Abstract
The purpose of this study was to determine the effectiveness of antihistamine therapy for withdrawal movements caused by rocuronium injection. One hundred seventy one ASA I-II adults undergoing elective surgery were randomly assigned to one of two groups. Patients in the control group (Group C) were premedicated with 2 mL normal saline, and those in the antihistamine group (Group A) were pre-medicated with 2 mL (45.5 mg) pheniramine maleate. After the administration of thiopental sodium 5 mg/kg, rocuronium 0.6 mg/kg was injected. Withdrawal movements were assessed using a four-grade scale. The administration of antihistamine reveals lower grade of withdrawal movement after rocuronium injection.
Rocuronium bromide is a non-depolarizing aminosteroidal drug characterized by rapid onset and intermediate duration of action. Pain is a common side effect of rocuronium injection, reported to occur in 50-80% of patients (1-3). Conscious patients administered sub-paralyzing doses often suffer severe burning sensation on injection of the drug (4). Even after loss of consciousness, rocuronium injection causes a withdrawal movement of the injected hand or arm. The pathophysiologic mechanism of pain caused by the intravenous (IV) administration of rocuronium injection remains unclear. Changes in plasma histamine concentration after administration of rocuronium are not significant (5). However, analysis of dermal microdialysis-induced mast cell stimulation reveals that high concentrations of rocuronium lead to significant increases in histamine and tryptase release (6, 7). Histamine is widely known for causing pruritus, rarely provokes pain (8), but high concentrations of histamine may activate polymodal nociceptors, resulting in pain production (5, 9). Peripheral veins are innervated with polymodal nociceptors that mediate the pain response to the injection of rocuronium (6, 10). There are no published studies on the incidence and degree of movement against rocuronium injection pain after pretreatment with antihistamines. This randomized, double-blind, placebo-controlled study was designed to evaluate the effectiveness of antihistamine pretreatment in reducing withdrawal movements associated with the administration of rocuronium.
A minimum sample size of 127 cases was required in this study by a statistical power analysis (conducted with α=0.05, power=0.80, and determined by the estimated relative proportions in each category for each group using our observations). After institutional ethics committee approval and informed patient consent were obtained, 171 patients (ages 18 to 65 yr, ASA physical status I or II, undergoing general anesthesia for elective surgery) were recruited for a prospective, randomized, and blinded study. Exclusion criteria are; patients with neurological deficits, opioid or local anesthetic allergies, recent exposure to antihistamines or antidepressants, asthma, pregnancy, those who received analgesics within the previous 24 hr, those with difficult venous access, and those requiring rapid sequence induction. All patients were premedicated with glycopyrrolate 0.2 mg and midazolam 2 mg intramuscularly 30 min before induction of anesthesia. Patients were randomly allocated into two groups using a sealed envelope system. The control group (n=79, group C) received 2 mL of saline, and the antihistamine group (n=92, group A) received pheniramine maleate 2 mL (45.5 mg) at the time of premedication. Patient age, sex, height, weight, body mass index (BMI), and IV site were recorded. All patients were monitored with electrocardiogram, pulse oximeter, and non-invasive arterial pressure on arrival at the operating room. Anesthesia was induced with 2.5% thiopental sodium 5 mg/kg. Just after loss of consciousness, rocuronium 0.6 mg/kg was injected over 5 sec. Crystalloids were then administered at maximum gravity flow. Eight patients in group C and 12 patients in group A were excluded from the study since they received succinylcholine instead of rocuronium, owing to poor mask ventilation or complaints of pain during thiopental sodium administration. To estimate the incidence and degree of the withdrawal movements associated with rocuronium, patient response was graded by the investigator according to the following scale proposed by Ahmad and colleagues (1) (Table 1). Mean arterial pressure (MAP) and heart rate (HR) were recorded before the administration of thiopental sodium (baseline), 1 min after injection of rocuronium, and 1 min after tracheal intubation. Statistical analyses were performed using a statistical package (SPSS 15.0 for Windows, SPSS Inc., Chicago, IL, U.S.A.). Data was expressed as mean±standard deviation (SD) or as number of patients. Demographic data was analyzed using a Student's t-test. The incidence and degree of movements, and site of IV cannula were compared using a chi-square test for trend. The incidence of withdrawal movement according to the site of the IV cannula was analyzed using chi-square test for trend. Hemodynamic variables were analyzed using a one-way repeated measures ANOVA. P<0.05 was considered significant.
No significant differences were noted in terms of demographic variables of patients in Group C and Group A (Table 2). The overall incidence of withdrawal was 84.5% (60/71) in Group C and 70% (56/80) in Group A, and there were no significant differences between two groups. The incidence are greater than expected in grade 3/4 withdrawal movement, and lesser than expected in grade 1/2 withdrawal movement in Group C. Group C reveals lesser incidence than expected value in grade 3/4 withdrawal movement (P=0.008) (Table 3). The overall incidence and grade of withdrawal responses were independent of the site on the IV cannula (Fig. 1). MAP and HR during anesthesia induction were not significantly different between two groups (Table 4).
This study demonstrates that the degree of withdrawal movement associated with the administration of rocuronium injection can be diminished by pretreatment with an antihistamine. The incidence of pain associated with rocuronium injection is high; reports suggest that 50-80% of patients suffer burning sensation (1-3). Withdrawal movements associated with rocuronium injection may negatively affect patient outcomes. Withdrawal movements may induce pulmonary aspiration secondary to gastric regurgitation in unconscious patients (11), cause dislocation or displacement of the IV catheter, or lead to an emergency situation. The exact mechanism of rocuronium-induced pain remains unclear, but it has been reported that the pain may be due to polymodal nociceptor stimulation caused by the osmolality or pH of the solution, and/or by the release of endogenous mediators, such as histamine, bradykinin, kinin and other substances mediating inflammation (12). Rocuronium is supplied as an isotonic solution of pH 4, and pain is known to be induced by low pH injections (13). However, absence of pain in patients receiving 0.9% NaCl adjusted to pH 4 is inconsistent with this hypothesis (12). Several methods have been attempted to reduce this withdrawal movement and pain, with variable results: pretreatment with ondansetron, lidocaine, tramadol, and fentanyl (3), remifentanil (14) and injection of a mixture of rocuronium and sodium bicarbonate (4, 15). Cheong and Wong (2) found that both 10 mg and 30 mg of lidocaine given before the administration of rocuronium significantly reduced the incidence and severity of pain on rocuronium injection in adults, and the larger dose was more effective in adult patients. However, side effects after the pretreatment is possible, such as anaphylaxis (16), coughing (17), chest rigidity, hypotension and bradycardia (18).
The purpose of this study was to determine the effectiveness of antihistamine pretreatment in reducing pain withdrawal associated with rocuronium administration. Pheniramine maleate is an alkylamine antihistamine of which mode of action is achieved by reversible and competitive inhibition of the interaction of histamine with H1 receptors on cells, preventing histamine effects on target organs (8). Several studies have also reported that the analgesic effect of antihistamines (19-21). Although antihistamine has a similar structure to lidocaine, allergic cross reactivity has not been reported. Antihistamine has been recommended as an alternative analgesics for the patients who have allergy to lidocaines (22).
After IV administration of pheniramine maleate, peak plasma concentrations are achieved at 15 min (23), with terminal half-lives estimated to range between 8 and 17 hr. We administrated pheniramine maleate at the time of premedication, 30 min before induction of anesthesia. Although Dalgleish (24) demonstrated that the use of a large vein in the antecubital fossa is likely to minimize the discomfort caused to the patient, discomfort did not depend on the site of IV cannulation in either group in our study. Antihistamine administration caused no significant changes in hemodynamic variables, such as MAP and HR.
In conclusion, we demonstrated that the degree of withdrawal reaction can be attenuated by treatment with an antihistamine before administration of rocuronium . Patients who were pretreated with antihistamine were less likely to suffer pain than those in the control group.
Figures and Tables
 | Fig. 1Response to administration of rocuronium in patients pretreated with antihistamine versus saline depends on intravenous catheter site. Values represent numbers of patients or withdrawal grade. |
Table 3
Incidence and grade of withdrawal movements during intravenous rocuronium injection
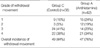
Values represent numbers of patients and percentage of patient response. Under chi-square test for trend, the proportions of observations on different raws vary from column to column (P=0.008).
Withdrawal response 1, no movement; 2, movement at hand or wrist only; 3, movement/withdrawal involving elbow and/or shoulder movement; 4, general response.
References
1. Ahmad N, Choy CY, Aris EA, Balan S. Preventing the withdrawal response associated with rocuronium injection: a comparison of fentanyl with lidocaine. Anesth Analg. 2005. 100:987–990.

2. Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000. 84:106–107.

3. Memis D, Turan A, Karamanlioglu B, Sut N, Pamukcu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002. 94:1517–1520.
4. Chiarella AB, Jolly DT, Huston CM, Clanachan AS. Comparison of four strategies to reduce the pain associated with intravenous administration of rocuronium. Br J Anaesth. 2003. 90:377–379.

5. Koda H, Minagawa M, Si-Hong L, Mizumura K, Kumazawa T. H1-receptor-mediated excitation and facilitation of the heat response by histamine in canine visceral polymodal receptors studied in vitro. J Neurophysiol. 1996. 76:1396–1404.

6. Blunk JA, Seifert F, Schmelz M, Reeh PW, Koppert W. Injection pain of rocuronium and vecuronium is evoked by direct activation of nociceptive nerve endings. Eur J Anaesthesiol. 2003. 20:245–253.

7. Koppert W, Blunk JA, Petersen LJ, Skov P, Rentsch K, Schmelz M. Different patterns of mast cell activation by muscle relaxants in human skin. Anesthesiology. 2001. 95:659–667.

8. Nagy I. Evers AS, Maze M, editors. Sensory processing. Anesthetic Pharmacology: Physiologic principles and Clinical Practice. 2004. 1st ed. Philladelphia: Elsevier Inc.;187–198.
9. Simone DA, Alreja M, LaMotte RH. Psychophysical studies of the itch sensation and itchy skin ("alloknesis") produced by intracutaneous injection of histamine. Somatosens Mot Res. 1991. 8:271–279.

10. Arndt JO, Klement W. Pain evoked by polymodal stimulation of hand veins in humans. J Physiol. 1991. 440:467–478.

11. Lui JT, Huang SJ, Yang CY, Hsu JC, Lui PW. Rocuronium-induced generalized spontaneous movements cause pulmonary aspiration. Chang Gung Med J. 2002. 25:617–620.
12. Borgeat A, Kwiatkowski D. Spontaneous movements associated with rocuronium: is pain on injection the cause? Br J Anaesth. 1997. 79:382–383.

13. Klement W, Arndt JO. Pain on i.v. injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991. 66:189–195.

14. Choi BI, Choi SH, Shin YS, Lee SJ, Yoon KB, Shin SK, Lee KY. Remifentanil prevents withdrawal movements caused by intravenous injection of rocuronium. Yonsei Med J. 2008. 49:211–216.

15. Turan A, Memis D, Karamanlioglu B, Sut N, Pamukcu Z. The prevention of pain from injection of rocuronium by magnesium sulphate, lignocaine, sodium bicarbonate and alfentanil. Anaesth Intensive Care. 2003. 31:277–281.

16. Chin TM, Fellner MJ. Allergic hypersensitivity to lidocaine hydrochloride. Int J Dermatol. 1980. 19:147–148.

17. Phua WT, Teh BT, Jong W, Lee TL, Tweed WA. Tussive effect of a fentanyl bolus. Can J Anaesth. 1991. 38:330–334.

18. Joshi GP, Warner DS, Twersky RS, Fleisher LA. A comparison of the remifentanil and fentanyl adverse effect profile in a multicenter phase IV study. J Clin Anesth. 2002. 14:494–499.

19. Orhan ME, Yuksel U, Bilgin F, Dogrul A. Comparison of the local anesthetic effects of chlorpheniramine, midazolam, lidocaine, and normal saline after intradermal injection. Med Sci Monit. 2007. 13:PI7–PI11.
21. Apiliogullari S, Keles B, Apiliogullari B, Balasar M, Yilmaz H, Duman A. Comparison of diphenhydramine and lidocaine for prevention of pain after injection of propofol: a double-blind, placebo-controlled, randomized study. Eur J Anaesthesiol. 2007. 24:235–238.
22. Green SM, Rothrock SG, Gorchynski J. Validation of diphenhydramine as a dermal local anesthetic. Ann Emerg Med. 1994. 23:1284–1289.

23. Witte PU, Irmisch R, Hajdu P. Pharmacokinetics of pheniramine (Avil) and metabolites in healthy subjects after oral and intravenous administration. Int J Clin Pharmacol Ther Toxicol. 1985. 23:59–62.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download