Abstract
Biofeedback with or without combined autogenic training is known to be effective for the treatment of migraine. This study aimed to examine the effect of biofeedback treatment on headache activity, anxiety, and depression in Korean female patients with migraine headache. Patients were randomized into the treatment group (n=17) and monitoring group (n=15). Mood states including anxiety and depression, and psychophysiological variables such as mean skin temperature of the patients were compared with those of the normal controls (n=21). We found greater treatment response rate (defined as ≥50% reduction in headache index) in patients with biofeedback-assisted autogenic training than in monitoring group. The scores on the anxiety and depression scales in the patients receiving biofeedback-assisted autogenic training decreased after the biofeedback treatment. Moreover, the decrease in their anxiety levels was significantly related to the treatment outcome. This result suggests that the biofeedback-assisted autogenic training is effective for the treatment of migraine and its therapeutic effect is closely related to the improvement of the anxiety level.
Migraine is a highly prevalent illness, and women of reproductive ages are more affected by it than men or women in other age groups (1). Many researchers have supported the view that behavioral interventions such as biofeedback and relaxation, either alone or in combination, can be effective for the treatment of headache (2-7). Especially, thermal biofeedback with or without combined autogenic training is known to be effective for the treatment of migraine headache (5, 8). In addition, some studies showed that the effect of the behavioral treatment is durable (9, 10). There have been no controlled studies about the efficacy of biofeedback and relaxation training for patients with migraine in Korea, and few studies have been conducted to investigate the direct association between mood states, including anxiety or depression, and headache activity. The mechanism underlying the efficacy of biofeedback treatment and the role of psychological factors in migraine treatment are still unclear, though various mood states, including anxiety and depression, and some cognitive factors are known to be related to pain regulation (11-13). Psychological conditions including anxiety and depression have been reported to have a strong association with migraine (12-14).
Thus, in this study, we examined the hypothesis that biofeedback-assisted autogenic training is effective for the treatment of Korean female patients with migraine and that the improvement of psychological factors, such as anxiety and depression, is associated with the reduction of headache activity in migraine patients who are given biofeedback treatment.
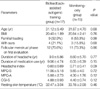
Thirty-two patients, who had migraine headache with or without aura, as defined by the International Headache Society criteria (15), participated in this study, from March 2003 until December 2006. The patients were female subjects aged 20 to 40 yr who had a body mass index (BMI) ranging from 18 to 27.5. They were among the migraineurs who visited the Samsung Medical Center. The patients were randomly allocated to one of two patient groups, consisting of a treatment group receiving biofeedback-assistant relaxation treatment (n=17) and a monitoring group in which the headache activities and biofeedback parameters of the patients were simply measured (n=15). These two groups did not show any significant difference in the duration of headache, headache index, duration of medication use, or other headache-related variables at the baseline (Table 1). Twenty-one normal female volunteers were recruited by advertisement and were matched with the migraine patients by age (treatment group: 31.12±5.49 yr, monitoring group: 31.87±4.70 yr, normal control group: 29.38±4.64 yr), and mood states and mean skin temperature of the patients before the biofeedback treatment were compared with those of the normal control subjects. Each subject underwent a comprehensive medical and psychiatric assessment including careful history taking, physical examination, neurological examination, mental status examination, and electrocardiography. Those patients who seemed to suffer from secondary headache due to medical or psychiatric illnesses were not included in the study. They did not take regular medications for migraine headache, and only pro re nata (p.r.n.) medication such as sumatriptan was permitted during the study. This study was approved by the Institutional Review Board of Samsung Medical Center, and all of the subjects gave their written informed consent.
The patients in the treatment group received 8 sessions of biofeedback-assisted autogenic training (two sessions per week) during a period of 4 weeks, while those in the monitoring group received no active intervention except for simple biofeedback measurements (1st, 4th, and 8th session) during the treatment-waiting period. Biofeedback treatment was administered with the patient sitting on a comfortable arm-chair in a quiet room in the psychiatric outpatient clinic of Samsung Medical Center. A Procomp+system and Biograph version 2.1 program (Thought Technology Ltd., Quebec, Canada) were used for the biofeedback treatment and measurements.
Each biofeedback-assisted autogenic training session lasted about 45-50 min. The autogenic training procedures consisted of 6 standard exercises combining both relaxation and auto-suggestion (limb heaviness exercise, limb warmth exercise, cardiac exercise, respiration exercise, solar plexus warmth exercise, and "forehead cooling" exercise) (16). During the 1st session, after the baseline profiles were obtained, education in relaxation techniques was given to the patients in the treatment group. During the 2nd to 8th sessions, thermal biofeedback combined with autogenic training was provided. For the first 15-20 min, after collecting the headache diary data, the patients were rated on psychological variables and headache severity. The patients were trained to increase their skin temperature by an experienced biofeedback therapist for about 15 min according to the procedures described in a treatment manual. During the last 15 min, they were instructed to continue the relaxation exercise by themselves, while listening to a prerecorded tape. They were also asked to perform autogenic training as homework between the sessions.
Headache indices were obtained using a daily headache diary over 7 consecutive days. Success was defined as a 50% reduction in the score. The headache severity was rated on a 6-point rating scale with 0 representing "no pain" and 5 representing "pain as severe as it can be". The headache severity was recorded every hour except during sleep. The average frequency, duration, and intensity of pain during the 7 consecutive days were compiled as headache indexes. Headache indexes at baseline, after 2 weeks, and after 4 weeks of biofeedback treatment were used to compare the two groups.
Secondary outcomes were evaluated using the MPQ (17) and the Clinical Global Impression severity scale (CGI-S) administered by the therapist. The baseline headache variables were recorded for the previous 1 week before the treatment and the follow-up headache variables as the mean of the symptoms during the previous week. Due to the possibility of there being a change in the perception of pain according to the menstrual cycle (18), the menstruation phase was determined by asking the subjects the onset of their last menstruation. Before the biofeedback treatment, there were no differences in the headache indices and mood states between the treatment group and monitoring group according to the menstruation phase.
The psychological assessments for anxiety and depressive symptoms were performed using the Hamilton Rating Scales for Anxiety (HAM-A) (19) and Depression (HAM-D) (20), and the Spielberger State Anxiety Inventory (STAI-S) (21). The CGI-S, HAM-A, and HAM-D were performed by a well-trained psychiatrist who was blind to the patients' clinical states.
To compare the baseline values, chi-square test, Fisher's exact test, and analysis of variance (ANOVA) were used. Treatment outcome analysis in terms of headache index was preformed using chi-square test. Repeated measures ANOVA was performed to analysis mean changes of skin temperature, psychological variables, and secondary pain outcomes. Student's t-test with Bonferroni's correction was performed for post hoc analysis. Univariate and multivariate logistic regression analyses were used to whether the baseline or changes of depression and anxiety level could predict the treatment outcome. All of the analyses were performed using the SPSS 13.0 statistical software.
The Fisher's exact test revealed a significant difference in the response rate in terms of headache index between the two groups (χ2=4.979, df=1, P=0.029). Ten of the 17 patients (58.9%) in the treatment group showed a significant improvement in their headache index corresponding to a 50% or greater reduction in their headache activity, whereas only 3 of the 15 subjects (20%) in the monitoring group achieved a significant improvement (Fig. 1). Repeated measures ANOVA indicated that there were significant interactions between time and group in the MPQ-S (F=6.994, P=0.014), MPQ-A (F=9.978, P=0.006), and CGI-S (F=16.160, P=0.001). Mean resting skin temperatures did not show any differences between the treatment and monitoring group, nor pre- and post-treatment (all P values >0.1).
The results of the comparisons of the psychological states of the three groups are shown in Table 2. The anxiety and depression levels in the migraine patients were significantly higher than those in the normal control subjects at the baseline (all P values <0.001). There were no group differences between the biofeedback-assisted autogenic training group and the monitoring group.
Fig. 2 shows the results of the repeated-measures ANOVA in the psychological variables. Significant interactions between time and group were found for the HAM-A (F=10.560, P=0.003), HAM-D (F=8.161, P=0.013), and STAI-S (F=12.320, P=0.002). Post hoc analysis revealed that there were significant between-group differences at the endpoint (P=0.002, 0.032, 0.001, respectively).
Age, BMI, the baseline HAM-D, HAM-A, and STAI-S were not associated with treatment response in terms of headache index (all P values >0.1) in the biofeedback-assisted training group. However, the multivariate logistic regression revealed that the greater reduction of the HAM-A score was associated with the treatment response controlling for age, BMI, and the baseline HAM-A in the biofeedback-assisted autogenic training group (OR=1.52, CI=1.01-2.33, P=0.048) whereas the reduction of the HAM-D score nor that of the STAI-S were not (P=0.088 and P=0.080, respectively).
We found that biofeedback-assisted autogenic training is effective in management of female migraine patients in Korean population. They also exhibited significant differences in their mood states measured by the HAM-A, HAM-D, STAI-S, as compared with the normal healthy women. This finding is consistent with the results of previous studies which showed that migraine patients had high levels of anxiety and depression (12, 14, 22). It is also consistent with a previous report (23) that negative mood states such as anxiety and depression are related to physical complaints and headache. The anxiety and depression scores in the migraine patients were reduced after 4 weeks of biofeedback treatment. Furthermore, the reduction in anxiety level after the biofeedback treatment was related to the treatment response of the patients. To our knowledge, there have been no reports about the association between mood states, including anxiety and depression, and improvements in headache activity in migraine patients receiving biofeedback treatment. Our result is also consistent with the finding of previous studies (24-27) that mood states might affect the experience of pain through the cognitive processing of nociceptive information, although this hypothesis has not been directly examined in headache patients. The present result is in contrast with the previous report (2) that decreased depression level rather than anxiety was related to the outcome of biofeedback-assisted training in patients with chronic tension-type headache. Taken together, reduction of anxiety may be related to the biofeedback treatment response of migraine headache, whereas reduction of depression may be related to the biofeedback treatment response of chronic tension-type headache. Further studies will be necessary to confirm this difference between migraine and tension type headache.
Mean skin temperatures between the pre- and post-treatment changes were not statistically different. Our finding also suggests that the reduction of anxiety rather than depression level is more important in the biofeedback treatment of migraine. This result appears to confirm the previous findings that the treatment mechanism of biofeedback is mediated by an indirect process rather than a direct physiological change (28, 29). Cognitive factors such as increased self-efficacy belief or coping style can affect the success of biofeedback treatment, and anxiety is known to be closely associated with cognitive factors (11). However, since migraine is known to be inter-related to anxiety (30), our tentative finding has the limitation that it does not confirm whether an improvement in anxiety causes a decrease in headache activity. Further studies are needed to examine the relationship among mood states, cognitive factors, and headache.
There are several limitations in this study. Firstly, the time period of the study was short. Migraine is an illness with a fluctuating course in which the symptoms wax and wane, and psychophysiological treatment may have a delayed effect. Secondly, the severity of headache in the recruited patients was relatively low and the patients in this study may not represent the general population with migraine headache. Finally, our sample size was relatively small. However, to the best of our knowledge, this is the first controlled study to examine the efficacy of biofeedback treatment and the relationship between mood states and headache activity in Korean migraine patients.
In conclusion, biofeedback treatment was found to cause an improvement of headache and mood states such as anxiety and depression in female migraine patients. In addition, the reduction of anxiety level was related to the biofeedback treatment response. These results suggest that biofeedback treatment can be an effective non-pharmacological treatment for migraine patients and that the improvement of the anxiety states afforded by biofeedback treatment may play a key role in reducing headache activity.
Figures and Tables
Fig. 1
Greater treatment response rate (defined as ≥50% reduction in headache index) was observed in patients with biofeedback-assisted autogenic training than in monitoring-only group (58.9% vs. 20%, χ2=4.979, d=1, P=0.029).

Fig. 2
Mood states by treatment group (Biofeedback-assisted autogenic training group vs. monitoring-only group). There were significant interactions between the two groups in changes of the HAM-A (F=10.560, P=0.003), HAM-D (F=8.161, P=0.013), and STAI-S (F=12.320, P=0.002). Post hoc analyses revealed that there were significant differences at the endpoint between the two groups in all the mood states (all P values <0.1).

Table 2
Mood states of migraine patients and normal control subjects at baseline

Data are given as mean±S.D.
*Significant by one-way analysis of variance (ANOVA). Post hoc analysis revealed that there were no significant differences in the mood states between the treatment and monitoring groups, whereas there was a significant differences between the patient group and normal controls (P<0.01, by Bonferroni's correction).
HAM-A, the Hamilton Rating Scale for Anxiety; STAI-S, the Spielberger State Anxiety Inventory; HAM-D, the Hamilton Rating Scale for Depression.
References
1. Lipton RB, Bigal ME. Migraine: epidemiology, impact, and risk factors for progression. Headache. 2005. 45:Suppl 1. S3–S13.

2. Kang EH, Ahn JY, Koo MS, Park JE, Yu BH. Biofeedback-assisted autogenic training for chronic tension-type headache in a Korean population. J Korean Neuropsychiatr Assoc. 2008. 47:247–253.
3. Jang MS, Hah YS, Chung CS, Yu BH. The effect of biofeedback-assisted relaxation on the clinical symptoms and stress responses in patients with chronic headache. J Korean Neuropsychiatr Assoc. 2004. 43:697–705.
4. Holroyd KA, Penzien DB. Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain. 1990. 42:1–13.

5. Holroyd KA, Penzien DB. Psychosocial interventions in the management of recurrent headache disorders. 1: overview and effectiveness. Behav Med. 1994. 20:53–63.

6. Reich BA. Non-invasive treatment of vascular and muscle contraction headache: a comparative longitudinal clinical study. Headache. 1989. 29:34–41.

7. Nestoriuc Y, Martin A, Rief W, Andrasik F. Biofeedback treatment for headache disorders: a comprehensive efficacy review. Appl Psychophysiol Biofeedback. 2008. 33:125–140.

8. Stetter F, Kupper S. Autogenic training: a meta-analysis of clinical outcome studies. Appl Psychophysiol Biofeedback. 2002. 27:45–98.
9. Grazzi L, Andrasik F, D'Amico D, Leone M, Moschiano F, Bussone G. Electromyographic biofeedback-assisted relaxation training in juvenile episodic tension-type headache: clinical outcome at three-year follow-up. Cephalalgia. 2001. 21:798–803.
10. Silver BV, Blanchard EB, Williamson DA, Theobald DE, Brown DA. Temperature biofeedback and relaxation training in the treatment of migraine headaches. One-year follow-up. Biofeedback Self Regul. 1979. 4:359–366.
11. Feldman SI, Downey G, Schaffer-Neitz R. Pain, negative mood, and perceived support in chronic pain patients: a daily diary study of people with reflex sympathetic dystrophy syndrome. J Consult Clin Psychol. 1999. 67:776–785.

12. Materazzo F, Cathcart S, Pritchard D. Anger, depression, and coping interactions in headache activity and adjustment: a controlled study. J Psychosom Res. 2000. 49:69–75.

13. Pauli P, Wiedemann G, Nickola M. Pain sensitivity, cerebral laterality, and negative affect. Pain. 1999. 80:359–364.

14. McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. 2004. 111:77–83.

15. Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988. 8:Suppl 7. 1–96.
16. Stoyva JM. Basmajian JV, editor. Autogenic training and biofeedback combined: A reliable method for the induction of general relaxation. Biofeedback: Principle and practice for clinicians. 1989. 3rd ed. Baltimore: Williams & Wilkins;169–185.
18. Riley JL 3rd, Robinson ME, Wise EA, Price DD. A meta-analytic review of pain perception across the menstrual cycle. Pain. 1999. 81:225–235.

21. Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State Trait Anxiety Inventory. 1970. Palo Alto, DA: Consulting Psychologists Press.
22. de Filippis S, Salvatori E, Coloprisco G, Martelletti P. Headache and mood disorders. J Headache Pain. 2005. 6:250–253.

23. Watson D, Pennebaker JW. Health complaints, stress, and distress: exploring the central role of negative affectivity. Psychol Rev. 1989. 96:234–254.

24. Cornwall A, Donderi DC. The effect of experimentally induced anxiety on the experience of pressure pain. Pain. 1988. 35:105–113.

25. Dougher MJ, Goldstein D, Leight KA. Induced anxiety and pain. J Anxiety Disord. 1987. 1:259–264.

26. Rhudy JL, Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. 2000. 84:65–75.

27. Robinson ME, Wise EA, Gagnon C, Fillingim RB, Price DD. Influences of gender role and anxiety on sex differences in temporal summation of pain. J Pain. 2004. 5:77–82.

28. Arena JG, Bruno GM, Hannah SL, Meador KJ. A comparison of frontal electromyographic biofeedback training, trapezius electromyographic biofeedback training, and progressive muscle relaxation therapy in the treatment of tension headache. Headache. 1995. 35:411–419.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download