Abstract
This randomized prospective study investigated the effect of fibrin glue use on drainage duration and overall drain output after lumpectomy and axillary dissection in breast cancer patients. A total of 100 patients undergoing breast lumpectomy and axillary dissection were randomized to a fibrin glue group (N=50; glue sprayed onto the axillary dissection site) or a control group (N=50). Outcome measures were drainage duration, overall drain output, and incidence of seroma. Overall, the fibrin glue and control groups were similar in terms of drainage duration, overall drain output, and incidence of seroma. However, subgroup analysis showed that fibrin glue use resulted in a shorter drainage duration (3.5 vs. 4.7 days; p=0.0006) and overall drain output (196 vs. 278 mL; p=0.0255) in patients undergoing level II or III axillary dissection. Fibrin glue use reduced drainage duration and overall drain output in breast cancer patients undergoing a lumpectomy and level II or III axillary dissection.
Prolonged lymphatic drainage following axillary dissection in breast cancer remains a significant clinical problem Shortening the drainage duration is associated with shorter in-patient times and hence lower health care costs. Methods applied to reduce lymphatic drainage include compression dressings (1), closed suction drains (2), postoperative shoulder immobilization (3) and fibrin glue application to the axillary dissection site (4-6).
The use of fibrin glue may reduce lymphatic drainage by reducing the number of transections of small vessels and lymphatics during axillary lymph node removal (7). However, conflicting clinical trial results exist regarding fibrin glue use in breast cancer surgery. Previous trials involved a wide variety of breast cancer surgery types or degrees of axillary dissection (8).
The present randomized study investigated the effect of fibrin glue use on the duration of drainage and overall drain output after breast lumpectomy and axillary dissection for breast cancer.
A prospective, randomized study was performed between September 2006 and July 2007 at the Department of Surgery, Seoul National University Hospital. The inclusion criteria (9) were 1) newly diagnosed breast cancer, 2) female gender, 3) elective breast lumpectomy and axillary dissection, 4) informed consent, and 5) being outside of any exclusion criteria. The exclusion criteria (9) were: 1) male gender, 2) a body mass index (kg/m2) <18.5 or >30, 3) current steroid use, 4) systemic anticoagulation or significant coagulation disorder, 5) diabetes, 6) heart disease, 7) history of chest radiation, 8) receiving preoperative chemotherapy, 9) planned immediate breast reconstruction, 10) pregnant or lactating, 11) limited to sentinel node biopsy, or 12) no consent. The study was approved by the Institutional Review Board of the Seoul National University Hospital.
Surgery was performed by two surgeons using principally identical methods. All patients underwent a lumpectomy and level I or greater axillary lymph node dissection, and an effort was made to ligate major vessels. For the patients in the fibrin glue group, fibrin glue (Greenplast kit®, Green Cross, Seoul, Korea) was mixed intraoperatively and diluted twice according to standard instructions, and 2 mL was sprayed onto the axillary dissection site using an aerosol spray applicator (Green Jet V2®, Green Cross, Seoul, Korea), after which manual compression was applied for 2 min according to manufacturer's manual. A Jackson-Pratt closed suction 100 mL/3.2 mm drain was placed into the axillary dissection site for all patients. Compression dressings with surgical bras and pads were applied to all patients for the first 5 days after surgery. Arm movement was restricted to below 90 degrees for 5 days (3). Participants were discharged on postoperative day 5±1 regardless of drain removal, and were routinely followed-up on postoperative days 12±1 and 30±2.
The primary outcome measure was the duration of drainage. Drainage was assessed daily from the day of surgery, and drains were removed when the drainage volume fell to <30 mL over a 24-hr period. Secondary outcome measures were overall drain output and the incidence of symptomatic seroma formation. A symptomatic seroma was defined as a palpable fluid collection under the wound with symptoms, and was treated using aspiration or open drain insertion. In addition, all wound-related complications were recorded. The wound was examined daily until discharge and during each clinic visit. Wound infections were defined as erythema and/or purulent discharge from the incision site, and were treated using an oral antibiotic for at least 3 days.
The primary endpoint was the duration of drainage. In a pilot study with 21 patients, the mean drainage duration was 3.0 days for the case group and 3.2 days for the control group, and the standard deviation of the mean difference between the case and control groups was 0.255. The current study had a power of 90 percent to show whether the drainage duration differed between the fibrin glue and non-fibrin glue groups. This approach assumed that the drainage duration for the two groups was equal, and that a difference of 10 percent or less was clinically irrelevant.
This approach required each group to have a sample size of 49 considering a 30% dropout, and α (two-sided) was set at 0.05. The enrollment procedure engaged 50 patients per group.
Patients were randomized using a web-based program hosted at the Medical Research Collaborating Center at Seoul National University Hospital. Participant randomization was done after bleeding control and confirmation of a negative margin status, immediately before wound closure. Fig. 1 shows the Consolidated Standards of Reporting Trials (CONSORT) flow chart outlining the progress of participants through the study (10). One hundred participants were randomized, 50 to the fibrin glue group and 50 to the control group (non-fibrin glue). Three fibrin glue patients and two control patients were excluded after randomization due to postoperative bleeding.
The surgical team was 'blinded' to treatment assignment until the completion of the surgical dissection and bleeding control just prior to randomization. The personnel involved in recording drainage volumes and complications were also blinded to the treatment assignment.
Data were stored using the Excel (Microsoft Corporation, Redmond, WA, U.S.A.) spread sheet program, and statistical analyses were performed using SPSS software version 12.0 (SPSS, Chicago, IL, U.S.A.) and SAS (SAS Inc., Cray, NC, U.S.A.). Outcome criteria were analyzed on an intension-to-treat basis and all tests were two-tailed. Qualitative data were compared using the Pearson's chi-square-test for more than 30 samples and Fisher's exact test for less than 30 samples. Quantitative data were expressed as means (standard deviations), and were compared using Student t-tests for all group samples and using Mann-Whitney U tests for subgroup samples. Using the general linear model (GLM) procedure, two-way analysis of variance (ANOVA) was used to identify subgroups showing the greatest benefit from use of fibrin glue. A p value <0.05 was considered to indicate a significant difference.
Of the 100 patients enrolled (50 fibrin glue, 50 control), 95 completed the study to the endpoint. All five of those that did not complete the study developed postoperative bleeding on the day of surgery, and four of them were conservatively treated (compression dressing with elastic bandage and open drain insertion) and the other underwent re-exploration for bleeding control and hematoma evacuation. It was not possible to measure the drainage duration or overall drain output in those five patients because the Jackson-Pratt closed suction drain was removed and an open drain inserted.
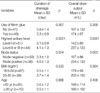
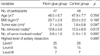
There were no significant differences between the fibrin glue and control groups with respect to age, body mass index (BMI), tumor size, the number of lymph nodes removed, and the number of tumor-involved lymph nodes (Table 1). Level I axillary dissection and node-negative status were found to be associated with a shorter drainage duration (p=0.0001 and p=0.004, respectively) and lower overall drain output (p=0.0001 and p=0.003, respectively), while other factors such as age <60 yr and BMI <25 kg/m2 were not (Table 2).
The mean drainage duration was 3.3 days for the fibrin glue group and 3.8 days for the control group (p=0.067). The overall drain output was 174 mL for the fibrin glue group and 197 mL for the control group (p=0.309). The differences between groups for these two factors were not found to be statistically significant (Table 2). In addition, the fibrin glue and control groups were found to be similar in terms of the incidence of seroma, postoperative bleeding and wound infection (Table 4).
Participants were classified according to two categorical factors and the data underwent an analysis of variance. One factor was the use of fibrin glue and the other factor was the axillary dissection level or node status. The variance between groups classified according to the use of fibrin glue and axillary dissection level was significant in terms of drainage duration (p=0.0005) and overall drain output (p=0.0098) (Table 3). The drainage duration was shorter (3.5 vs. 4.7 days; p=0.0006) and the overall drain output was lower (196 vs. 278 mL; p=0.0255) in the fibrin glue group compared with the control group among those undergoing level II or III axillary dissection. These differences were not apparent in those undergoing level I axillary dissection. While the data appeared to suggest there may have been a greater benefit from the use of fibrin glue in patients with a positive node status compared with a negative node status, the differences were not statistically significant (p=0.0818 for drainage duration and p=0.1123 for overall drain output).
While prolonged axillary lymphatic drainage is not a serious complication after axillary dissection in breast cancer, it remains the main cause of prolonged hospital stays resulting in increased health care costs. Therefore, several approaches have been used to reduce axillary lymphatic drainage, such as the use of fibrin glue and immobilization of the affected arm (11).
Although Lindsey et al. (12) reported that fibrin glue reduced lymphatic drainage in rats, conflicting results have been reported in clinical trials. Five studies (4-6, 9, 13) have examined the association between fibrin glue use and drainage duration or overall drain output. Three of those studies (4-6) showed that fibrin glue reduced both axillary lymphatic drainage and drainage duration, while two (9, 13) reported that fibrin glue had no effect on either axillary lymphatic drainage and drainage duration. Moreover, a meta-analysis of several published trials (8) reported that while the data appeared to suggest decreased overall drain output and a shorter drainage duration in patients receiving fibrin sealant, the findings were not statistically significant. Those studies enrolled almost exclusively mastectomy cases or various cases rarely involving lumpectomy, therefore making it difficult to accurately evaluate axillary lymphatic drainage due to the influence of fluid from the mastectomy site or the heterogeneity of surgery.
The present study enrolled patients undergoing only breast lumpectomy and axillary dissection to minimize the influence of fluid from mastectomy or lumpectomy. The analysis of all patients showed that fibrin glue use did not reduce the drainage duration or the overall drain output. However, subgroup analysis showed that the use of fibrin glue reduced both drainage duration and overall drain output in patients undergoing level II or III axillary dissection. Fibrin glue had no such effect in patients undergoing level I axillary dissection.
The current study found that in both fibrin glue and control groups, drainage duration and overall drain output increased as the level of axillary dissection or nodal stage increased, and that the benefit from the use of fibrin glue was greater in those undergoing higher level dissections. Moreover, the data suggest that a study using a larger population may find that there is greater benefit from fibrin glue use in node-positive patients compared to node-negative patients. The present results suggest that fibrin glue use will be beneficial under conditions of high drainage, such as axillary dissection extended to two or three levels, higher nodal stage (14), following preoperative chemotherapy, old age (2) and obesity (11). In contrast to previous studies (2, 11), the present study did not find an association between lymphatic drainage and age or obesity. This may have been because in this study the body mass index of participants was restricted ≤30 kg/m2 and the number of participants aged ≥60 yr was only 10.
The current study found that the use of fibrin glue did not prevent seroma formation, which is consistent with other reports (4, 6, 8, 9, 13). One explanation is that perhaps fibrin glue had only a short and transient effect on drainage (4). Despite subgroup analysis showing a shorter drainage duration in the fibrin glue group compared to the control group, the groups did not differ in terms of seroma formation or the number of outpatient clinic visits due to wound issues. Thus, it appears that the use of fibrin glue can reduce the length of hospital stay and has no detrimental effect on the complication rate.
In conclusion, the present results indicate that fibrin glue use can decrease the drainage duration and overall drain output after breast lumpectomy and axillary dissection in patients undergoing level II or III axillary dissection. Thus, fibrin glue use might be recommended in patients at a risk of high lymphatic drainage in order to reduce the length of hospital stays.
Figures and Tables
Fig. 1
Study flow chart.
BMI, body mass index; body weight (kg)/height2 (m2).
*Five patients with postoperative bleeding were excluded.
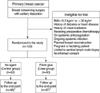
Table 2
Univariate analysis of the association between clinicopathological variables and drainage duration or overall drain output
References
1. O'Hea BJ, Ho MN, Petrek JA. External compression dressing versus standard dressing after axillary lymphadenectomy. Am J Surg. 1999. 177:450–453.
2. Divino CM, Kuerer HM, Tartter PI. Drains prevent seromas following lumpectomy with axillary dissection. Breast J. 2000. 6:31–33.

3. Shamley DR, Barker K, Simonite V, Beardshaw A. Delayed versus immediate exercises following surgery for breast cancer: a systematic review. Breast Cancer Res Treat. 2005. 90:263–271.

4. Gilly FN, Francois Y, Sayag-Beaujard AC, Glehen O, Brachet A, Vignal J. Prevention of lymphorrhea by means of fibrin glue after axillary lymphadenectomy in breast cancer: prospective randomized trial. Eur Surg Res. 1998. 30:439–443.

5. Langer S, Guenther JM, DiFronzo LA. Does fibrin sealant reduce drain output and allow earlier removal of drainage catheters in women undergoing operation for breast cancer? Am Surg. 2003. 69:77–81.
6. Moore M, Burak WE Jr, Nelson E, Kearney T, Simmons R, Mayers L, Spotnitz WD. Fibrin sealant reduces the duration and amount of fluid drainage after axillary dissection: a randomized prospective clinical trial. J Am Coll Surg. 2001. 192:591–599.
7. Moore MM, Freeman MG. Fibrin sealant in breast surgery. J Long Term Eff Med Implants. 1998. 8:133–142.
8. Carless PA, Henry DA. Systematic review and meta-analysis of the use of fibrin sealant to prevent seroma formation after breast cancer surgery. Br J Surg. 2006. 93:810–819.

9. Johnson L, Cusick TE, Helmer SD, Osland JS. Influence of fibrin glue on seroma formation after breast surgery. Am J Surg. 2005. 189:319–323.

10. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001. 357:1191–1194.

11. Christodoulakis M, Sanidas E, de Bree E, Michalakis J, Volakakis E, Tsiftsis D. Axillary lymphadenectomy for breast cancer-the influence of shoulder mobilisation on lymphatic drainage. Eur J Surg Oncol. 2003. 29:303–305.
12. Lindsey WH, Masterson TM, Spotnitz WD, Wilhelm MC, Morgan RF. Seroma prevention using fibrin glue in a rat mastectomy model. Arch Surg. 1990. 125:305–307.

13. Ulusoy AN, Polat C, Alvur M, Kandemir B, Bulut F. Effect of fibrin glue on lymphatic drainage and on drain removal time after modified radical mastectomy: a prospective randomized study. Breast J. 2003. 9:393–396.

14. Petrek JA, Peters MM, Nori S, Knauer C, Kinne DW, Rogatko A. Axillary lymphadenectomy. A prospective, randomized trial of 13 factors influencing drainage, including early or delayed arm mobilization. Arch Surg. 1990. 125:378–382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download