients with CAD showed a tendency for aspirin, β-blockers and statins to be underused, probably due to concerns about limited efficacy and toxic effects in renal dysfunction (26, 27). However, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers were more frequently prescribed in our CKD patients, so we can at least exclude the possibility of worse clinical outcomes in CKD due to inadequate use of medications.
There were reports showing an increase in rates of CAD in the presence of CKD (12, 13), but the sample size was small, and both studies were conducted on selected populations. Additionally, it has been reported that patients with non-dialysis-dependent CKD have more severe coronary lesions than those with normal kidney function (28). However, this finding might reflect selection bias because dialysis patients were less likely to have severe coronary anatomy than those with non-dialysis-dependent CKD. Chonchol et al. (29) recently reported a significant relationship between CKD and angiographic CAD in 261 male patients with positive nuclear imaging studies. They also showed that CKD patients were more likely to have three-vessel or left main disease. In contrast to our study, their study cohort included only males and neglected many important cardiovascular risk factors. In this study, we compared the angiographic findings of more than 3,600 patients, including over 1,000 CKD patients with an eGFR less than 60 mL/min/1.73 m2. We found that the severity of CAD was directly proportional to the degree of renal dysfunction, and CKD patients have a high prevalence of angiographic CAD. Our results support the findings showing a strong association between cardiovascular mortality and CKD (4).
Although variables such as age, diabetes, serum albumin level, and number of involved coronary arteries are independent predictors of mortality in our population, CKD stage is the strongest predictor. Possible explanations for the increased mortality rate associated with CKD include increased traditional and non-traditional cardiovascular risk factors in these patients, and increased complications from cardiovascular disease when it develops. Despite the increased risk profile of our CKD patients prior to CAG, CKD was independently associated with mortality even after adjusting for these variables. Our results are consistent with previous studies (16, 26, 30). There are also some reports showing a graded inverse relationship between renal function and risk of death (31, 32). Furthermore, renal insufficiency is an independent predictor of increased in-hospital morbidity and mortality after PCI with stent implantation (33). Even after successful PCI, CKD was associated with increased short-term and long-term mortality (19, 34). According to our data and those of others, eGFR is a strong prognostic marker independent of underlying severity of CAD in patients with cardiovascular disease. Therefore, the systemic ascertainment of renal function in all patients with cardiovascular disease should be encouraged.
Most patients with renal dysfunction and acute coronary syndrome have been treated medically rather than by percutaneous or surgical revascularization (21, 35). However, more than half of our CKD patients with an eGFR less than 60 mL/min/1.73 m2 underwent PCI or CABG. The inception point of this study was CAG. Therefore, all the patients who presented with stable angina as well as acute coronary syndrome were included. The optimal treatment strategy with regard to CAD in CKD patients is controversial. Several studies have suggested that CABG is better than or similar to PCI in the clinical outcomes of patients on dialysis (15, 36-38). Subgroup analysis of the arterial revascularization therapies study (ARTS) trial showed that mild to moderate CKD patients with an eGFR around 50 mL/min who were randomly assigned to CABG or PCI showed similar outcomes for both treatments (39, 40). However, Keeley et al. showed that PCI has a better survival rate than CABG or medical treatment for patients with severe CKD and acute coronary syndrome (21). Since cardiac interventions did not worsen long-term renal function (41), more aggressive management of the increased cardiovascular risk in CKD patients should be encouraged. The reason that a certain treatment modality did not provide a survival benefit over another treatment in our CKD patients may stem from the short follow-up period for detecting the differences. Another possible explanation is that the treatments were not randomly assigned; our results might also be biased by the treatment preferences of our hospital.
The recent introduction of drug-eluting stents has dramatically decreased the incidence of restenosis and the need for repeat revascularization (42, 43). Previous studies showed that CKD patients had a higher mortality after PCI with bare metal stents than patients with normal renal function, with no difference in the rates of repeat revascularization (18, 33, 37, 44). The superiority of drug-eluting stents has yet to be established in patients with CKD (45-48). Although there were no differences in the rates of restenosis or TVR, our study showed that drug-eluting stents significantly reduced the rate of all-cause mortality and myocardial infarction. We propose that more frequent use of drug-eluting stents should be recommended to improve the long-term outcomes in patients with renal dysfunction.
Despite the comprehensive nature of this data, there are several limitations to consider in this study. First, our patients are only those who underwent CAG. These patients are a subset of all patients with cardiovascular disease and may not reflect the outcomes of all patients with cardiovascular disease. Second, we defined CKD stage based on an eGFR derived from a single serum creatinine determination rather than on a serum creatinine determination on the day of CAG or a direct measurement of renal function, like iothalamate clearance. In addition, the creatinine value might have been influenced by medications or clinical status. Third, indication bias might have affected the results because the indication for treatment may affect the outcomes. For example, if the presence of CKD influences choice of treatment modality, it may introduce a bias that may also affect clinical outcomes. Fourth, clinical outcome data in patients with an eGFR less than 60 mL/min/1.73 m2 were based on univariate analysis. Further prospective randomized trials are required. Fifth, due to the observational nature of this study, it is not possible to determine a causal relationship between renal function and mortality among patients undergoing CAG. Final limitations include the single-center experience represented by these data.
In summary, we found that among patients undergoing CAG, there is a direct relationship between renal dysfunction and risk of mortality, independent of underlying clinical risk factors. We also showed that the severity of CAD increased progressively with decreasing renal function. In CKD patients, drug-eluting stents showed more favorable clinical outcomes than did bare metal stents.
Figures and Tables
Table 3
Multivariate predictors of all-cause mortality

*Reference CKD stage 1; †Reference insignificnat disease; ‡Adjusted with age, gender, history of diabetes mellitus, history of congestive heart failure, history of any malignant neoplasm, history of previous coronary heart disease, BMI, mean arterial blood pressure, hemoglobin, calcium, phosphorus, uric acid, cholesterol, serum albumin, urine proteinuria 1+ or more by dipstick test, C-Reactive Protein, number of diseased coronary artery, treatment with erythropoietin, type of coronary stent, treatment modality of coronary arterial lesion, CKD stage.
References
1. Atlas of End-Stage Real Disease in the United States. National Institutes of Health, National Institutes of Diabetes and Digestive and Kidney Disease. USRDS 2005 Annual data report. 2005.
2. Korean Society of Nephrology, Registry Committee. Renal Replacement Therapy in Korea. Korean J Nephrol. 2006. 25:Suppl 2. S425–S443.
3. Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002. 13:745–753.

4. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004. 351:1296–1305.

5. Baigent C, Burbury K, Wheeler D. Premature cardiovascular disease in chronic renal failure. Lancet. 2000. 356:147–152.

6. Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med. 2001. 134:629–636.

7. Fried LF, Shlipak MG, Crump C, Bleyer AJ, Gottdiener JS, Kronmal RA, Kuller LH, Newman AB. Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003. 41:1364–1372.

8. Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, Coresh J, Levey AS, Sarnak MJ. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003. 41:47–55.

9. Ansari A, Kaupke CJ, Vaziri ND, Miller R, Barbari A. Cardiac pathology in patients with end-stage renal disease maintained on hemodialysis. Int J Artif Organs. 1993. 16:31–36.

10. Rostand SG, Kirk KA, Rutsky EA. Dialysis-associated ischemic heart disease: insights from coronary angiography. Kidney Int. 1984. 25:653–659.

11. Nicholls SJ, Tuzcu EM, Hsu A, Wolski K, Sipahi I, Schoenhagen P, Crowe T, Kapadia SR, Hazen SL, Nissen SE. Comparison of coronary atherosclerotic volume in patients with glomerular filtration rates <or=60 versus>60 mL/min/1.73 m(2): a meta-analysis of intravascular ultrasound studies. Am J Cardiol. 2007. 99:813–816.
12. Reis SE, Olson MB, Fried L, Reeser V, Mankad S, Pepine CJ, Kerensky R, Merz CN, Sharaf BL, Sopko G, Rogers WJ, Holubkov R. Mild renal insufficiency is associated with angiographic coronary artery disease in women. Circulation. 2002. 105:2826–2829.

13. Ohtake T, Kobayashi S, Moriya H, Negishi K, Okamoto K, Maesato K, Saito S. High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: an angiographic examination. J Am Soc Nephrol. 2005. 16:1141–1148.

14. Anavekar NS, Pfeffer MA. Cardiovascular risk in chronic kidney disease. Kidney Int. 2004. Suppl 92. S11–S15.

15. Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation. 2002. 106:2207–2211.

16. Reddan DN, Szczech LA, Tuttle RH, Shaw LK, Jones RH, Schwab SJ, Smith MS, Califf RM, Mark DB, Owen WF Jr. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003. 14:2373–2380.

17. Reddan DN, Marcus RJ, Owen WF Jr, Szczech LA, Landwehr DM. Long-term outcomes of revascularization for peripheral vascular disease in end-stage renal disease patients. Am J Kidney Dis. 2001. 38:57–63.

18. Best PJ, Berger PB, Davis BR, Grines CL, Sadeghi HM, Williams BA, Willerson JT, Granett JR, Holmes DR Jr. PRESTO Investigators. Impact of mild or moderate chronic kidney disease on the frequency of restenosis: results from the PRESTO trial. J Am Coll Cardiol. 2004. 44:1786–1791.
19. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002. 39:2 Suppl 1. S1–S266.
20. Levey AS, Greene T, Kusek JW, Beck G. A simplified equation to predict glomerular filtration rate from serum creatinine. (Abstract). J Am Soc Nephrol. 2000. 11:A0828.
21. Keeley EC, Kadakia R, Soman S, Borzak S, McCullough PA. Analysis of long-term survival after revascularization in patients with chronic kidney disease presenting with acute coronary syndromes. Am J Cardiol. 2003. 92:509–514.

22. Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000. 342:836–843.

23. Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy RP, Furberg CD, Psaty BM. Cardiovascular disease risk status in elderly persons with renal insufficiency. Kidney Int. 2002. 62:997–1004.

25. Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS, Sarnak MJ. The relationship between nontraditional risk factors and outcomes in individuals with stage 3 to 4 CKD. Am J Kidney Dis. 2008. 51:212–223.

26. Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004. 351:1285–1295.

27. Reddan DN, Szczech L, Bhapkar MV, Moliterno DJ, Califf RM, Ohman EM, Berger PB, Hochman JS, Van de Werf F, Harrington RA, Newby LK. Renal function, concomitant medication use and outcomes following acute coronary syndromes. Nephrol Dial Transplant. 2005. 20:2105–2112.

28. Hemmelgarn BR, Ghali WA, Quan H, Brant R, Norris CM, Taub KJ, Knudtson ML. Poor long-term survival after coronary angiography in patients with renal insufficiency. Am J Kidney Dis. 2001. 37:64–72.

29. Chonchol M, Whittle J, Desbien A, Orner MB, Petersen LA, Kressin NR. Chronic kidney disease is associated with angiographic coronary artery disease. Am J Nephrol. 2008. 28:354–360.

30. Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000. 35:681–689.

31. Beddhu S, Allen-Brady K, Cheung AK, Horne BD, Bair T, Muhlestein JB, Anderson JL. Impact of renal failure on the risk of myocardial infarction and death. Kidney Int. 2002. 62:1776–1783.

32. Hemmelgarn BR, Southern DA, Humphries KH, Culleton BF, Knudtson ML, Ghali WA. Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease (APPROACH) Investigators. Refined characterization of the association between kidney function and mortality in patients undergoing cardiac catheterization. Eur Heart J. 2006. 27:1191–1197.
33. Blackman DJ, Pinto R, Ross JR, Seidelin PH, Ing D, Jackevicius C, Mackie K, Chan C, Dzavik V. Impact of renal insufficiency on outcome after contemporary percutaneous coronary intervention. Am Heart J. 2006. 151:146–152.

34. Papafaklis MI, Naka KK, Papamichael ND, Kolios G, Sioros L, Sclerou V, Katsouras CS, Michalis LK. The impact of renal function on the long-term clinical course of patients who underwent percutaneous coronary intervention. Catheter Cardiovasc Interv. 2007. 69:189–197.

35. Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000. 35:1044–1051.

36. Rinehart AL, Herzog CA, Collins AJ, Flack JM, Ma JZ, Opsahl JA. A comparison of coronary angioplasty and coronary artery bypass grafting outcomes in chronic dialysis patients. Am J Kidney Dis. 1995. 25:281–290.

37. Herzog CA, Ma JZ, Collins AJ. Long-term outcome of dialysis patients in the United States with coronary revascularization procedures. Kidney Int. 1999. 56:324–332.

38. Ivens K, Gradaus F, Heering P, Schoebel FC, Klein M, Schulte HD, Strauer BE, Grabensee B. Myocardial revascularization in patients with end-stage renal disease: comparison of percutaneous transluminal coronary angioplasty and coronary artery bypass grafting. Int Urol Nephrol. 2001. 32:717–723.
39. Aoki J, Ong AT, Hoye A, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, Schönberger JP, Buller N, Bonser R, Lindeboom W, Unger F, Serruys PW. Five year clinical effect of coronary stenting and coronary artery bypass grafting in renal insufficient patients with multivessel coronary artery disease: insights from ARTS trial. Eur Heart J. 2005. 26:1488–1493.

40. Ix JH, Mercado N, Shlipak MG, Lemos PA, Boersma E, Lindeboom W, O'Neill WW, Wijns W, Serruys PW. Association of chronic kidney disease with clinical outcomes after coronary revascularization: the Arterial Revascularization Therapies Study (ARTS). Am Heart J. 2005. 149:512–519.

41. Inrig JK, Patel UD, Briley LP, She L, Gillespie BS, Easton JD, Topol EJ, Szczech LA. Mortality, kidney disease and cardiac procedures following acute coronary syndrome. Nephrol Dial Transplant. 2008. 23:934–940.

42. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, Molnár F, Falotico R. RAVEL Study Group. Randomized Study with the Sirolimus-Coated Bx Velocity Balloon-Expandable Stent in the Treatment of Patients with de Novo Native Coronary Artery Lesions. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002. 346:1773–1780.
43. Degertekin M, Serruys PW, Foley DP, Tanabe K, Regar E, Vos J, Smits PC, van der Giessen WJ, van den Brand M, de Feyter P, Popma JJ. Persistent inhibition of neointimal hyperplasia after sirolimus-eluting stent implantation: long-term (up to 2 years) clinical, angiographic, and intravascular ultrasound follow-up. Circulation. 2002. 106:1610–1613.
44. Nikolsky E, Mehran R, Turcot D, Aymong ED, Mintz GS, Lasic Z, Lansky AJ, Tsounias E, Moses JW, Stone GW, Leon MB, Dangas GD. Impact of chronic kidney disease on prognosis of patients with diabetes mellitus treated with percutaneous coronary intervention. Am J Cardiol. 2004. 94:300–305.

45. Halkin A, Mehran R, Casey CW, Gordon P, Matthews R, Wilson BH, Leon MB, Russell ME, Ellis SG, Stone GW. Impact of moderate renal insufficiency on restenosis and adverse clinical events after paclitaxel-eluting and bare metal stent implantation: results from the TAXUS-IV Trial. Am Heart J. 2005. 150:1163–1170.

46. Lemos PA, Arampatzis CA, Hoye A, Daemen J, Ong AT, Saia F, van der Giessen WJ, McFadden EP, Sianos G, Smits PC, de Feyter P, Hofma SH, van Domburg RT, Serruys PW. Impact of baseline renal function on mortality after percutaneous coronary intervention with sirolimus-eluting stents or bare metal stents. Am J Cardiol. 2005. 95:167–172.





 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download