Abstract
We determined the relationship between the progression of immunoglobulin A nephropathy (IgAN) and the A1818T polymorphism in intron 2 of Angiotensin II type 2 receptor (AT2R) gene, which might play protective roles in the pathogenesis of IgAN. Patients with biopsy-proven IgAN were recruited from the registry of the Progressive REnal disease and Medical Informatics and gEnomics Research (PREMIER) which was sponsored by the Korean Society of Nephrology. A1818T polymorphism of AT2R gene was analyzed with PCR-RFLP method and the association with the progression of IgAN, which was defined as over 50% increase in baseline serum creatinine level, was analyzed with survival analysis. Among the 480 patients followed for more than 10 months, the group without T allele had significantly higher rates of progression of IgAN than the group with T allele (11.4% vs. 3.9%, p=0.024), although there were no significant differences in the baseline variables such as initial serum creatinine level, the degree of proteinuria, and blood pressure. In the Cox's proportional hazard model, the hazard ratio of disease progression in the patients with T allele was 0.221 (95% confidence interval for Exp(B): 0.052-0.940, p=0.041) compared to that of without T allele. In conclusion, A1818T polymorphism of AT2R gene was associated with the progression of IgAN.
Immunoglobulin A nephropathy (IgAN) is the most common type of primary glomerulonephritis in the world among patients undergoing renal biopsy. It is known to be an important cause of end stage renal disease. The actuarial renal survival at 10 yr in adults with IgAN is about 80-85% according to several epidemiologic studies of Asian countries (1-3). Although several clinical factors such as severe proteinuria, arterial hypertension, elevated serum creatinine level (4-6), and the severity of glomerular sclerosis and interstitial fibrosis on the renal pathology (7) have been thought to be related to the progression of IgAN, it is not clear why some of patients develop progressive disease, while the others do not. It has been suggested that genetic factors may contribute not only to the susceptibility to IgAN but also to its progression. There have been so many genetic association studies on the candidate genes of IgAN progression, of which the most widely studied have been polymorphisms of genes involved in the renin-angiotensin system (RAS), including insertion/deletion (I/D) polymorphisms of angiotensin converting enzyme (ACE) gene (10), and angiotensinogen gene polymorphisms (11). However, results of these studies were inconsistent.
Several experimental studies have suggested that as an another important part of the RAS, counter-regulatory to the vasoconstrictor action of the angiotensin II via AT1R, angiotensin II type 2 receptor (AT2R) might have a protective role in the ischemic kidney injury (12) and that tubular expression of AT2R and imbalance to AT1R could be related to the pathogenesis of IgAN (13). Additionally, according to recent association study in type 1 diabetic patients, among the polymorphisms of X-chromosomal AT2R gene, A1818T polymorphism was reported to be related to the kidney function (14). Therefore, we hypothesize that A1818T polymorphism of AT2R gene may be involved in the progression of IgAN.
This study was approved by the Institutional Review Board in Seoul National University Hospital and other participated hospitals before gathering the data. Informed consents were obtained from the patients. The subjects were enrolled in the Progressive REnal disease and Medical Informatics and gEnomics Research (PREMIER) which was sponsored by the Korean Society of Nephrology since August 2003. In PREMIER study, 34 hospitals and clinics in Korea participated. We analyzed the clinical data of 4,406 patients aged 15 yr or more with glomerulonephritis diagnosed by renal biopsy from May 1982 to December 2006. From this registry, 480 patients with primary IgAN, who were over 15 yr old, had a minimum follow up period of 10 months were enrolled in this study. Diagnosis of IgAN was based on established pathologic criteria, including mesangial expansion and the diagnostic presence of IgA as the sole, predominant, or co-dominant immunoglobulin. Patients with evidence of systemic diseases, such as diabetes, chronic liver disease, or systemic lupus erythematosus, were excluded. One hundred healthy, randomly selected, age-matched, normotensive subjects without any evidence of renal disease were also recruited from the Health Promotion Centre of Seoul National University Hospital as control.
The participated researchers had selected candidate patients, and one qualified nurse visited every participated institution to collect the clinical data at the time of renal biopsy and during follow-up visits. We gathered the data of age, gender, body mass index (BMI), blood pressure, serum protein level, serum albumin level, serum cholesterol level, serum uric acid level, serum creatinine level, the degree of proteinuria by spot urine protein creatinine ratio (suPCR) at the time of renal biopsy and medication of RAS inhibitors or steroid during follow-up period. The hypertension was defined as systolic blood pressure (SBP) 140 mmHg or higher, diastolic blood pressure (DBP) 90 mmHg or higher, or taking antihypertensive medication before renal biopsy and the severe proteinuria were defined as more than 3 of suPCR, respectively. The estimated glomerular filtration rate (eGFR) was calculated by the modified MDRD equation (15).
The primary end point was an increase of serum creatinine level by more than 50% of baseline value or initiation of renal replacement therapy for the end stage renal disease. We defined the progressive disease as the group of patients of IgAN reached to the primary end point and stable disease for the others. The follow-up duration was the duration of time between renal biopsy and the primary end point or the last follow-up date.
Genomic DNA was isolated from peripheral blood using a Wizard Genomic DNA Purification Kit (Promega, Madison, WI, U.S.A.), according to the manufacturer's instructions. Genotyping for the A1818T polymorphism of AT2R gene was done using methods previously described (16). Briefly for the region spanning the polymorphism, the minisequencing primers were 5'-CTGTATTTTGCAAAACTCCT-3'and 5'-TTATGTTAATTTGTTAGGTC-3', respectively. The resulting amplicon was digested using Sau961 restriction enzyme (Promega), which recognizes the 1818T allele. The restriction products were then visualized on 2% agarose gels containing ethidium bromide. Confirmation of genotypes was done by direct DNA sequencing using the ABI Prism Big Dye Terminator kit (Applied Biosystems, Foster City, CA, U.S.A.) of 10% of the study population samples. In all cases, the genotype determined by PCR restriction fragment length polymorphism assay was identical to that determined by DNA sequencing.
All data were analyzed using SPSS 12.0 KO for Windows. Mantel-Haenszel chi-square test was used to detect the differences in the genotype distributions of the patients and controls. The Continuous variables were tested by Student's t-test or Mann-Whitney tests and the discrete variables by chi-square test. To test the significance of various prognostic factors related to the disease progression, survival analysis using the log rank test and the Cox's proportional hazards models were carried out. With the Kaplan-Meier analysis, we expressed survivorship curve about the difference between patients with T allele and those without T allele. And then we analyzed the multivariate analysis with Cox's model, adjusted for age, sex, serum creatinine level, the degree of proteinuria (as a continuous variables, and a discrete variable suPCR <3 or ≥3), the presence of hypertension, and decreased renal function at the time of diagnosis.
We investigated A1818T polymorphism in intron 2 of the AT2R gene located on X-chromosome. Table 1 shows the genotype distribution in control and patients groups. The genotype distribution was not different between control and patient groups (χ2=5.111, p=0.078). This finding suggested that A1818T polymorphism of AT2R gene was not associated with susceptibility of IgAN. The genotype distribution in female control group and in female patient group did not deviate from Hardy-Weinberg equilibrium (p>0.05).
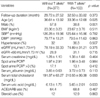
Among 480 patients with biopsy-proven IgAN, progressive disease was observed in 47 patients in 9.8% of the population after a follow-up of 30.33±3.34 months (mean±standard deviation). There was a higher proportion of male patients in patients with progressive disease than in those with stable disease. The well-known indicators of poor renal function, such as lower eGFR and higher serum creatinine level, higher blood pressure, more severe proteinuria were observed in progressive disease group, compared to stable disease group (Table 2). The proportion of patients taking inhibitors of renin-angiotensin systems and that of patients with a history of steroid therapy were not different between 2 groups.
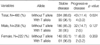
Males were less common in patients group with T allele than in patients group without T allele (38.8% vs. 57.8% respectively, p=0.001) (Table 3). Patients with the T allele were significantly younger at the time of kidney biopsy than those without it (33.36±12.68 vs. 36.61±13.92 respectively, p=0.025) (Table 3). Patients with T allele showed lower serum uric acid than those without it (5.65±2.01 vs. 6.13±1.75 respectively, p=0.033) (Table 3). The baseline renal function, blood pressure, and the proportion of patients taking inhibitors of RAS or steroid were not different between patients with the T allele and those without it. The progression of renal disease was observed in 11.4% (43/334) of patients without the T allele and in 3.9% (4/103) of those with it (p=0.024) (Table 4). According to sex, there was no significant difference in the incidence of progressive renal disease between patients with the T allele and those without it. However, it tended to increase in the patients without the T allele (Table 4).
With a univariate Cox proportional hazard model, the presence of T allele at AT2R A1818T, female gender, lower serum creatinine level at the time of kidney biopsy, absence of hypertension, and suPCR <3 were associated with better renal prognosis. With multivariate analysis, the presence of T allele and lower baseline serum creatinine level were independent factors associated with better prognosis (Table 5). The Kaplan-Meier survival curve in Fig. 1 shows that the survival rate of the patients with the patients with the T allele is significantly better than those without it. (Logrank test, p=0.0236).
Our study indicated that the A1818T polymorphism of AT2R gene is an independent prognostic factor for IgAN but not a significant susceptibility factor for IgAN development. To the best of our knowledge, this is the first report on the association between the A1818T polymorphism and the prognosis of primary renal disease. Various genetic factors have been reported to be associated with the susceptibility or prognosis of IgAN (17). Regarding chronic renal diseases, including IgAN and diabetic nephropathy, the genetic polymorphisms of genes involved in the renin-angiotensin system have been investigated most extensively because of their essential roles in the pathophysiology of chronic renal diseases and the renoprotective effects of RAS inhibitors on various chronic renal diseases, independent of blood pressure lowering effect. The counter-regulatory role of the AT2R in the biologic effects mediated by the ATR1 has raised a possible renoprotective role of AT2R and a novel therapeutic target for IgAN.
The variants of AT2R have been reported to be associated with various cardiovascular and renal diseases. AT2R gene null mice showed congenital anomalies of the kidney and urinary tract (18) and the AT2R gene transfer to the heart attenuated cardiac hypertrophy and fibrosis in a nongenetic rat model of hypertension (19). It has been reported that A to G transition in intron 1 of the AT2R gene was associated with congenital anomalies of kidney and urinary tract in Caucacians (18), but not in Japanese (16). The association of the AT2R gene variants with body mass index (20), the protective role of the AT2R gene in hypertensive subjects (21), and the association of AT2R gene polymorphism with the development of hypertension (22) and salt sensitivity (23) have been reported. It has been suggested that the +1675 G/A polymorphism of the AT2R gene is associated with early structural changes of the heart due to arterial hypertension (24). The variants of AT2R gene have been reported to be associated with a lower GFR and a higher pulse pressure in type 1 diabetes patients (14). Based on the results of this report, it is thought that the AT2R gene might be associated with clinical features of primary renal diseases.
Our study indicated that the T allele of the A1818T polymorphism of the AT2R gene was associated with better prognosis of IgAN in a relatively large number of patients. However, further functional studies on the biologic implications of polymorphism relevant to the pathophysiology of IgAN are needed to confirm our results. In addition, further genetic research with a large sample sized and a longer follow-up period is required to determine the interaction between conventional risk factors and various genetic risk factors.
In conclusion, the results of this study suggest that the A1818T polymorphism of the AT2R gene may be associated with the prognosis of IgAN, but not with susceptibility to IgAN and also, these results need to be confirmed in different ethnic groups.
Members of the PREMIER group: Institutions that participated in the study (Investigators).
Cheju National University Hospital (Eun Hee Jang), Chonbuk National University Medical School (Won Kim), Chonnam National University Medical School (Nam Ho Kim, Woo Kyun Bae), Chungbuk National University College of Medicine (Hye Young Kim), Chungnam National University College of Medicine (Young-Tai Shin, Kang Wook Lee, Ki-Ryang Na), Daegu Catholic University Medical Center (Ki Sung Ahn), Dankook University Hospital (Jong Tae Cho, Eun Kyeong Lee), Dong-A University College of Medicine (Ki Hyun Kim, Wonsuk An, Seong Eun Kim), Ewha Womans University School of Medicine (Choi Gyu Bog, Seung-Jung Kim), Gachon University of Medicine and Science (Woo Kyung Chung, Hyun Hee Lee, Jaeseok Yang, Sejoong Kim), Gyeongsang National University Hospital (Se-Ho Chang), Hallym University College of Medicine (Jung Woo Noh, Young Ki Lee, Seong Gyun Kim, Jieun Oh, Young Rim Song), Inha University College of Medicine (Moon Jae Kim, Seoung Woo Lee), Inje University College of Medicine (Yeong Hoon Kim, Won Do Park), Keimyung university school of medicine (Hyun Chul Kim, Sung Bae Park), Konkuk University School of Medicine (Kyo-Soon Kim), Korea University Anam Hospital (Won Yong Cho, Hyung Kyu Kim, Sang Kyung Jo), Korea University Ansan Hospital (Cha Dae Ryong, Kang Young Sun), Korea University College of Medicine Guro Hospital (Young-Joo Kwon), Kyungpook National University School of Medicine (Yong-Lim Kim, Sun-Hee Park, Chan-Duck Kim), Pochon CHA University College of Medicine (Dong Ho Yang), Pusan National University School of Medicine (Ihm Soo Kwak,, Soo Bong Lee, Dong Won Lee, Sang Heon Song, Eun Young Seoung), Seoul Medical Center (Su-Jin Yoon), Seoul National University Bundang Hospital (Dong-Wan Chae, Ki Young Na, Ho Jun Chin), Seoul National University College of Medicine Boramae Medical Center (Chun Soo Lim, Yoon Kyu Oh), Seoul National University Hospital (Kook Hwan Oh, Kwon Wook Joo, Yon-Su Kim, Curie Ahn, Jin Suk Han, Suhnggwon Kim), Seoul National University Hosptial Clinical Institute (Hyung Jin Yoon), Sungkyunkwan University School of Medicine (Kyu-Beck Lee), Sungkyunkwan University School of Medicine Samsung Medical Center (Yoon Goo Kim, Jung Eun Lee), Ulsan University College of Medicine, Asan Medical Center (Sang Koo Lee), Yeungnam University College of Medicine (Jun-Young Do, Jong-Won Park, Kyung-Woo Yoon), ordered by alphabet.
Figures and Tables
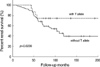 | Fig. 1Kaplan-Meier curve of survivorship of immunoglobulin A nephropathy according to allelic difference. |
References
1. Yagame M, Suzuki D, Jinde K, Saotome N, Murakami R, Asakura K, Nakashima R, Kashem A, Yano N, Endoh M, Nomoto Y, Sakai H, Tomino Y. Value of pathological grading in prediction of renal survival in IgA nephropathy. Nephrology. 1996. 2:107–117.

2. Koyama A, Igarashi M, Kobayashi M. Natural history and risk factors for immunoglobulin A nephropathy in Japan. Am J Kidney Dis. 1997. 29:526–532.

3. Li PK, Ho KK, Szeto CC, Yu L, Lai FM. Prognostic indicators of IgA nephropathy in the Chinese-clinical and pathological perspectives. Nephrol Dial Transplant. 2002. 17:64–69.

4. Frimat L, Briançon S, Hestin D, Aymard B, Renoult E, Huu TC, Kessler M. IgA nephropathy: prognostic classification of end-stage renal failure. Nephrol Dial Transplant. 1997. 12:2569–2575.
5. Rychlik I, Andrassy K, Waldherr R, Zuna I, Tesar V, Jancová E, Ste jskalová A, Ritz E. Clinical features and natural history of IgA nephropathy. Ann Med Interne. 1999. 150:117–126.
6. Vleming LJ, de Fijter JW, Westendorp RG, Daha MR, Bruijn JA, van Es LA. Histomorphometric correlates of renal failure in IgA nephropathy. Clinical Nephrol. 1998. 49:337–344.
7. D'Amico G, Colasanti G, Barbiano di Belgioioso G, Fellin G, Ragni A, Egidi F, Radaelli L, Fogazzi G, Ponticelli C, Minetti L. Long-term follow-up of IgA mesangial nephropathy: clinico-histological study in 374 patients. Semin Nephrol. 1987. 4:355–358.
8. Hsu SI, Ramirez SB, Winn MP, Bonventre JV, Owen WF. Evidence for genetic factors in the development and progression of IgA nephropathy. Kidney Int. 2000. 57:1818–1835.

9. Frimat L, Kessler M. Controversies concerning the importance of genetic polymorphism in IgA nephropathy. Nephrol Dial Transplant. 2002. 17:542–545.

10. Suzuki S, Suzuki Y, Kobayashi Y, Harada T, Kawamura T, Yoshida H, Tomino Y. Insertion/deletion polymorphism in ACE gene is not associated with renal progression in Japanese patients with IgA nephropathy. Am J Kidney Dis. 2000. 35:896–903.

11. Goto S, Narita I, Saito N, Watanabe Y, Yamazaki H, Sakatsume M, Shimada H, Nishi S, Ueno M, Akazawa K, Arakawa M, Gejyo F. A(-20)C polymorphism of the angiotensinogen gene and progression of IgA nephropathy. Kidney Int. 2002. 62:980–985.

12. Carey RM. Update on the role of the AT2 receptor. Curr Opin Nephrol Hypertens. 2005. 14:67–71.
13. Chan LY, Leung JC, Tang SC, Choy CB, Lai KN. Tubular Expression of Angiotensin II Receptors and Their Regulation in IgA Nephropathy. J Am Soc Nephrol. 2005. 16:2306–2317.

14. Pettersson-Fernholm K, Fröjdö S, Fagerudd J, Thomas MC, Forsblom C, Wessman M, Groop PH. FinnDiane Study Group. The AT2 gene may have a gender-specific effect on kidney function and pulse pressure in type 1 diabetic patients. Kidney Int. 2006. 69:1880–1884.
15. Levey AS, Greene T, Kusek JW, Beck GJ, Group MS. A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract]. J Am Soc Nephrol. 2000. 11:A0828.
16. Hiraoka M, Taniguchi T, Nakai H, Kino M, Okada Y, Tanizawa A, Tsukahara H, Ohshima Y, Muramatsu I, Mayumi M. No evidence for AT2R gene derangement in human urinary tract abnormalies. Kidney Int. 2001. 59:1244–1249.
17. Barratt J, Feehally J, Smith AC. Pathogenesis of IgA nephropathy. Semin Nephrol. 2004. 24:197–217.

18. Nishimura H, Yerkes E, Hohenfellner K, Miyazaki Y, Ma J, Hunley TE, Yoshida H, Ichiki T, Threadgill D, Phillips JA 3rd, Hogan BM, Fogo A, Brock JW 3rd, Inagami T, Ichikawa I. Role of the angiotensin type 2 receptor gene in congenital anomalies of the kidney and urinary tract, CAKUT, of mice and men. Mol Cell. 1999. 3:1–10.

19. Falcón BL, Stewart JM, Bourassa E, Katovich MJ, Walter G, Speth RC, Sumners C, Raizada MK. Angiotensin II type 2 receptor gene transfer elicits cardioprotective effects in an angiotensin II infusion rat model of hypertension. Physiol Genomics. 2004. 19:255–261.

20. Kotani K, Sakane N, Saiga K, Tsuzaki K, Sano Y, Mu H, Kurozawa Y. The angiotensin II type 2 receptor gene polymorphism and body mass index in healthy Japanese women. Ann Clin Biochem. 2007. 44:83–85.

21. Jones A, Dhamrait SS, Payne JR, Hawe E, Li P, Toor IS, Luong L, Wootton PT, Miller GJ, Humphries SE, Montgomery HE. Genetic variants of angiotensin II receptors and cardiovascular risk in hypertension. Hypertension. 2003. 42:500–506.

22. Jin JJ, Nakura J, Wu Z, Yamamoto M, Abe M, Chen Y, Tabara Y, Yamamoto Y, Igase M, Bo X, Kohara K, Miki T. Association of angiotensin II type 2 receptor gene variant with hypertension. Hypertens Res. 2003. 26:547–552.





 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download