Abstract
The aim of this study was to assess the efficacy of consolidation therapy with hexamethylmelamine (HMM) in patients with advanced epithelial ovarian cancer (EOC). Patients treated at our hospital between January 1997 and November 2006 and in documented clinical complete response from advanced ovarian cancer following front-line platinum-based therapy were retrospectively analyzed. The patients treated with HMM were compared to the patients of matched counterpart without consolidation therapy. Of 102 patients enrolled, 49 were treated with HMM and 53 received no consolidation treatment. For patients with HMM and observed patients, the mean age were 54.6 and 55.6 yr; the distribution of stage was similar (P=0.977); the optimal surgery was performed in 36 (73.5%) and 44 (83%) (P=0.336); the recurrence rate were 27 (55.1%) and 33 (62.3%) (P=0.463); and the median progression-free survival were 38 months and 21 months for patients with HMM and observed patients (P=0.235). No treatment-related adverse events were reported during the follow-up period. Although this study failed to show the significant survival benefit of consolidation therapy with HMM in patients with advanced EOC, we consider that our study can contribute data to investigate the effectiveness of consolidation therapy in epithelial ovarian cancer.
Epithelial ovarian cancer (EOC) has the highest death rate among gynecologic malignancies throughout the world, primarily because most patients are diagnosed with advanced stage disease. The standard treatment consists of cytoreductive surgery followed by induction chemotherapy with a taxane/platinum combination. Despite an initial excellent response to chemotherapy, the disease subsequently recurs in most patients and their long-term prognosis is dismal. For patients with optimally debulked stage III ovarian cancer, the median progression-free survival (PFS) is 21 months, with a median overall survival (OS) of 57 months (1). Even patients who attain a complete clinical response (cCR) after primary therapy, as defined by the absence of symptoms, normal examination, serum CA 125 concentration below 35 U/mL and imaging analyses showing no evidence of disease, have a median PFS from completion of therapy of about 21 months (2, 3).
Most patients who attain cCR to primary treatment receive no additional chemotherapy, although the majority will require multiple salvage regimens due to tumor recurrence. Attempts to improve the clinical outcome of EOC patients included the identification of new first-line regimens which are able to induce higher cCR rates and effective treatments to consolidate or maintain the response achieved by first-line chemotherapy (4). Consolidation therapy uses one or more of the multiple chemotherapeutic agents known to be active in recurrent disease (5, 6). One of these agents, hexamethylmelamine (HMM), which has been used to treat recurrent ovarian cancer for many years, is well tolerated (7-11) and is associated with prolonged PFS and OS in the Phase II setting (12). Little is known, however, about outcomes of consolidation therapy in advanced EOC patients; and there have been no comparison studies of HMM consolidation therapy in these patients. We therefore assessed the efficacy of HMM consolidation therapy in advanced EOC patients.
Patients (n=102) with histologically confirmed advanced (stage III or IV) EOC and documented cCR following front-line platinum-based therapy who had been treated at Asan Medical Center between January 1997 and November 2006 were enrolled. All patients had WHO performance status of 2 or less (Karnofsky index >60) and adequate bone marrow (white blood cell count [WBC] >3.0×109/L and platelet count >100×109/L), kidney (serum creatinine <120 µM/L), and liver (liver enzymes ≥2×upper normal limit) function.
Patients (n=49) treated with oral HMM (altretamine) consolidation therapy were retrospectively assessed and compared to the untreated patients (n=53). Each patient in the former group received 260 mg/m2/day HMM for 14 consecutive days of each 28-day cycle, with a maximum of 12 cycles. Treatment was stopped early due to disease progression, unacceptable toxicity, or withdrawal of patient compliance. The patient was followed for recurrence of measurable disease as defined by the study protocol. Patients were also followed by physical examination, pelvic examination, complete blood counts, blood chemistries and CA-125 concentration every 3 months for the first 2 yr and every 6 months thereafter until disease progression, death, or loss to follow-up.
Among clinical and pathological characteristics of patients, optimal debulking was defined as residual tumor <1 cm, suboptimal debulking as residual tumor ≥1 cm. Serum CA-125 concentration was measured 6 weeks after initiation of the front-line chemotherapy. Toxicity was graded according to Gynecologic Oncology Group (GOG) criteria. PFS was estimated from the date of study registration to the date of clinically proven recurrence.
Data analysis was performed using SPSS (version 12.0). The chi-square test, Student's t-test were used to compare clinical and pathologic characteristics of patient groups. PFS analyses were performed using the Kaplan-Meier method and log-rank test. We estimated the parameters in the Cox proportional hazard model using PFS as a dependent variable, CA-125 concentration and debulking status as independent variables, and recurrence as a censoring variable. For all statistical tests, the level of significance was P<0.05.
Of the 102 patients with documented cCR from advanced EOC following front-line platinum-based therapy, 49 received HMM consolidation treatment and 53 received no consolidation treatment. The two groups were similar in age, debulking status, histological type, stage, CA-125 concentration 6 weeks after initiation of first-line therapy, and recurrence rate (Table 1).
Of the 49 HMM-treated patients who received at least one cycle of oral altretamine, 14 patients did ≤3 cycles, 4 patients did 4 to 5 cycles of HMM. Among the patients who received 6-12 cycles (n=31), 12 patients did 12 cycles of HMM.
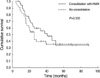
Although the median PFS of the HMM-treated group (38 months; 95% confidence interval [CI] 16-60 months) was longer than that of the untreated group (21 months; 95% CI 16-26 months), the difference was not significant (P=0.235) (Fig. 1).
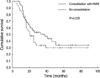
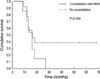
Of patients with optimal debulked disease (residual tumor <1 cm), those who received consolidation treatment had a median PFS of 41 months (95% CI 25-57 months), whereas those who received no treatment had a median PFS of 25 months (95% CI 19-31 months), but there was no significant difference (P=0.333) (Fig. 2). Of patients with suboptimal debulked disease (residual tumor ≥1 cm), median PFS of those who did and did not receive HMM were 16 months (95% CI 10-22 months) and 16 months (95% CI 12-20 months), respectively (P=0.204) (Fig. 3). Using Cox's proportional hazards model, we found that serum CA-125 concentration 6 weeks after initiation of first-line therapy, which means just before the 3rd cycle of adjuvant chemotherapy (P<0.0001), stage (P=0.005), and debulking status (P=0.038) were significant prognostic factors for PFS (Table 2). Gastrointestinal toxicity was the prominent feature in our study group. Four patients discontinued consolidation therapy due to grade 4 toxicity. But most patients with HMM were tolerable during the follow-up period.
Cytoreductive surgery followed by induction chemotherapy with a taxane/platinum combination is currently accepted as the standard regimen for advanced EOC. Despite excellent responses to first-line chemotherapy, most patients with advanced ovarian cancers who achieve cCR relapse after a median time of 18-24 months (13-15). Among attempts made to improve the clinical outcome of EOC patients is maintaining the response achieved by first-line chemotherapy. Maintenance therapy can include cytotoxic chemotherapy, radiation therapy, and/or biological therapy. Several trials have assessed maintenance therapy with single-agent HMM, epirubicin, topotecan, or paclitaxel in patients responsive to first-line platinum-based chemotherapy (2, 16-18).
HMM (altretamine) is a synthetic, cytotoxic, antineoplastic, s-triazine derivative that can be taken orally. Its exact mechanism of action is unknown, although chemically it resembles alkylating agents (19, 20). Vergote et al. reported a 14% response rate of HMM as a single agent in 50 patients with pltinum-resistant disease. And oral altretamine 260 mg/m2/day was given for 14 days every 4 weeks for six cycles to patients with FIGO stage III EOC who obtained a clinical response following platinum-based therapy (12). To date, however, there have been no trials comparing HMM with no treatment in patients with advanced EOC.
The dosage of HMM used in this study was 260 mg/m2/day for 14 days every 4 weeks, for a maximum 12 cycles; and median follow-up was 3.2 yr. 37 of 49 (75.6%) patients with HMM did not receive maximum 12 cycles. HMM therapy for patients received less than 6 cycles (n=18) were caused by a progression of disease, and severe gastrointestinal toxicity. For patients receiving 6 or more cycles of HMM (n=31) the reasons of discontinuation were patient's desire of discontinuation of consolidation therapy due to poor compliance with gastrointestinal discomfort and a loss of follow-up.
Our study failed to show the statistical significance in the median PFS of the HMM-treated group (Fig. 1). The main reason of this results might be a small number of our study. Prospective randomized trials in larger numbers of patients are clearly warranted.
Serum CA-125 is a marker frequently used in evaluating the clinical situation in ovarian cancer patients, and the rate of decline in serum CA-125 during primary chemotherapy has been an important prognostic factor in several multivariate analyses (21). Moreover, postoperative serum CA-125 concentration is an independent prognostic factor in patients with invasive ovarian cancer (22). Reduction in serum CA-125 over the first two cycles of platinum-based chemotherapy is an independent predictor of survival in patients with suboptimal stage III or IV ovarian cancer; patients without significant declines had a particularly poor prognosis (23). In agreement with these findings, our study results showed that CA-125 concentration 6 weeks after initiation of first-line chemotherapy was prognostic for PFS.
We also found that debulking status was a prognostic of PFS in patients with advanced EOC. Our finding is in agreement with that large residual disease after initial surgery is the strongest prognostic variable for tumor recurrence (14, 24, 25). Of our 102 patients, 80 had optimal cytoreductive surgery (residual <1 cm), whereas 22 had suboptimal surgery (residual ≥1 cm). Although all 102 patients achieved cCR following first-line chemotherapy, those with optimal surgery had a better prognosis than those with suboptimal surgery.
The ultimate aim of consolidation therapy is to improve clinical outcome, including prolonged survival rate and better quality of life in patients with EOC. Few studies have investigated consolidaton therapy in patients with advanced EOC. Although our study were retrospective analysis and failed to show the prolonging PFS in patients with advanced EOC by consolidation therapy with HMM, we consider that our study can contribute data to investigate the effectiveness of consolidation therapy in epithelial ovarian cancer.
Figures and Tables
Fig. 2
Progression-free survival of patients with optimal debulked disease (residual tumor <1 cm), treated or untreated with HMM.
References
1. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, Mannel RS, DeGeest K, Hartenbach EM, Baergen R. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003. 21:3194–3200.

2. Markman M, Liu PY, Wilczynski S, Monk B, Copeland LJ, Alvarez RD, Jiang C, Alberts D. Phase III randomized trial of 12 versus 3 months of maintenance paclitaxel in patients with advanced ovarian cancer after complete response to platinum and paclitaxel-based chemotherapy: a Southwest Oncology Group and Gynecologic Oncology Group trial. J Clin Oncol. 2003. 21:2460–2465.

3. McMeekin DS, Tillmanns T, Chaudry T, Gold M, Johnson G, Walker J, Mannel R. Timing isn't everything: an analysis of when to start salvage chemotherapy in ovarian cancer. Gynecol Oncol. 2004. 95:157–164.

4. Ozols RF. In : Perry MC, editor. Current controversies in ovarian cancer: maintenance chemotherapy and neoadjuvant chemotherapy as standard care. 2004 Educational Book. 2004. Spring. 40th Annual Meeting; June 5-8 2004; New Orleans, LA. Alexandria, VA: American Society of Clinical Oncology;268–275.
5. Eisenhauer EA, Vermorken JB, van Glabbeke M. Predictors of response to subsequent chemotherapy in platinum pretreated ovarian cancer: a multivariate analysis of 704 patients. Ann Oncol. 1997. 8:963–968.

7. Vergote I, Himmelmann A, Frankendal B, Scheistroen M, Vlachos K, Trope C. Hexamethylmelamine as second-line therapy in platin-resistant ovarian cancer. Gynecol Oncol. 1992. 47:282–286.

8. Rustin GJ, Nelstrop AE, Crawford M, Ledermann J, Lambert HE, Coleman R, Johnson J, Evans H, Brown S, Oster W. Phase II trial of oral altretamine for relapsed ovarian carcinoma: evaluation of defining response by serum CA125. J Clin Oncol. 1997. 15:172–176.

9. Manetta A, Tewari K, Podczaski ES. Hexamethylmelamine as a single second-line agent in ovarian cancer: follow-up report and review of the literature. Gynecol Oncol. 1997. 66:20–26.

10. Markman M, Blessing JA, Moore D, Ball H, Lentz SS. Altretamine (hexamethylmelamine) in platinum-resistant and platinum-refractory ovarian cancer: a Gynecologic Oncology Group phase II trial. Gynecol Oncol. 1998. 69:226–229.

11. Malik IA. Altretamine is an effective palliative therapy of patients with recurrent epithelial ovarian cancer. Jpn J Clin Oncol. 2001. 31:69–73.

12. Alberts DS, Jiang C, Liu PY, Wilczynski S, Markman M, Rothenberg ML. Long-term follow-up of a phase II trial of oral altretamine for consolidation of clinical complete remission in women with stage III epithelial ovarian cancer in the Southwest Oncology Group. Int J Gynecol Cancer. 2004. 14:224–228.

13. Mano MS, Awada A, Minisini A, Atalay G, Lago LD, Cardoso F, Piccart M. Remaining controversies in the upfront management of advanced ovarian cancer. Int J Gynecol Cancer. 2004. 14:707–720.

14. Gadducci A, Sartori E, Maggino T, Zola P, Landoni F, Fanucchi A, Palai N, Alessi C, Ferrero Am, Cosio S, Cristofani R. Analysis of failures after negative second-look in patients with advanced ovarian cancer: an Italian multicenter study. Gynecol Oncol. 1998. 68:150–155.

15. Thigpen JT. In : Perry MC, editor. Current controversies in ovarian cancer: maintenance chemotherapy as standard care. 2004 educational book. 2004. Spring. 40th Annual Meeting; June 5-8 2004; New Orleans, LA. Alexandria VA: American Society of Clinical Oncology;281–284.
16. Rothenberg ML, Liu PY, Wilczynski S, Hannigan EV, Weiner SA, Weiss GR, Hunter VJ, Chapman JA, Tiersten A, Kohler PC, Alberts DS. Phase II trial of oral altretamine for consolidation of clinical complete remission in women with stage III epithelial ovarian cancer: a Southwest Oncology Group trial (SWOG-9326). Gynecol Oncol. 2001. 82:317–322.

17. De Placido S, Scambia G, Di Vagno G, Naglieri E, Lombardi AV, Biamonte R, Marinaccio M, Carteni G, Manzione L, Febbraro A, De Matteis A, Gasparini G, Valerio MR, Danese S, Perrone F, Lauria R, De Laurentiis M, Greggi S, Gallo C, Pignata S. Topotecan compared with no therapy after response to surgery and carboplatin/paclitaxel in patients with ovarian cancer: Multicenter Italian Trials in Ovarian Cancer (MITO-1) randomized study. J Clin Oncol. 2004. 22:2635–2642.

18. Conte PF, Gadducci A, Cianci C. Second-line treatment and consolidation therapies in advanced ovarian cancer. Int J Gynecol Cancer. 2001. 11:Suppl 1. 52–56.

19. Ames MM. Hexamethylmelamine: pharmacology and mechanisms of action. Cancer Treat Rev. 1991. 18:Suppl A. 3–14.
20. Lee CR, Faulds D. Altretamine. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in cancer chemotherapy. Drugs. 1995. 49:932–953.
21. Bast RC Jr, Xu FJ, Yu YH, Barnhill S, Zhang Z, Mills GB. CA 125: the past and the future. Int J Biol Markers. 1998. 13:179–187.

22. Makar AP, Kristensen GB, Kaern J, Bormer OP, Abeler VM, Trope CG. Prognostic value of pre- and postoperative serum CA 125 levels in ovarian cancer: new aspects and multivariate analysis. Obstet Gynecol. 1992. 79:1002–1010.

23. Markman M, Federico M, Liu PY, Hannigan E, Alberts D. Significance of early changes in the serum CA-125 antigen level on overall survival in advanced ovarian cancer. Gynecol Oncol. 2006. 103:195–198.

24. Podratz KC, Malkasian GD Jr, Wieand HS, Cha SS, Lee RA, Stanhope CR, Williams TJ. Recurrent disease after negative second-look laparotomy in stages III and IV ovarian carcinoma. Gynecol Oncol. 1988. 29:274–282.

25. Chiara S, Lionetto R, Campora E, Oliva C, Merlini L, Bruzzi P, Rosso R, Conte PF. The Gruppo Oncologico Nord Ovest. Long-term prognosis following macroscopic complete response at second-look laparotomy in advanced ovarian cancer patients treated with platinum-based chemotherapy. Eur J Cancer. 1995. 31A:296–301.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download