Abstract
This study was undertaken to evaluate the incidence and risk factors associated with relative adrenal insufficiency (RAI) in Korean critically-ill patients. All patients who were admitted to the Medical Intensive Care Unit (MICU) of Samsung Medical Center between January 1, 2006 and April 30, 2007 were prospectively evaluated using a short corticotropin stimulation test on the day of admission. RAI was defined as an increase in the serum cortisol level of <9 µg/dL from the baseline after administration of 250 µg of corticotropin. In all, 123 patients were recruited and overall the incidence of RAI was 44% (54/123). The presence of septic shock (P=0.001), the Simplified Acute Physiology Score (SAPS) II (P=0.003), the Sequential Organ Failure Assessment (SOFA) score (P=0.001), the mean heart rate (P=0.040), lactate levels (P=0.001), arterial pH (P=0.047), treatment with vasopressors at ICU admission (P=0.004), and the 28-day mortality (P=0.041) were significantly different between patients with and without RAI. The multivariate analysis showed that the SOFA score was an independent predictor of RAI in critically-ill patients (odd ratio=1.235, P=0.032). Our data suggest that RAI is frequently found in Korean critically-ill patients and that a high SOFA score is an independent predictor of RAI in these patients.
Severe illness or infection activates the hypothalamic-pituitary-adrenal (HPA) axis (1-3); this activation is an essential component of the general adaptation to stress. However, the cortisol levels considered normal or above normal may not be sufficient in critically-ill patients (4). The presence of insufficient cortisol secretion, relative to illness severity, is referred to as relative adrenal insufficiency (RAI) or critical illnessrelated corticosteroid insufficiency (5).
There is increasing evidence that suggests that RAI occurs in critically-ill patients with sepsis, patients with human immunodeficiency virus infection, head injury, pancreatitis, burns, and following cardiac surgery (4, 6-9). However, the diagnosis of RAI in critically-ill patients is difficult because the expected cortisol levels vary with the type and severity of disease (4, 10), as well as with different serum levels of binding proteins (11). Increases in cortisol levels <9 µg/dL, after corticotropin stimulation, have been suggested to be the diagnostic criterion for adrenal insufficiency in critically-ill patients; these cortisol levels have been associated with vascular unresponsiveness to catecholamines (12, 13) and with an increased risk of death (4). However, the short corticotropin stimulation test takes time and requires three samples of blood, making it cumbersome to perform in the intensive care setting. If cortisol response to corticotropin stimulation can be predicted, it would be very helpful for clinicians at the bedside. However, currently there are no such variables that have been identified. Therefore, the aim of this study was to evaluate the incidence of RAI in critically-ill patients and to determine whether pretest clinical factors, including the disease severity index could be predictive of the cortisol response to the standard short corticotropin test.
All consecutive patients hospitalized and admitted to the Medical Intensive Care Unit (ICU) at Samsung Medical Center, in Seoul, Republic of Korea between January 2006 and April 2007 were prospectively enrolled in this study. Patients were excluded if they were in the ICU for cardiac monitoring or postoperative care, had been treated with any dose of corticosteroid previously, etomidate, estrogen, or any drug that could interfere with the HPA axis within the last 30 days, had known previous conditions that may have disrupted the HPA axis, were positive for the HIV antibody, were expected to improve promptly requiring less than 24 hr of ICU care, were pregnant, and had previously been admitted to the ICU during the same admission. The protocol was approved by our institutional review board and informed consent was obtained from the patients or patients' next of kin.
Within 24 hr of the ICU admission, the short corticotropin stimulation test was performed by administering 250 µg of synthetic corticotropin intravenously. Blood samples were taken immediately before the test and 30 and 60 min after the injection for measurement of the total cortisol by the enzyme-linked fluorescent assay. RAI was diagnosed when the peak cortisol concentration, after the corticotropin administration, was <9 µg/dL compared to the baseline.
At patient enrollment, the following parameters were recorded: time to rapid ACTH stimulation from ICU admission; age and gender; past medical history and underlying disease; the signs and symptoms of adrenal insufficiency at admission, which included presence of weakness, fatigue, anorexia, nausea, and vomiting; vital signs; the severity of illness, as assessed by the simplified acute physiology score (SAPS) II and the sequential organ failure assessment (SOFA) score. Laboratory measurements included arterial blood gas analysis, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, serum lactate, C-reactive protein, blood electrolytes, total blood cells, eosinophil and platelet counts, and serum levels of creatinine and albumin. In addition, the treatment given including vasopressors and mechanical ventilation were recorded. The duration of mechanical ventilation and the 28 day mortality were assessed.
Discrete variables are expressed as counts (percentage) and continuous variables as mean±standard deviation when they were normally distributed or in the median and interquartile range (25th and 75th percentiles) when they were not normally distributed. Chi-square analysis with the Fisher's exact test (when appropriate) was used to compare the categorical data. Continuous variables were analyzed with the Student's t-test and the Mann-Whitney U test as appropriate. The logistic regression model was used to identify significant variables predicting the odds ratio (OR) of RAI (along with the 95% confidence interval [CI]). Discrimination was assessed using the area under the receiver operating characteristic curve to evaluate how well the model distinguished patients who had RAI from those who did not. To perform survival analyses, continuous variables were discretized according to their medican value. The 28 day mortality was evaluated by the Kaplan-Meier method and compared with the log-rank test for all variables studied. A Cox regression model was used to assess variables related to the 28 day mortality. Statistical significance was established at P<0.05.
Among 419 admissions, 123 (29%) patients were recruited for the study. Two hundred nine (50%) patients were excluded because they were using or had used glucocorticoids within one month of the ICU admission. The reasons for glucocorticoid treatment were chemotherapy for malignant diseases in 122 (58%), chronic obstructive lung disease or asthma in 40 (19%), immunosuppressive treatment due to organ transplantation or rheumatologic diseases in 18 (9%), adrenal insufficiency in 12 (6%), and others in 17 (8%). Sixty (14%) patients were excluded because they were admitted for shortterm observation only, 20 (5%) patients or their families refused to give consent, and seven (2%) patients because 24 hr had already elapsed before the short corticotropin test could be given.
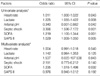
Of the 123 patients, 55 were female and 68 were male. The mean age of the patients was 57±16 yr. At ICU admission, 52% of all patients had septic shock and 72% had severe sepsis. The mean SAPS II and SOFA scores were 49.1±19.9 and 9.4±4.4, respectively. In all, 54 (44%) patients were diagnosed with RAI. The short corticotropin stimulation test was performed at a median of 8 hr (IQR 3-16 hr) after the ICU admission. Table 1 shows the main patient characteristics and results of the univariate analysis of the patients with RAI compared to those without RAI. Septic shock (P=0.001), the mean SAPS II score (P=0.003), the SOFA score (P=0.001), the mean heart rate (P=0.040), lactate levels (P=0.001), the arterial pH (P=0.047), treatment with vasopressors at ICU admission (P=0.004), and the 28-day mortality (P=0.041) were significantly different between the patients with and without RAI. Among subcategories of SOFA score, platelet (1.67±1.47 in RAI vs. 0.93±1.27, P=0.004), liver (1.37±1.34 in RAI vs. 0.57±0.96, P>0.001), cardiovascular (2.98±1.58 in RAI vs. 1.93±1.84, P=0.001), and renal (1.5±1.48 in RAI vs. 0.80±1.28, P=0.006). SOFA scores were significantly higher in patients with RAI compared to those without RAI.
All variables found to be significantly different between the patients with RAI and those without RAI, according to the univariate analysis performed on patient characteristics at ICU admission (apart from physician's interventions, namely the administration of vasopressors), were entered into the logistic regression model. Among those variables, the SOFA score was the only independent predictive factor of RAI in critically ill patients (OR, 1.235, 95% CI, 1.018-1.498, P=0.032) (Table 2). To evaluate the potential to predict RAI in the critically-ill patients, a receiver operating characteristic (ROC) analysis was performed. The SOFA score had an area under the ROC curve of 0.717 (95% CI, 0.623-0.811) and with an optimal calculated SOFA score threshold of 9.5, the sensitivity and specificity were 61% and 67%, respectively (Fig. 1).
In the univariate analysis, factors predicting the 28 day mortality were a SOFA >10 (P<0.001), the SAPS II >50 (P=0.002), and a lactate >2.3 mM/L (P<0.045). Among those variables, the SOFA score was the only independent predictive factor of the 28 day mortality in the Cox proportional hazards model (OR, 8.1, 95% CI, 1.0-63.9, P=0.046).
Our findings suggest that RAI, diagnosed by a decreased cortisol response to corticotropin, is frequently observed in Korean critically-ill patients and that the SOFA score was an independent predictive factor for RAI.
The optimal way to diagnose RAI in critically ill patients remains controversial. The simplest method is to test a random cortisol level. In an otherwise stable person, a random serum cortisol level ≤3 µg/dL is suggestive of adrenal insufficiency, whereas the presence of adrenal insufficiency may be ruled out with a random cortisol level ≥19 µg/dL (14). However, in critically-ill patients, the basal serum cortisol levels are usually elevated and correlate with the severity of the illness (4), which makes determining the appropriate cortisol response difficult. Prior studies of RAI have used different levels of cortisol to diagnose RAI; currently there is no universally accepted level (15).
In this study, we defined RAI in critically-ill patients as an increase in cortisol levels <9 µg/dL, compared to the baseline, after corticotropin infusion. This level has been associated with increased mortality and is the most widely accepted criterion used for RAI (4, 16); however, the utility of RAI diagnosed by this criterion continues to be debated. In contrast to an earlier report of improved survival after corticosteroid replacement therapy (16), a recent large scale randomized study failed to demonstrate improved survival in patients with septic shock after corticosteroid therapy (17).
In a study recently published by Annane et al. (18), the investigators compared the cortisol response to corticotropin with the metyrapone test, which assesses the entire HPA axis, and suggested a new criterion for RAI (basal cortisol <10 µg/dL or an increase in cortisol levels ≤9 µg/dL from baseline). However, the metyrapone test has its own limitations. It requires intact gastrointestinal absorption of the drug, which in critically-ill patients is not always present (14), and it is influenced by P450 enzyme inducers such as rifampin or phenobarbital (14, 19). In addition, there is no data available on the clinical significance of RAI diagnosed with these criteria using clinically important endpoints.
Although the incidence of RAI in critically ill patients varied widely depending on the population being studied and the diagnostic criteria used, it is well established that RAI is frequently observed in patients with septic shock. In this study, the incidence of RAI in patients with septic shock was 58%; this was slightly lower than the reports of Annane et al. (77%) (16), and a previous study reported by our group (71%) (20). However, at present, little data is available in the literature on the incidence of impaired adrenal function in patients without septic shock. In this study, we found that a similar proportion of patients admitted to the MICU had RAI whether they had septic shock (29%), severe sepsis (31%) or other conditions (31%).
This study is the first prospective study reporting the incidence of RAI in Korean critically-ill patients. RAI in critically-ill patients, in an Asian population, has not been well studied. It is not known whether there are interracial differences in the incidence of RAI. In one study conducted in China, which used the same diagnostic criteria of RAI as our study, the incidence of RAI in patients with severe sepsis was 38.3%, and was higher in non-survivors (62.3%) compared to survivors (19.4%) (21).
The only independent factor predicting RAI was the SOFA score. This could be important because there is no specific clinical feature proven to be helpful in predicting RAI in critically-ill patients (22, 23). Although symptoms such as fatigue, weight loss, nausea, abdominal pain, arthralgia, and postural syncope are known to be associated with hypoadrenalism, these are nonspecific findings and frequently found in critically ill patients (24). Similarly, the classic features of an Addisonian crisis, such as anorexia, nausea, vomiting, diarrhea, delirium, fever, and hypotension, are common in septic patients (24). Thus, it is extremely difficult to identify adrenal insufficiency in patients requiring intensive care.
One recent study showed that the SOFA score and other laboratory data such as a low pH/bicarbonate and platelet count were independent predictors of relative adrenal insufficiency in critically-ill patients (25). However, that study was a retrospective study and included patients who were receiving glucocorticoids, antifungal agents and etomidate, which can interfere with the HPA axis. In addition, the short corticotropin stimulation test was performed only in patients with suspicious symptoms or signs of adrenal insufficiency. In our study, we prospectively enrolled all patients, excluding patients using drugs that could influence the HPA axis.
The present study has several limitations. First, we measured the total cortisol not the free cortisol. Free cortisol is thought to be more representative of the physiologic actions of cortisol because of the common findings of hypoalbuminemia in the critically-ill (11). However, a recent study conducted by Annane et al. (18) showed that free cortisol was not superior to total cortisol in diagnosing RAI in the critically-ill. Second, only 29% of all eligible patients were recruited limiting the generalization of our findings. This was mainly because half of all of the patients admitted to the medical ICU were receiving or had recently received steroid treatment at ICU admission. Third, not all of the patients with RAI received treatment with corticosteroid replacement therapy, as the decision to administer such treatment was made by the attending physician. Only 19 (35%) patients with RAI received low-dose corticosteroid replacement therapy (hydrocortisone sodium succinate 50 mg every 6 hr for 7 days). No significant difference in mortality was observed between patients who received corticosteroid replacement therapy and those who did not (26% [5/19] vs. 37% [13/22], P=0.550). Whether corticosteroid replacement therapy improves in patients with RAI should be further studied.
In conclusion, the results of this study show that adrenal insufficiency is frequently found in Korean critically-ill patients. In addition, a high SOFA score is an independent risk factor for RAI in these patients.
Figures and Tables
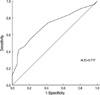 | Fig. 1Receiver operator curve (ROC) analysis of Sepsis-Related Organ Failure scores predicting adrenal insufficiency in critically-ill patients.
AUC, area under the ROC curve.
|
Table 1
The patient characteristics according to the presence of adrenal insufficiency

Values are expressed as the mean±SD or median (first quartile-third quartile) or number (%).
*Chi-square test was performed; †Student's t-test was performed; ‡Mann-Whitney U test was performed.
RAI, relative adrenal insufficiency; ACTH, adrenocorticotropic hormone; ARDS, acute respiratory distress syndrome; F, emale; M, male; SAPS, Simplified Acute Physiology Score; SOFA, Sepsis-Related Organ Failure Assessment; ICU, intensive care unit.
References
1. Schein RM, Sprung CL, Marcial E, Napolitano L, Chernow B. Plasma cortisol levels in patients with septic shock. Crit Care Med. 1990. 18:259–263.

2. Drucker D, McLaughlin J. Adrenocortical dysfunction in acute medical illness. Crit Care Med. 1986. 14:789–791.

3. Drucker D, Shandling M. Variable adrenocortical function in acute medical illness. Crit Care Med. 1985. 13:477–479.

4. Annane D, Sebille V, Troche G, Raphael JC, Gajdos P, Bellissant E. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA. 2000. 283:1038–1045.

5. Marik PE. Mechanisms and clinical consequences of critical illness associated adrenal insufficiency. Curr Opin Crit Care. 2007. 13:363–369.

6. Dimopoulou I, Tsagarakis S, Kouyialis AT, Roussou P, Assithianakis G, Christoforaki M, Ilias I, Sakas DE, Thalassinos N, Roussos C. Hypothalamic-pituitary-adrenal axis dysfunction in critically ill patients with traumatic brain injury: incidence, pathophysiology, and relationship to vasopressor dependence and peripheral interleukin-6 levels. Crit Care Med. 2004. 32:404–408.

7. Kilger E, Weis F, Briegel J, Frey L, Goetz AE, Reuter D, Nagy A, Schuetz A, Lamm P, Knoll A, Peter K. Stress doses of hydrocortisone reduce severe systemic inflammatory response syndrome and improve early outcome in a risk group of patients after cardiac surgery. Crit Care Med. 2003. 31:1068–1074.

8. Marik PE, Kiminyo K, Zaloga GP. Adrenal insufficiency in critically ill patients with human immunodeficiency virus. Crit Care Med. 2002. 30:1267–1273.

9. Sheridan RL, Ryan CM, Tompkins RG. Acute adrenal insufficiency in the burn intensive care unit. Burns. 1993. 19:63–66.

10. Sibbald WJ, Short A, Cohen MP, Wilson RF. Variations in adrenocortical responsiveness during severe bacterial infections. Unrecognized adrenocortical insufficiency in severe bacterial infections. Ann Surg. 1977. 186:29–33.
11. Hamrahian AH, Oseni TS, Arafah BM. Measurements of serum free cortisol in critically ill patients. N Engl J Med. 2004. 350:1629–1638.

12. Annane D, Bellissant E, Sebille V, Lesieur O, Mathieu B, Raphael JC, Gajdos P. Impaired pressor sensitivity to noradrenaline in septic shock patients with and without impaired adrenal function reserve. Br J Clin Pharmacol. 1998. 46:589–597.

13. Hoen S, Asehnoune K, Brailly-Tabard S, Mazoit JX, Benhamou D, Moine P, Edouard AR. Cortisol response to corticotropin stimulation in trauma patients: influence of hemorrhagic shock. Anesthesiology. 2002. 97:807–813.
14. Grinspoon SK, Biller BM. Clinical review 62: laboratory assessment of adrenal insufficiency. J Clin Endocrinol Metab. 1994. 79:923–931.

15. Beishuizen A, Thijs LG. Relative adrenal failure in intensive care: an identifiable problem requiring treatment? Best Pract Res Clin Endocrinol Metab. 2001. 15:513–531.

16. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, Chaumet-Riffaut P, Bellissant E. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002. 288:862–871.

17. Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka A, Forst H, Laterre PF, Reinhart K, Cuthbertson BH, Payen D, Briegel J. Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008. 358:111–124.

18. Annane D, Maxime V, Ibrahim F, Alvarez JC, Abe E, Boudou P. Diagnosis of adrenal insufficiency in severe sepsis and septic shock. Am J Resp Crit Care Med. 2006. 174:1319–1326.

19. Meikle AW, Jubiz W, Matsukura S, West CD, Tyler FH. Effect of diphenylhydantoin on the metabolism of metyrapone and release of ACTH in man. J Clin Endocrinol Metab. 1969. 29:1553–1558.

20. Kwon YS, Suh GY, Kang EH, Koh WJ, Chung MP, Kim H, Kwon OJ. Basal serum cortisol levels are not predictive of response to corticotropin but have prognostic significance in patients with septic shock. J Korean Med Sci. 2007. 22:470–475.

21. Yang Y, Liu L, Zhao B, Li MQ, Wu B, Yan Z, Gu Q, Sun H, Qiu HB. Relationship between adrenal function and prognosis in patients with severe sepsis. Chin Med J (Engl). 2007. 120:1578–1582.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download