Abstract
Although cabergoline is effective in the treatment of micro- and macro-prolactinoma, little is known about its efficacy in the treatment of invasive giant prolactinoma. We investigated the efficacy and safety of cabergoline in 10 male patients with invasive giant prolactinoma. Before treatment, mean serum prolactin level was 11,426 ng/mL (range, 1,450-33,200 ng/mL) and mean maximum tumor diameter was 51 mm (range, 40-77 mm). Three months after initiation of cabergoline treatment, serum prolactin concentrations decreased more than 97% in 9 patients; at last follow-up (mean treatment duration, 19 months), the mean decrease in serum prolactin concentrations was 98%, with 5 patients having normal serum prolactin levels. At first MRI follow-up (3-12 months after initiation of cabergoline), the mean reduction in tumor size was 85±4% (range, 57-98%). Cabergoline treatment for more than 12 months caused a greater reduction in tumor size compared to the treatment for less than 12 months (97±1% vs. 78±7%, P<0.05). These findings indicate that cabergoline treatment led to a significant and rapid reduction in serum prolactin concentrations and tumor size in patients with giant prolactinoma. Therefore, cabergoline represents an effective and well-tolerated treatment for invasive giant prolactinoma.
Prolactinoma is the most common functioning pituitary adenoma with excellent medical response. Invasive giant prolactinoma, an extreme subset of prolactinoma, is characterized by large size (>40 mm in diameter), high aggressiveness, massive extrasellar involvement and very high plasma prolactin levels, usually >1,000 ng/mL (1, 2). Although microprolactinoma is found predominantly in young female patients, invasive giant prolactinoma is prevalent in young male patients (3). Patients with giant prolactinoma usually present with symptoms or signs caused by the compression of surrounding structures by large or invasive tumors, including headache, visual disturbance, and/or diplopia. Many patients also have symptoms or signs of hypopituitarism, including hypogonadism.
Dopamine agonists are used in the first line treatment for prolactinoma. Surgery is indicated for patients non-responsive or intolerant to dopamine agonists, as well as in patients with invasive macroadenomas and compromised vision who do not rapidly improve after medical treatment. Although the dopamine agonist bromocriptine has been widely used in patients with prolactinoma, the more recently developed dopamine agonist cabergoline is longer-acting and more selective for the dopamine type 2 (D2)-receptor. Moreover, cabergoline has been found to be more effective and better tolerated than bromocriptine in normalizing prolactin levels and shrinking tumors in both men and women (4). Here we report 10 cases of invasive giant prolactinoma, which were successfully treated with cabergoline alone.
The present study included all patients, who were diagnosed with invasive giant prolactinoma at the pituitary clinic of Asan Medical Center between April 2003 and June 2007 and treated only with cabergoline. All met the criteria for invasive giant prolactinomas: tumor diameter >40 mm, serum prolactin concentrations >1,000 ng/mL, and invasive extrasellar tumor growth. None of these patients had undergone surgery or radiotherapy for prolactinoma and none had a history of treatment with dopamine agonists. This study was performed retrospectively and approved by the ethical review board of Asan Medical Center. All individuals agreed to participate in the study and gave informed consent.
All patients received oral cabergoline at a starting dose of 0.5 mg once weekly. Based on serum prolactin concentrations, the dose of cabergoline was increased 0.5 mg/week every 3 to 6 months, to a maximum dose of 1.5 mg twice per week (total 3 mg per week). During treatment, all patients visited the clinic every 3 months, at which time serum prolactin concentrations were monitored. All patients were asked to report any side effects. Other pituitary function tests were performed before and during treatment, if warranted. Change in tumor size was monitored using sellar magnetic resonance imaging (MRI).
Serum prolactin levels were measured by an immunoradiometric assay using commercial kits (TFB, Tokyo, Japan). The lowest detectible level of serum prolactin is 1.0 ng/mL, and its intra- and inter-assay coefficients of variation for prolactin concentrations were 7.1% and 3.6% respectively. The reference prolactin levels for men are 1.5-9.7 ng/mL. If serum prolactin levels were over 300 ng/mL, serum were serially diluted and subjected to remeasurement. Serum total testosterone concentrations were determined by radioimmunoassay (Adaltis Italia S.P.A., Italy) and the reference levels for testosterone are 2.8-8.8 ng/mL.
Pituitary tumor volume was evaluated using 0.5 or 1.5 T MRI scanners in the sagittal, coronal, and axial planes before and after gadolinium administration. Pituitary tumor volume was calculated from the major transverse, antero-posterior and cranio-caudal diameters. Pituitary tumor shrinkage was evaluated by the percentage reduction in tumor volume.
During the study period, 10 male patients were diagnosed with invasive giant prolactinoma; at diagnosis, mean age was 37±4 yr (range, 25-59 yr). Of these 10 patients, 4 had visual field defects and headache and 3 had only headache. One patient (No. 10) had nasal obstruction and bleeding, which resulted from a tumor growing downward to the infrasellar area. The remaining two patients had no symptoms; their tumors were accidentally found during routine checkup of brain MRI or CT. Seven patients had low serum testosterone concentrations (<2.8 ng/mL), and one (No. 2) had panhypopituitarism at diagnosis. Before treatment, mean serum prolactin concentration was 11,426 ng/mL (range, 1,450-33,200 µg/mL) and mean maximal tumor diameter was 51 mm (range, 40-77 mm).
Seven patients received 0.5-1 mg cabergoline per week with no dose increment throughout the treatment period. The dose of cabergoline was increased to 2 mg per week in 2 patients (Nos. 7 and 10) and to 3 mg per week in one patient (No. 6). Average treatment duration was 19 months (range, 9-43 months). Cabergoline was well tolerated by all patients. None of the patients required dose reduction or discontinuation due to side effects.
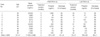
After 3 months of cabergoline treatment, serum prolactin concentrations were decreased dramatically (Table 1, Fig. 1). In all patients except one (No. 7), serum prolactin concentration was reduced by 97% after 3 months of treatment. At the last follow-up, average serum prolactin levels were decreased by 98%, with 6 of the 10 patients having serum prolactin concentrations <20 ng/mL. Patient No. 7, who experienced only a 33% decrease at 3 months due to irregular medication, showed an 89% decrease in serum prolactin concentration after 9 months of treatment. These findings indicate that cabergoline treatment was very effective in reducing serum prolactin levels in all patients with invasive giant prolactinoma.
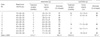
When we analyzed changes in tumor size during cabergoline treatment, we observed a significant reduction (mean, 85±4%; range, 57-98%) at first MRI follow-up, performed after 3 to 12 months of treatment (Table 2, Fig. 2). Except for Patient No. 7, all patients showed a significant decrease in tumor size within 6 months of treatment (mean, 86±3%; range, 70-90%). A further reduction in tumor size was observed with a longer duration of cabergoline treatment. Cabergoline treatment for >12 months caused a greater reduction in tumor size compared with the treatment for <12 months (97±1% vs. 78±7%, P<0.05), indicating that long-term cabergoline treatment was very efficient for reduction of tumor size in giant prolactinoma.
During treatment, three patients showed improvements in visual field defects. Serum testosterone concentrations returned to the normal level in three of seven patients who had initially hypogonadism (mean testosterone levels; 1.2 to 4.0 ng/mL). There was no further decrease in other pituitary hormones during cabergoline treatment (data not shown).
In the present study, the patients with invasive giant prolactinoma were all males. Prolactinomas in males are known to be more invasive and growing more rapidly (5), suggesting that male prevalence of large prolactinoma may be due to its aggressive nature, not merely due to delayed diagnosis (6). The extreme aggressive type of macroprolactinoma is invasive giant prolactinoma.
A previous study reported that long-term cabergoline treatment (mean duration, 15 months) in males and females with macroprolactinoma resulted in a 61% prolactin normalization rate and a 66% tumor shrinkage rate (7). Similarly, in another study, the rate of prolactin normalization was approximately 75% in males with macroprolactinoma following 24 months of cabergoline treatment (8). There were two previous studies showing the outcomes of cabergoline treatment in giant prolactinoma (2, 9). In one study, cabergoline treatment normalized prolactin concentrations in 5 of 10 men with giant prolactinoma. Furthermore, in the remaining five patients, serum prolactin levels were decreased by 94% of the pretreatment levels after a mean 39 months of cabergoline therapy (9). In the other study, cabergoline treatment for 1-50 months normalized prolactin levels in eight out of ten patients with giant prolactinoma (2).
Consistent with the previous reports, our study showed that cabergoline induced a profound reduction (>95%) in serum prolactin levels within 3 months in 7 among 10 patients. At last follow-up (average treatment duration, 19 months), serum prolactin levels were decreased to 2% of basal levels in all 10 patients and normalized in 5 patients. Tumor shrinkage was significant (86% reduction) within 6 months although a further decrease (97%) in tumor size was observed after >12 months of cabergoline treatment. Compared to the previous reports (2, 9), our data showed that lower dose (0.5-1 mg/week) of cabergoline treatment induced more rapid decreases in both serum prolactin levels and tumor volume. The reason for the excellent outcome in our patients is unclear. However, it may result from that our study included the patients with more aggressive prolactinoma as suggested by larger tumor size and higher basal prolactin levels.
When we reviewed the outcome of bromocriptine treatment in giant prolactinoma, bromocriptine treatment for more than 5 yr caused an overall 99.8% decrease in prolactin levels and a mean 68% decrease in tumor volume (1). Although outcomes of bromocriptine treatment are comparable to those of cabergoline, some patients are intolerant to bromocriptine due to side effects such as nausea, orthostatic dizziness, fatigue and nasal congestion (10). In our study, none of the patients experienced any adverse effects during cabergoline treatment, and none experienced disturbances in the other pituitary functions or cerebrospinal fluid rhinorrhea, a rare complication of dopamine agonist treatment (11-13). Thus cabergoline treatment is safe and well-tolerated.
Complete surgical removal of giant prolactinomas via the transsphenoidal approach is very difficult because these tumors invade local surrounding structures, including the cavernous sinus and optic chiasm. Therefore, the persistence and recurrence of giant prolactinoma after surgery are very high (14, 15). Biochemical cure is also rare even after extensive tumor removal. Indeed, during the same study period, nine patients were diagnosed with invasive giant prolactinoma but underwent transsphenoidal tumor resection before a referral to our department. Although serum prolactin concentrations were significantly decreased by surgery (from 2,655±474 to 381±187 ng/mL), normalization of serum prolactin levels or complete tumor resection was not achieved by surgery in all patients (unpublished data), requiring additional medical treatment.
Our study has limitations; it was a retrospective and non-controlled study with small number of patients. However, our data indicate that cabergoline treatment is a safe and effective treatment in male patients with invasive giant prolactinomas.
Figures and Tables
Fig. 1
Serum prolactin concentrations before and during cabergoline treatment in 10 men with invasive giant prolactinoma.

Fig. 2
Serial follow-up of gadolinium-enhanced T1 weighted magnetic resonance imaging before and during cabergoline treatment. Four patients had giant prolactinoma with cavernous sinus invasion and suprasellar and infrasellar extension before treatment. Significant tumor shrinkage was induced by cabergoline treatment.
Tx, treatment; mo, months.

References
1. Shrivastava RK, Arginteanu MS, King WA, Post KD. Giant prolactinomas: clinical management and long-term follow up. J Neurosurg. 2002. 97:299–306.

2. Shimon I, Benbassat C, Hadani M. Effectiveness of long-term cabergoline treatment for giant prolactinoma: study of 12 men. Eur J Endocrinol. 2007. 156:225–231.

3. Schaller B. Gender-related differences in prolactinomas. A clinicopathological study. Neuro Endocrinol Lett. 2005. 26:152–159.
4. Biller BM, Molitch ME, Vance ML, Cannistraro KB, Davis KR, Simons JA, Schoenfelder JR, Klibanski A. Treatment of prolactin-secreting macroadenomas with the once-weekly dopamine agonist cabergoline. J Clin Endocrinol Metab. 1996. 81:2338–2343.

5. Delgrange E, Trouillas J, Maiter D, Donckier J, Tourniaire J. Sex-related difference in the growth of prolactinomas: a clinical and proliferation marker study. J Clin Endocrinol Metab. 1997. 82:2102–2107.

6. Hulting AL, Muhr C, Lundberg PO, Werner S. Prolactinomas in men: clinical characteristics and the effect of bromocriptine treatment. Acta Med Scand. 1985. 217:101–109.

7. Ferrari CI, Abs R, Bevan JS, Brabant G, Ciccarelli E, Motta T, Mucci M, Muratori M, Musatti L, Verbessem G, Scanlon MF. Treatment of macroprolactinoma with cabergoline: a study of 85 patients. Clin Endocrinol (Oxf). 1997. 46:409–413.

8. Colao A, Vitale G, Cappabianca P, Briganti F, Ciccarelli A, De Rosa M, Zarrilli S, Lombardi G. Outcome of cabergoline treatment in men with prolactinoma: effects of a 24-month treatment on prolactin levels, tumor mass, recovery of pituitary function, and semen analysis. J Clin Endocrinol Metab. 2004. 89:1704–1711.

9. Corsello SM, Ubertini G, Altomare M, Lovicu RM, Migneco MG, Rota CA, Colosimo C. Giant prolactinomas in men: efficacy of cabergoline treatment. Clin Endocrinol (Oxf). 2003. 58:662–670.

11. Suliman SG, Gurlek A, Byrne JV, Sullivan N, Thanabalasingham G, Cudlip S, Ansorge O, Wass JA. Nonsurgical cerebrospinal fluid rhinorrhea in invasive macroprolactinoma: incidence, radiological, and clinicopathological features. J Clin Endocrinol Metab. 2007. 92:3829–3835.

12. Leong KS, Foy PM, Swift AC, Atkin SL, Hadden DR, MacFarlane IA. CSF rhinorrhoea following treatment with dopamine agonists for massive invasive prolactinomas. Clin Endocrinol (Oxf). 2000. 52:43–49.

13. Baskin DS, Wilson CB. CSF rhinorrhea after bromocriptine for prolactinoma. N Engl J Med. 1982. 306:178.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download