Abstract
The incidence of ischemic heart disease has been increased rapidly in Korea. However, the clinical effects of antecedent hypertension on acute myocardial infarction have not been identified. We assessed the relationship between antecedent hypertension and clinical outcomes in 7,784 patients with acute myocardial infarction in the Korea Acute Myocardial Infarction Registry during one-year follow-up. Diabetes mellitus, hyperlipidemia, cerebrovascular disease, heart failure, and peripheral artery disease were more prevalent in hypertensives (n=3,775) than nonhypertensives (n=4,009). During hospitalization, hypertensive patients suffered from acute renal failure, shock, and cerebrovascular event more frequently than in nonhypertensives. During follow-up of one-year, the incidence of major adverse cardiac events was higher in hypertensives. In multi-variate adjustment, old age, Killip class ≥III, left ventricular ejection fraction <45%, systolic blood pressure <90 mmHg on admission, post procedural TIMI flow grade ≤2, female sex, and history of hypertension were independent predictors for in-hospital mortality. However antecedent hypertension was not significantly associated with one-year mortality. Hypertension at the time of acute myocardial infarction is associated with an increased rate of in-hospital mortality.
Hypertension is an established risk factor for adverse cardiovascular outcomes, including heart failure, myocardial infarction, stroke and cardiovascular death (1-5). The incidence of morbidity and mortality related to myocardial infarction and coronary heart disease has been increased in Korea. The prevalence of antecedent hypertension in patients with acute myocardial infarction (AMI) varies from 31% to 59% (6-8). Several studies have reported that a history of hypertension was shown to be associated with an increased rate of adverse outcomes after AMI such as stroke, heart failure and cardiovascular death (9, 10). Although exact mechanisms are not clear, the increased incidence of AMI or sudden death in hypertensive patients seems to be related to endothelial damage, atherosclerosis, insulin resistance, left ventricular hypertrophy, and ventricular arrhythmias (11). However, long-term prognostic impact is still controversial. Nevertheless, Korea Acute Myocardial Infarction Registry (KAMIR) is in search for better AMI management and preventive care, as well as investigating the risk factors for mortality in AMI patients.
The aim of the present study was to evaluate the impact of hypertension on the in-hospital events as well as one year clinical outcomes of patients with AMI in the Korean population.
The KAMIR is a prospective, multi-center and observational on-line registry designed to examine current epidemiology, in-hospital management, and outcome of patients with AMI in Korea. A total of 50 university hospitals and community hospitals with facilities for percutaneous coronary intervention (PCI) and on-site cardiac surgery, were registered in KAMIR. This study protocol included age, sex, body mass index, initial symptom, vital sign, Killip class, symptom onset time, ambulance arrival time, first medical contact time, transfer time from the first hospital to the primary PCI centers, door to needle time, door to balloon time, risk factors, past medications, co-morbidities, electrocardiographic locations of AMI, initial treatment strategy, drugs, coronary angiographic findings, in-hospital complications, medical therapy in hospital and 1, 6, 12-month follow-up major adverse cardiac event (cardiac death, reinfarction, re-PCI, coronary artery bypass graft) (12, 13).
A total of 8,568 patients with acute MI were enrolled in KAMIR from November 2005 to December 2006, and 7,784 patients (5,430 male and 2,354 female, 64.4±12.9 yr) were evaluated in the present study.
AMI was diagnosed if typical rise and gradual fall (troponin) or more rapid rise and fall (creatine kinase-MB) with at least one of the following criteria were satisfied: 1) ischemic symptoms, 2) development of pathologic Q waves on the electrocardiographic reading, 3) electrocardiographic changes indicative of ischemia (ST-segment elevation or depression), 4) coronary artery intervention. Acute myocardial infarction was subcategorized into ST-segment elevation myocardial infarction (STEMI) or non-ST-segment myocardial infarction (NSTEMI). STEMI was manifested by ST-segment elevations or hyperacute T waves, and then by T wave inversions, often associated with evolution of pathologic Q waves. Clinically significant ST-segment elevation is considered to be present if it is greater than 1 mm (0.1 mV) in at least two contiguous precordial leads or in at least two adjacent limb leads and is not attributable to non-ischemic causes. NSTEMI was manifested by ST-segment depressions or T wave inversions without Q waves with corroborating laboratory evidence of infarction.
Information on antecedent hypertension and other baseline data were assessed at first visit. Patients who reported a diagnosis of hypertension were considered to have hypertension or antihypertensive medications antecedent to their MI. Blood pressure was recorded at first visit and patients with a systolic blood pressure <90 mmHg on admission were considered to have low blood pressure. The left ventricular ejection fraction (LVEF) was obtained and averaged in apical 4- and 2-chamber views by modified Simpson's method.
Initial treatment strategy was composed of reperfusion therapy, including primary PCI, facilitated PCI and thrombolytics, and conservative treatment in STEMI and early invasive treatment including early invasive PCI and early conservative treatment in NSTEMI. Primary PCI was defined as: 1) PCI that was performed within 12 hr at admission, 2) PCI that was performed after 12 hr at admission because of continuing symptom, 3) PCI that was performed within 36 hr at admission because of cardiogenic shock. Facilitated PCI refers to a strategy of planned immediate PCI after administering drugs to reduce blood vessel obstruction before the procedure. Early invasive PCI was defined as PCI in NSTEMI within 48 hr because of continuing symptom. Elective PCI was defined as scheduled PCI in patients without symptom.
MACE at 6 months and one-year clinical follow-up were evaluated. MACE was defined as the composite of 1) all cause death, 2) non-fatal MI, and 3) re-PCI or coronary artery bypass graft (CABG). All data were recorded on a standardized, electronic, web page-based case report form (http://www.kamir.or.kr) (12, 13).
The statistical Package for Social Sciences (SPSS) for Windows, version 12.0 (Chicago, IL, U.S.A.) was used for all analyses. Continuous variables were presented as the mean value±SD; comparisons were conducted by Student's t-test. Discrete variables were presented as percentages and relative frequencies and comparisons were conducted by chi-square statistics or Fisher's exact test as appropriate. Logistic regression analysis was performed to identify the independent predictors of primary end points. A P value <0.05 was considered statistically significant.
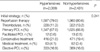
In Table 1, 7,784 eligible patients (5,430 male and 2,354 female, 64.4±12.9 yr) were analyzed. Among them, 3,775 patients (48.5%) reported antecedent hypertension.
The patients with antecedent hypertension were older (66.8±11.9 yr vs. 62.1±13.4 yr, P<0.001) and more often female (38.4%±22.6%, P<0.001) than the normotensive patients.
On admission, systolic and diastolic blood pressures were higher in the patients with antecedent hypertension. Diabetes mellitus, hyperlipidemia, heart failure, cerebrovascular disease, peripheral artery disease, previous MI, previous angina, previous PCI and previous CABG were more significantly common in hypertensives, compared with in normotensives. On admission, the hypertensive patients more frequently presented with non ST-segment elevations on the electrocardiogram (44.7% vs. 36.6%, P<0.001).
The level of serum creatinine, glucose, triglyceride, N-terminal pro-brain natriuretic peptide (NT-proBNP) were higher in hypertensives than in nonhypertensives, but the level of maximum creatine kinase-MB and low density lipoprotein-cholesterol were lower.
There were no differences in initial treatment strategy of STEMI between the two groups (Table 2). However, hypertensives received more frequently conservative treatments in NSTEMI (45.0% vs. 38.1%, P<0.001).
Left anterior descending artery (LAD) was the most common infarct related artery (IRA) in both two groups. LAD was the less common IRA in hypertensives than in nonhypertensives (47.0% vs. 50.6%, P=0.006). Multivessel disease was more common in hypertensives (63.6% vs. 48.4%, P<0.001). Lesion type B2 or C according to the American College of Cardiology/American Heart Association (ACC/AHA) classification was more common in hypertensives (79.2% vs. 77.0%, P=0.039). Thrombolysis In Myocardial Infarction (TIMI) 0-1 flow was present in 53.7% in hypertensives and 55.4% in nonhypertensives (P=0.186).
There was no difference in TIMI flow grade 3 after procedures in the two groups. Drug eluting stent was used in most cases in both groups (91.5% vs. 92.2%, P=0.379). The average diameter of stents was larger in nonhypertensives (3.2±0.4 mm) than in hypertensives (3.1±0.4 mm) (P<0.001). The number of implanted stents were significantly higher in hypertensives compared with nonhypertensives (1.6±0.9 vs. 1.5±0.8, P<0.001).
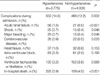
In Table 3, the hypertensive patients suffered from a higher incidence of complications during admission (14.6% vs. 12.2%, P=0.002), acute renal failure (1.5% vs. 0.5%, P<0.001), shock (0.7% vs. 0.4%, P=0.046), major bleeding (0.7% vs. 0.4%, P=0.046) and cerebrovascular disease (0.9% vs. 0.5%, P=0.033) than the nonhypertensive group. The incidence of in-hospital death was significantly higher in hypertensives (5.9% vs. 4.0%, P<0.001).
The hypertensive patients were more frequently prescribed various medications at the time of discharge from hospital, including angiotensin receptor blocker (21.9% vs. 14.7%, P<0.001), beta blocker (71.0% vs. 67.6%, P=0.002), calcium channel blocker (15.7% vs. 9.9%, P<0.001) and diuretics (24.8% vs. 20.7%, P<0.001) as compared with the nonhypertensive patients.
To find clinical factors that could predict the occurrence of in-hospital death, we used a logistic regression model in which in-hospital death was the dependent variable. The following risk factors were entered as independent variables: old age, female sex, post procedural TIMI flow grade ≤2, systolic blood pressure <90 mmHg on admission, LVEF <45%, Killip class ≥III, multivessel disease, antecedent hypertension, diabetes mellitus, and administration of reperfusion therapy. Results of logistic regression demonstrated that old age, post procedural TIMI flow grade ≤2, systolic blood pressure <90 mmHg on admission, LVEF <45%, Killip class ≥III, multivessel disease and antecedent hypertension were independent predictors for in-hospital mortality (Table 4).
The cumulative incidence of MACE at one year was 27.6% in hypertensives and 22.7% in nonhypertensives (P=0.001). Cardiac death during one-year occurred in 16.1% in hypertensives and 11.0% in nonhypertensives (P<0.001). However, the rates of non-cardiac death, myocardial infarction, re-PCI and CABG were not different between the two groups during one-month and one-year follow-up.
To find clinical factors that could predict the occurrence of one-year mortality, we used a logistic regression model in which one-year mortality was the dependent variable. The following risk factors were entered as independent variables: old age, female sex, post procedural TIMI flow grade ≤2, LVEF <45%, Killip class ≥III, multivessel disease, antecedent hypertension, diabetes mellitus, the use of bare metal stents, administration of reperfusion therapy and beta blockers. Results of logistic regression demonstrated that old age, Killip class ≥III and multivessel disease were independent predictors for one-year mortality. However, antecedent hypertension was no longer an independent predictor of one-year mortality (Table 5).
KAMIR study revealed that a history of hypertension independently contributed to a higher in-hospital mortality in patients of AMI. However, we did not find significant association between antecedent hypertension and one-year mortality by multivariate analysis.
Epidemiologic studies of treated and untreated hypertensive patients confirmed that there were gradually increasing incidence of coronary disease, stroke and cardiovascular mortality as the blood pressure rises above 110/75 mmHg (14). Similar observations have been made in patients with known coronary heart disease (CHD) (15). CHD is estimated to be the leading cause of death in the developing as well as in the developed world. In particular, several studies have reported that antecedent hypertension after myocardial infarction is associated with adverse cardiovascular outcomes such as stroke, heart failure, and cardiovascular death (9, 10, 16). Although mortality rates for CHD including AMI have been declined in several developed countries in the past decades (17, 18), the incidence of CHD including AMI and mortality rate from the case fatality have been increased in Korea (19, 20).
Similar to previous study (21), KAMIR revealed the differences in demographic parameters in antecedent hypertensives with AMI compared with normotensives. The hypertensive patients tend to be older, and female. There is also a greater prevalence of diabetes mellitus, hyperlipidemia, heart failure, cerebrovascular disease, peripheral artery disease, and previous coronary heart disease with PCI.
The hypertensive patients received different pharmacological treatment from nonhypertnesives in AMI. In our study, no differences were observed in the use of aspirin, clopidogrel, angiotensin converting enzyme inhibitor, nitrate, nicorandil or statin. However, the hypertensive patients received angiotensin receptor blocker, beta blocker and calcium channel blocker more frequently than the nonhypertensive patients. The comorbidity associated with arterial hypertension such as heart failure and angina pectoris may be responsible for the increased protective prescription of medication in these patients. PCI, if performed in a timely fashion, is the reperfusion therapy of choice in patients who have had AMI (22, 23). In reality, Song et al. (24) have reported that the rate of primary PCI in Korea was much higher than other countries, and the KAMIR data confirmed this higher rate. There was no difference in revascularization rate in both two groups. Low systolic pressure on admission was an independent predictor of in-hospital mortality.
Mauri et al. (25) have reported that a history of hypertension in AMI was associated with an increased risk of hemodynamic complications and an increased incidence of sudden death. Our results also revealed that old age, low post procedural TIMI flow grade, low systolic blood pressure on admission, low LVEF, high Killip class, multivessel disease and antecedent hypertension were strongly associated with in-hospital mortality. Hypertension also increased risk of cardiac death and overall MACE during one-month, and one-year follow-up after MI. Multi-vessel disease and complex lesion in coronary angiography also associated with poor outcomes in hypertensive patients (26). However, in contrast to previous study (27), our study did not reveal that a history of hypertension independently contributes to a higher mortality during one-year of follow-up. The poor outcomes after AMI are probably attributable not to antecedent hypertension but to the concomitant existence of other risk factors such as an old age, high Killip class and multivessel disease. These factors are known to imply poorer prognosis in myocardial infarction (28). White et al. (29) reported that clinical outcomes remained poor in elderly patients with heart failure and/or impaired left ventricular systolic function after acute myocardial infarction, although most received beta-blockers and all received an ACE inhibitor and/or an angiotensin receptor blocker.
This study has several limitations. First, our study is multicenter prospective registry, and it was not a randomized, controlled study. Thus, there could have been a selection bias in enrolled patients. Second, the patients of undetected hypertension with low blood pressure on admission was left out in the analysis and some people were not followed up for one year. Therefore, there was a possibility of higher mortality in patients with AMI. Third, we obtained the results for the blood test from different laboratories, therefore it was possible that different laboratories may produce different results for the same sample of blood. Fourth, a value of blood pressure at follow-up was not recorded in the registry, therefore the relation between the adequate control of blood pressure and the prognosis of the patients was not estimated. Fifth, whether long term and more aggressive treatment of elevated blood pressure in patients with AMI can reduce adverse outcomes or not remains unknown (10).
There are large-scale, nationwide or worldwide AMI registration programs, such as A National Registry of Myocardial Infarction in the U.S. in 1998, A National Survey of Acute Myocardial infarction and Ischemia (SAMII) in the U.K. in 2000, The Maximal Individual TherRapy of Acute Myocardial Infarction (MITRA) in Germany in 2002 and the Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) projects. The World Health Organization now suggests efficient AMI management systems beyond providing detailed information. KAMIR is also expected to make a contribution to the establishment of better AMI management and preventive care, as well as investigating the risk factors for mortality in AMI patients.
Figures and Tables
Table 1
Baseline clinical and laboratory characteristics

PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-STEMI; HDL-C, High density lipoprotein-cholesterol; LDL-C, Low density lipoprotein-cholesterol; hs-CPR, High sensitivity C-reactive protein; NT-proBNP, N-terminal pro-brain natriuretic peptide.
References
1. Lewis EF, Moye LA, Rouleau JL, Sacks FM, Arnold JM, Warnica JW, Flaker GC, Braunwald E, Pfeffer MA. CARE Study. Predictors of late development of heart failure in stable survivors of myocardial infarction: the CARE study. J Am Coll Cardiol. 2003. 42:1446–1453.

2. Richards AM, Nicholls MG, Troughton RW, Lainchbury JG, Elliott J, Frampton C, Espiner EA, Crozier IG, Yandle TG, Turner J. Antecedent hypertension and heart failure after myocardial infarction. J Am Coll Cardiol. 2002. 39:1182–1188.

3. Witt BJ, Ballman KV, Brown RD Jr, Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J Med. 2006. 119:354.e1–354.e9.

4. Miura K, Daviglus ML, Dyer AR, Liu K, Garside DB, Stamler J, Greenland P. Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men: The Chicago Heart Association Detection Project in Industry. Arch Intern Med. 2001. 161:1501–1508.
5. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002. 360:1903–1913.
6. Willich SN, Müller-Nordhorn J, Kulig M, Binting S, Gohlke H, Hahmann H, Bestehorn K, Krobot K, Völler H. PIN Study Group. Cardiac risk factors, medication, and recurrent clinical events after acute coronary disease; a prospective cohort study. Eur Heart J. 2001. 22:307–313.

7. Piegas LS, Avezum A, Pereira JC, Neto JM, Hoepfner C, Farran JA, Ramos RF, Timerman A, Esteves JP. AFIRMAR Study Investigators. Risk factors for myocardial infarction in Brazil. Am Heart J. 2003. 146:331–338.

8. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, Mc-Queen M, Budaj A, Pais P, Varigos J, Lisheng L. INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004. 364:937–952.

9. Richards AM, Nicholls MG, Troughton RW, Lainchbury JG, Elliott J, Frampton C, Espiner EA, Crozier IG, Yandle TG, Turner J. Antecedent hypertension and heart failure after myocardial infarction. J Am Coll Cardiol. 2002. 39:1182–1188.

10. Thune JJ, Signorovitch J, Kober L, Velazquez EJ, McMurray JJ, Califf RM, Maggioni AP, Rouleau JL, Howlett J, Zelenkofske S, Pfeffer MA, Solomon SD. Effect of antecedent hypertension and follow-up blood pressure on outcomes after high-risk myocardial infarction. Hypertension. 2008. 51:48–54.

11. Rakugi H, Yu H, Kamitani A, Nakamura Y, Ohishi M, Kamide K, Nakata Y, Takami S, Higaki J, Ogihara T. Links between hypertension and myocardial infarction. Am Heart J. 1996. 132:213–221.

12. Korea Acute Myocardial Infarction Registry (KAMIR) Investigators. Lee KH, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi D, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Cho JG, Park SJ. Other Korea Acute Myocardial Infarction Registry Investigators. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol. 2008. 130:227–234.

13. Lee SR, Jeong MH, Ahn YK, Chae SC, Hur SH, Kim YJ, Seong IW, Chae JK, Hong TJ, Rhew JY, Cho MC, Bae JH, Rha SW, Kim CJ, Jang YS, Park SJ. Korea Acute Myocardial Infarction Registry Investigators. Clinical safety of drug-eluting stents in the Korea acute myocardial infarction registry. Circ J. 2008. 72:392–398.

14. Pastor-Barriuso R, Banegas JR, Damian J, Appel LJ. Systolic blood pressure, diastolic blood pressure, and pulse pressure: an evaluation of their joint effect on mortality. Ann Intern Med. 2003. 139:731–739.

15. Sipahi I, Tuzcu EM, Schoenhagen P, Wolski KE, Nicholls SJ, Balog C, Crowe TD, Nissen SE. Effects of normal, pre-hypertensive, and hypertensive blood pressure levels on progression of coronary atherosclerosis. J Am Coll Cardiol. 2006. 48:833–838.

16. Kenchaiah S, Davis BR, Braunwald E, Rouleau JL, Dagenais GR, Sussex B, Steingart RM, Brown EJ Jr, Lamas GA, Gordon D, Bernstein V, Pfeffer MA. Survival and Ventricular Enlargement Trial. Antecedent hypertension and the effect of captopril on the risk of adverse cardiovascular outcomes after acute myocardial infarction with left ventricular systolic dysfunction: Insights from the Survival and Ventricular Enlargement Trial. Am Heart J. 2004. 148:356–364.

17. Kuulasmaa K, Tunstall-Pedoe H, Dobson A, Fortmann S, Sans S, Tolonen H, Evans A, Ferrario M, Tuomilehto J. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet. 2000. 355:675–687.

18. Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007. 356:2388–2398.

19. Khor GL. Cardiovascular epidemiology in the Asia-Pacific region. Asia Pac J Clin Nutr. 2001. 10:76–80.

20. Ko M, Kim MT, Nam JJ. Assessing risk factors of coronary heart disease and its risk prediction among Korean adults: the 2001 Korea National Health and Nutrition Examination Survey. Int J Cardiol. 2006. 110:184–190.

21. Majahalme SK, Smith DE, Cooper JV, Kline-Rogers E, Mehta RH, Eagle KA, Bisognano JD. Comparison of patients with acute coronary syndrome with and without systemic hypertension. Am J Cardiol. 2003. 92:258–263.

22. Mehta RH, Roe MT, Chen AY, Lytle BL, Pollack CV Jr, Brindis RG, Smith SC Jr, Harrington RA, Fintel D, Fraulo ES, Califf RM, Gibler WB, Ohman EM, Peterson ED. Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE initiative. Arch Intern Med. 2006. 166:2027–2034.
23. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intra venous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003. 361:13–20.
24. Song YB, Hahn JY, Gwon HC, Kim JH, Lee SH, Jeong MH. KAMIR investigators. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea Acute Myocardial Infarction Registry. J Korean Med Sci. 2008. 23:357–364.

25. Mauri F, Maggioni AP, Franzosi MG, de Vita C, Santoro E, Santoro L, Giannuzzi P, Tognoni G. A simple electrocardiographic predictor of the outcome of patients with acute myocardial infarction treated with a thrombolytic agent. A Gruppo Italiano per lo Studio della Sopravvivenza nell' Infarto Miocardico (GISSI-2)-Derived Analysis. J Am Coll Cardiol. 1994. 24:600–607.
26. Devereux RB, Roman MJ. Inter-relationships between hypertension, left ventricular hypertrophy and coronary heart disease. J Hypertens. 1993. 11:Suppl. S3–S9.

27. Herlitz J, Bång A, Karlson BW. Five-year prognosis after acute myocardial infarction in relation to a history of hypertension. Am J Hypertens. 1996. 9:70–76.

28. Yagi M, Nakao K, Honda T, Tsurumi Y, Kasanuki H. Clinical characteristics and early outcomes of very elderly patients in the reperfusion era. Int J Cardiol. 2004. 94:41–46.

29. White HD, Aylward PE, Huang Z, Dalby AJ, Weaver WD, Barvik S, Marin-Neto JA, Murin J, Nordlander RO, van Gilst WH, Zannad F, McMurray JJ, Califf RM, Pfeffer MA. VALIANT Investigators. Mortality and morbidity remain high despite captopril and/or Valsartan therapy in elderly patients with left ventricular systolic dysfunction, heart failure, or both after acute myocardial infarction: results from the Valsartan in Acute Myocardial Infarction Trial (VALIANT). Circulation. 2005. 112:3391–3399.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download