Abstract
Restorative proctocolectomy with ileal pouch-anal anastomosis is one of the surgical treatments of choice for patients with familial adenomatous polyposis. Although the risk of cancer developing in an ileal pouch is not yet clear, a few cases of adenocarcinoma arising in an ileal pouch have been reported. We report a case of adenocarcinoma in ileal pouch after proctocolectomy with ileal pouch-anal anastomosis. A 56-yr-old woman was diagnosed as having familial adenomatous polyposis. Total colectomy with ileorectal anastomosis was performed. Six years later, she underwent completion-proctectomy with ileal J pouch-anal anastomosis including anorectal mucosectomy for rectal cancer. After 7 yr, she presented with anal spotting. Endoscopic biopsies revealed adenocarcinoma at the ileal pouch. Resection of the ileal pouch and permanent ileostomy were performed. The risk of cancer in an ileal pouch and its prevention with regular surveillance must be emphasized.
Primary adenocarcinoma at the site of an ileal pouch-anal anastomosis (IPAA) is rare. In familial adenomatous polyposis (FAP), the subsequent development of adenocarcinoma in ileal pouch, residual rectal mucosa in the anal canal or anastomotic site have been reported (1-11).
After restorative proctocolectomy, some rectal mucosa may be left behind, even after ano-rectal mucosectomy has been performed (12). Theoretically, this residual mucosa may develop dysplasia or cancer in the anastomotic site of IPAA or the anal transitional zone. Also, the inflammatory mucosal changes or adenomas in ileal pouch have been thought to be risk factors for cancer development (7, 13). But there is no definitive correlation between cancer development and the presence of inflammatory mucosal changes or adenomas in ileal pouch. The reported cases of cancer in ileal pouch were very few. Herein we report a case of adenocarcinoma arising from the ileal pouch after an IPAA and represents the first reported case of ileal pouch cancer in a patient with FAP in Korea.
A 56-yr-old woman was diagnosed with FAP in 1992. Total colectomy with ileorectal anastomosis was carried out in another Hospital. In January 1998, rectal cancer was identified 15 cm above the anal verge. Proctectomy, formation of an ileal J-pouch, IPAA and protective ileostomy were performed. Take down of ileostomy was done 3 months later. Histopathology showed a moderately differentiated rectal adenocarcinoma that has infiltrated into the muscularis propria (pT2). Lymph node metastasis was not found (pN0). After surgery, adjuvant chemotherapy with 5-fluorouracil was underwent for a year. Chest radiography, abdominal computed tomography, and sigmoidoscopy were performed annually. She had no recurrence signs on follow-up studies during the follow-up of three years. Afterward, follow-up was lost for four years.
In March 2005, 7 yr later, she presented with anal spotting. Endoscopy revealed an ulcero-fungating tumor in the ileal pouch, 5 cm above the anal verge. Forcep biopsies were interpreted as adenocarcinoma. Computed tomography showed tumorous wall thickening of the ileal pouch with peri-pouch tissue invasion (Fig. 1). Extirpation of the ileal J-pouch above the previous anastomotic site and permanent ileostomy were performed.
Gross examination of the pouch specimen revealed a 3×2.5 cm sized ulcerative mucosal lesion with adenocarcinoma (Fig. 2). The tumor was exposed on the ileal serosa. Histologic examination revealed a well-differentiated adenocarcinoma composed of anaplastic glandular epithelial cells in the mucosa and submucosa (Fig. 3A). The tumor cells had infiltrated into the ileal serosa. Both proximal and distal margins of the resected pouch were free of tumor cells. Eight lymph nodes with metastses were found among 12 lymph nodes examined. (Fig. 3B). The patient received chemotherapy with oxaliplatin, 5-fluorouracil and leucovorin. In July 2007, lung metastasis was identified.
Restorative proctocolectomy with IPAA has now been accepted as the standard surgical procedure for FAP. When an IPAA is performed, controversy exists about the appropriate technique to be used for the pouch-anal anastomosis. Techniques vary between a handsewn IPAA with mucosectomy of the anal transitional zone or a stapled IPAA at the level of the ano-rectal ring without mucosectomy. A stapled IPAA has simplified the operation and improved the functional results, but this retains the rectal mucosa on the anal transitional zone (12). Although a mucosectomy and hand sewn anastomosis are necessary for complete removal of the rectal mucosa, some rectal mucosa may be left behind, even after an ano-rectal mucosectomy has been performed (14). This residual mucosa in the anal transitional zone may develop dysplasia or cancer, but the risk of dysplasia in the anal transitional zone is very low and is usually self-limiting (15, 16). Remzi et al. (16) suggested that the anal transitional zone preservation did not lead to the development of cancer in this area after a minimum of ten years of follow up. However, Ooi et al. (8) reported two cases of anal transitional zone cancer after restorative proctocolectomy and ileo-anal anastomosis in FAP patients. The interval between ileo-anal anastomosis and cancer development was 3 and 8 yr.
Concern about the risk of neoplasia in ileal pouches was raised after observing a combination of histologic changes in the ileal mucosa of the pouch (17-19). These histologic changes include villous atrophy, inflammation and metaplasia. These transformations in ileal pouches are caused by a chronic inflammatory state. Theoretically, the inflammatory response as seen in pouchitis may lead to dysplasia. Further inflammation can then lead to loss of heterozygosity in similar regions consistent with precancerous lesions of the colon (13). Based on this reasoning, the proposed dysplasia to neoplasia pathway can occur in ileal pouches and can lead to cancer of the pouch. The cumulative risk of pouchitis is up to 50% in patients with ulcerative colitis and they experience at least one episode of pouchitis during the first ten years after surgical pouch construction, while pouches in patients with FAP have pouchitis rate below 5% (20-22). Also, the incidence of dysplasia in the ileal pouches is very low (23, 24). There are no reports of carcinoma developing on a background of pouchitis with bacterial proliferation but it is a theoretical possibility.
Ileal adenomatous transformation is one of the most logical explanation for cancer arising in ileal pouches (7). Parc et al. (25) reported that the risk of developing one or more pouch adenomas in FAP patients at 5, 10, and 15 yr was 7%, 35%, and 75%, respectively. Most studies of pouch adenomas have described only small polyps with low risk of malignant change (26). It is necessary to have a long-term endoscopic surveillance of the pouches in FAP patients for pouch adenomas. The relationship between the presence of pouch adenomas and increasing age, the presence of duodenal or ampullary adenomas, the follow-up period and the site of APC mutation are unclear (25, 26).
It is not clear what malignant potential pouchitis or pouch adenoma may have and what the lifetime risk of developing pouch cancer will be for patients with FAP. We experienced a case with adenocarcinoma in ileal pouch among total 16 cases of FAP patients. There are several reported cases with adenocarcinoma in ileal pouches, anastomotic sites, anal transitional zone and rectal cuffs after restorative proctocolectomy and ileo-anal anastomosis in FAP patients (Table 1). The mean interval between IPAA and emergence of adenocarcinoma in ileal pouches or remained the anal canal was 7.63 yr (range, 3-20 yr) (1-11). Therefore, a relatively long period of careful and periodic pouch surveillance should be routinely done in FAP patients with IPAA.
Figures and Tables
 | Fig. 1Computed tomography displayed a tumor (arrow) at ileal pouch extending into the peri-pouch tissue. |
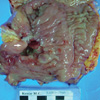 | Fig. 2Gross finding showed a large ulcerative lesion at the posterior wall of the ileal pouch, measuring 3×2.5 cm, located 12 cm from the proximal margin and 2.5 cm from the distal margin. The distal margin was previous anastomotic site. |
References
1. Hoehner JC, Metcalf AM. Development of invasive adenocarcinoma following colectomy with ileoanal anastomosis for familial polyposis coli. Report of a case. Dis Colon Rectum. 1994. 37:824–828.
2. von Herbay A, Stern J, Herfarth C. Pouch-anal cancer after restorative proctocolectomy for familial adenomatous polyposis. Am J Surg Pathol. 1996. 20:995–999.

3. Bassuini MM, Billings PJ. Carcinoma in an ileoanal pouch after restorative proctocolectomy for familial adenomatous polyposis. Br J Surg. 1996. 83:506.

4. Palkar VM, deSouza LJ, Jagannath P, Naresh KN. Adenocarcinoma arising in "J" pouch after total proctocolectomy for familial polyposis coli. Indian J Cancer. 1997. 34:16–19.
5. Vuilleumier H, Halkic N, Ksontini R, Gillet M. Columnar cuff cancer after restorative proctocolectomy for familial adenomatous polyposis. Gut. 2000. 47:732–734.

6. Brown SR, Donati D, Seow-Choen F. Rectal cancer after mucosectomy for ileoanal pouch in familial adenomatous polyposis: report of a case. Dis Colon Rectum. 2001. 44:1714–1715.
7. Cherki S, Glehen O, Moutardier V, Francois Y, Gilly FN, Vignal J. Pouch adenocarcinoma after restorative proctocolectomy for familial adenomatous polyposis. Colorectal Dis. 2003. 5:592–594.

8. Ooi BS, Remzi FH, Gramlich T, Church JM, Preen M, Fazio VW. Anal transitional zone cancer after restorative proctocolectomy and ileoanal anastomosis in familial adenomatous polyposis: report of two cases. Dis Colon Rectum. 2003. 46:1418–1423.
9. Vrouenraets BC, Van Duijvendijk P, Bemelman WA, Offerhaus GJ, Slors JF. Adenocarcinoma in the anal canal after ileal pouch-anal anastomosis for familial adenomatous polyposis using a double-stapled technique: report of two cases. Dis Colon Rectum. 2004. 47:530–534.

10. Campos FG, Habr-Gama A, Kiss DR, da Silva EV, Rawet V, Imperiale AR, Perez R, da Silva JH, Sousa AH, Gama-Rodrigues J. Adenocarcinoma after ileoanal anastomosis for familial adenomatous polyposis: review of risk factors and current surveillance apropos of a case. J Gastrointest Surg. 2005. 9:695–702.

11. Ulas M, Nessar G, Bostanoglu A, Aydog G, Kayaalp C, Ozogul Y, Seven C. Development of two cancers in the same patient after ileorectal and ileal pouch anal anastomosis for familial adenomatous polyposis. Med Princ Pract. 2006. 15:83–86.

12. Tuckson W, Lavery I, Fazio V, Oakley J, Church J, Milsom J. Manometric and functional comparison of ileal pouch anal anastomosis with and without anal manipulation. Am J Surg. 1991. 161:90–96.

13. Gullberg K, Lindforss U, Zetterquist H, Stalberg D, Reinholt FP, Veress B, Tribukait B, Olivecrona H, Lofberg R. Cancer risk assessment in long-standing pouchitis; DNA aberrations are rare in transformed neoplastic pelvic pouch mucosa. Int J Colorectal Dis. 2002. 17:92–97.
14. Heppell J, Weiland LH, Perrault J, Pemberton JH, Telander RL, Beart RW Jr. Fate of rectal mucosa after rectal mucosectomy and ileoanal anastomosis. Dis Colon Rectum. 1983. 26:768–771.
15. Ziv Y, Fazio VW, Sirimarco MT, Lavery IC, Goldblum JR, Petras RE. Incidence, risk factors, and treatment of dysplasia in the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum. 1994. 37:1281–1285.

16. Remzi FH, Fazio VW, Delaney CP, Preen M, Ormsby A, Bast J, O'Riordain MG, Strong SA, Church JM, Petras RE, Gramlich T, Lavery IC. Dysplasia of the anal transitional zone after ileal pouchanal anastomosis: results of prospective evaluation after a minimum of ten years. Dis Colon Rectum. 2003. 46:6–13.
17. Gullberg K, Stahlberg D, Liljeqvist L, Tribukait B, Reinholt FP, Veress B, Lofberg R. Neoplastic transformation of the pelvic pouch mucosa in patients with ulcerative colitis. Gastroenterology. 1997. 112:1487–1492.

18. Veress B, Reinholt FP, Lindquist K, Lofberg R, Liljeqvist L. Long-term histomorphological surveillance of the pelvic ileal pouch: dysplasia develops in a subgroup of patients. Gastroenterology. 1995. 109:1090–1097.

19. Setti Carraro P, Talbot IC, Nicholls RJ. Longterm appraisal of the histological appearances of the ileal reservoir mucosa after restorative proctocolectomy for ulcerative colitis. Gut. 1994. 35:1721–1727.

20. Heuschen UA, Autschbach F, Allemeyer EH, Zollinger AM, Heuschen G, Uehlein T, Herfarth C, Stern J. Long-term follow-up after ileoanal pouch procedure: algorithm for diagnosis, classification, and management of pouchitis. Dis Colon Rectum. 2001. 44:487–499.
21. Kuhbacher T, Schreiber S, Runkel N. Pouchitis: pathophysiology and treatment. Int J Colorectal Dis. 1998. 13:196–207.
22. Dozois RR, Kelly KA, Welling DR, Gordon H, Beart RW Jr, Wolff BG, Pemberton JH, Ilstrup DM. Ileal pouch-anal anastomosis: comparison of results in familial adenomatous polyposis and chronic ulcerative colitis. Ann Surg. 1989. 210:268–273.
23. Herline AJ, Meisinger LL, Rusin LC, Roberts PL, Murray JJ, Coller JA, Marcello PW, Schoetz DJ. Is routine pouch surveillance for dysplasia indicated for ileoanal pouches? Dis Colon Rectum. 2003. 46:156–159.

24. Thompson-Fawcett MW, Marcus V, Redston M, Cohen Z, McLeod RS. Risk of dysplasia in long-term ileal pouches and pouches with chronic pouchitis. Gastroenterology. 2001. 121:275–281.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download