Abstract
Posterior cervical foraminotomy is an effective surgical technique for the treatment of radicular pain caused by foraminal stenosis or posterolateral herniated discs. The present study was performed to compare the clinical parameters and surgical outcomes of open foraminotomy/discectomy (OF/OFD) and tubular retractor assisted foraminotomy/discectomy (TAF/TAFD) in the treatment of cervical radiculopathy. A total of 41 patients were divided into two groups: 19 patients in Group 1 underwent OF/OFD and 22 patients in Group 2 underwent TAF/TAFD. Among the various clinical parameters, skin incision size, length of hospital stay, analgesic using time, and postoperative neck pain (for the first 4 weeks after the operation) were favorable in Group 2. Surgical outcomes were not different between the two groups. In conclusion, TAF/TAFD should increase patient's compliance and is as clinically effective as much as the OF/OFD.
Posterior cervical foraminotomy is an effective surgical technique for the treatment of radicular pain arising from compression in the foramen secondary to bony stenosis or soft disc herniation (1-3). In 1943, Semmes and Murphey first described cervical radicular root syndromes (4), and Murphey followed up with a description of 648 cases in 1973 (5).
Various surgical techniques can be used for the treatment of cervical radiculopathy. Although anterior cervical procedures have gained prominence, posterior cervical foraminotomy has proven benefits. It has been found to relieve symptoms in 82% to 97% of patients who have radiculopathy caused by foraminal stenosis or posterolateral herniated discs (1, 3, 6-9). Moreover, a posterior procedure avoids the complications associated with anterior approaches to the cervical spine, particularly vascular injury, esophageal injury, dyspnea, recurrent laryngeal nerve injury, dysphagia, and the accelerated degeneration of adjacent motion segments after fusion, known as adjacent segment disease (10-12). However, postoperative neck pain and spasm are disadvantages of a posterior procedure. A wider incision and an extensive periosteal muscle dissection for adequate visualization can induce neck discomfort, which can result in a slower recovery. Minimally invasive spine surgery is necessary to meet the demands of modern society for faster recoveries, which allow patients to resume their normal activities as soon as possible.
Currently, among the various minimally invasive spinal surgery techniques, the tubular retractor system is a well developed system that enables posterior cervical foraminotomy and discectomy through a tubular retractor under microscopic visualization. The present study was performed to compare the clinical parameters and surgical outcomes between open foraminotomy/discectomy (OF/OFD) and tubular retractor assisted foraminotomy/discectomy (TAF/TAFD) in the treatment of cervical radiculopathy.
A total of 41 patients with radiating pain in the upper arm caused by foraminal stenosis or cervical posterolateral disc herniation were enrolled in the study from January 2003 to June 2005. They were randomly assigned to have surgical treatment by either OF/OFD or TAF/TAFD. Inclusion criteria were the presence of a foraminal stenosis or a posterolateral disc herniation on magnetic resonance imaging (MRI) and persistent radiating pain in the upper arm after 6 weeks of conservative treatment. Patients were excluded if they had neoplasm, traumatic injury, myelopathy, or recurrent cervical disc disease.
After the inclusion criteria were met and informed consent was obtained, patients were randomly allocated into one of two groups based on the surgical technique: Group 1 underwent OF/OFD (19 patients); and Group 2 underwent TAF/TAFD (22 patients). All of these operations were performed by the same spinal neurosurgeon.
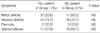
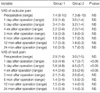
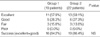
The preoperative and postoperative evaluation consisted of a radiologic finding, a neurological examination, and a pain scoring for the upper arm and neck using a Visual analogue scale (VAS). Postoperative evaluations were done on days 1 and 5, week 4, and months 3, 6, 12, and 24 after the operation. The clinical outcomes were evaluated using modified Odom et al. criteria (13) (Table 1). All patients underwent a preoperative MRI as well as preoperative and postoperative computed tomography (CT) scans. The postoperative CT scan was done on 5 days after the operation. We calculated the vertical and transverse diameters of the foraminotomy using the postoperative CT scan (Fig. 1).
All patients were operated on in a prone position. A radiolucent three pin-head fixed instrument was used. A vertical 3 cm midline incision was made after determining the correct level on a lateral radiograph. The lateral lamina/medial facet joints were exposed. Under a surgical microscope, a partial hemilaminectomy and foraminotomy with partial facetectomy of the target level was performed using high-speed drills. The extent of the facet resection was based on the extent of the foraminal pathology on that half of the facet joint. In cases of pure disc herniation, the proximal root was adequately visualized in order to remove the compressing disc material. However, in cases of foraminal stenosis, bony decompression and skeletonization of the proximal root were carefully performed using a 2-mm bullet burr, cervical curette and punch. Patients wore a soft collar for 2-4 weeks after the operation, and were given adequate medication.
The technique used for TAF or TAFD was similar to that used for OF or OFD. Although the procedures use a tubular retractor (METRx system, Medtronic Sofamor Danek, Memphis, TN, U.S.A.), the principles are the same regardless of the specific type of retractor system that was used. A skin incision was initially made approximately 5 mm off the midline ipsilateral to and at the target level. For two-level procedures, the incision should be placed midway between the target levels. After an initial skin incision, the K-wire is slowly advanced through the musculature. This is done under continuous fluoroscopic guidance in order to avoid malposition of the K-wire. The K-wire is docked on bone at the inferomedial edge of the rostral lateral mass at the target level (Fig. 2). At this point, the skin incision was extended above and below the K-wire entry point for a total length of approximately 2 cm and the wire is removed. The cervical fascia is incised equal to the length of the skin incision using monopolar cautery. The tubular muscle dilators are placed serially. After dilation is complete, a final working channel (16-mm or 18-mm tubular retractor) is placed over the dilators and fixed over the laminofacet junction with a table-mounted flexible retractor arm, and the dilators are removed. The additional skin incision can be needed in order to avoid skin necrosis, if the final working channel is tightly packed the skin incision. Under the surgical microscope, a partial hemilaminectomy and foraminotomy with partial facetectomy of the target level was performed using high-speed drills. Although the techniques of foraminotomy and discectomy were the same as those for OF/OFD, the tubular retractor assisted procedure needs a more detailed review of preoperative radiological findings in order to achieve adequate neural decompression.
All patients received the same postoperative pain management medication, which included talniflumate (1,110 mg/day) and afloqualone (60 mg/day) as the postoperative analgesic and muscle relaxant, respectively. These medications were discontinued if both VAS scores for radicular and neck pain were less than 3. Patient-controlled analgesia was used for the first 2 days after the operation.
The SPSS 12.0 statistical software package (SPSS, Inc., Chicago, IL, U.S.A.) was used for statistical analysis. Data were analyzed using the chi-square, Fisher exact, Student's t, and Mann-Whitney tests, as appropriate. A P value of <0.05 was considered to be statistically significant.
A total of 41 patients were divided into two groups: 19 patients in Group 1 underwent OF/OFD and 22 patients in Group 2 underwent TAF/TAFD (Table 2). The mean follow-up period was 34.2 months in Group 1 (range, 24-66 months) and 33.1 months in Group 2 (range, 24-64 months). The clinical parameters (age, sex, duration of symptoms, surgical time, skin incision size, length of hospital stay, analgesic using time, number and location of affected lesion, diagnosis and foraminotomy defect diameter) are shown in Table 2. The skin incision size, length of hospital stay and analgesic using time were significantly shorter in Group 2 compared to Group 1 (P<0.05).
Five patients (12.2%) experiended only pain as a presenting symptom. All other patients had an additional motor and/or sensory deficit prior to the operation. The preoperative neurological status of the patients is shown in Table 3 and there were no differences in neurological status between the two groups.
The pain evaluations were done using the VAS. We used the VAS score to check for radicular pain and neck pain on days 1 and 5, week 4, and months 3, 6, 12, and 24 after the operation (Table 4). The degree of radicular pain did not differ between the two groups. However, the degree of neck pain was different. VAS scores for neck pain from day 1 to week 4 after the operation were more severe in Group 1 than in Group 2.
The total success rate was 85.4% using modified Odom's criteria. Each surgical outcome is shown in Table 5. There were no differences in surgical outcomes between the two groups, and there were no reported complications due to the surgeries.
Various mechanical causes, such as disc herniation, bony spur and foraminal stenosis, can induce radiculopathy. There are various surgical techniques to treat radiculopathy (1, 3, 5, 7, 14, 15). The effectiveness of posterior foraminotomy/discectomy for treating foraminal stenosis and posterolateral disc herniation is well established in the literature (1, 16-19).
The advantages of posterior foraminotomy/discectomy include the avoidance of complications associated with anterior approaches to the cervical spine and no need for cervical fusion and instrumentation. However, posterior procedures also have some problems, such as a limitation in surgical indication (e.g., central disc herniation) and postoperative neck discomfort. A wider incision and an extensive periosteal muscle dissection for adequate visualization can induce neck pain, which can result in a slower recovery. Modern society demands faster recovery times, which necessitates minimally invasive spine surgery. Foley and Smith (20) first described the tubular retractor assisted endoscopic discectomy for lumbar disc herniation in 1997. They believed that this procedure is a less invasive and more effective technique for treating lumbar stenosis and disc herniation. This concept has since been adapted to treatments of the cervical spine.
In this study, we compared the various clinical parameters of TAF/TAFD and OF/OFD (Table 2). The skin incision size, length of hospital stay, and analgesic using time were significantly shorter in Group 2 than in Group 1 (P<0.05). In addition, the postoperative neck pain reported during the 4 weeks after the operation was significantly lower in Group 2. These results show the advantages of TAF/TAFD. TAF/TAFD is a minimally invasive procedure using a tubular retractor system, which allows for a smaller skin incision and far less muscle injury (21). It also reduces the amount of postoperative discomfort and shortens the length of hospital stays and the postoperative analgesic using time.
Our surgical outcomes for the two groups were not statistically different. Fessler et al. described the use of the tubular retractor assisted endoscopic system for posterior cervical laminoforaminotomy in human cadaveric spines in 2000 (10). They demonstrated that the average vertical and transverse diameters of the foraminotomy defect were greater in the TAF group compared to the OF group. In our study, the average vertical and transverse diameters of the foraminotomy defect were the same in the two groups. These results suggest that the TAF is at least as clinically effective as the OF in relieving the neural compression and thereby reducing radicular symptoms. Our total success rate was 85.4% using modified Odom's criteria. This outcome is similar to the success rates (82-97%) reported in other studies (1, 3, 6-9).
The complication rate in other studies was 0-9%. Durotomy and CSF leak were the most commonly reported complications (5, 6, 8, 9, 13, 18). Although we did not experience complications after the posterior procedure, our study had a small number of patients and more complications may arise in a large study group. However, it is clear that the cervical posterior procedures (TAF/TAFD and OF/OFD) can be safely performed in patients with foraminal stenosis and posterlateral disc herniation.
The superiority of TAF/TAFD over OF/OFD has been demonstrated in some studies (10, 19), but until now, there has not been a randomized clinical study comparing TAF/TAFD and OF/OFD. To our knowledge, this is the first prospective randomized clinical study comparing the clinical outcomes of these techniques.
Some parameters (skin incision size, length of hospital stay, analgesic using time, and postoperative neck pain during the first four postoperative weeks) were favorable in Group 2 and these factors should affect the willingness of a patient to undergo this operation. In conclusion, TAF/TAFD should increase patient's compliance and is as clinically effective as OF/OFD.
Figures and Tables
Fig. 1
Postoperative CT shows the foramintomy defect. (A) Transverse diameter (B) Vertical diameter.

Fig. 2
The K-wire is advanced slowly through the musculature under fluoroscopic guidance and docked on bone at the inferomedial edge of the rostral lateral mass at the target level.

References
1. Henderson CM, Hennessy RG, Shuey HM Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. 1983. 13:504–512.

2. Caglar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, Ugur HC. Keyhole approach for posterior cervical discectomy: experience on 84 patients. Minim Invasive Neurosurg. 2007. 50:7–11.

3. Ducker TB, Zeidman SM. The posterior operative approach for cervical radiculopathy. Neurosurg Clin N Am. 1993. 4:61–74.

4. Semmes RE, Murphey F. Syndrome of unilateral rupture of the sixth, cervical intervertebral disk, with compression of the seventh cervical nerve root. Report of four cases with symptoms simulating coronary disease. JAMA. 1943. 121:1209–1214.
5. Murphey F, Simmons JC, Brunson B. Surgical treatment of laterally ruptured cervical disc. Review of 648 cases, 1939 to 1972. J Neurosurg. 1973. 38:679–683.
6. Aldrich F. Posterolateral microdisec tomy for cervical monoradiculopathy caused by posterolateral soft cervical disc sequestration. J Neurosurg. 1990. 72:370–377.
7. Korinth MC, Kruger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine. 2006. 31:1207–1214.

8. Jodicke A, Daentzer D, Kastner S, Asamoto S, Boker DK. Risk factors for outcome and complications of dorsal foraminotomy in cervical disc herniation. Surg Neurol. 2003. 60:124–129.
9. Onimus M, Destrumelle N, Gangloff S. Surgical treatment of cervical disk displacement. Anterior or posterior approach? Rev Chir Orthop Reparatrice Appar Mot. 1995. 81:296–301.
10. Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery. 2002. 51:S37–S45.

11. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004. 4:190S–194S.

12. Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004. 4:624–628.

14. Roh SW, Kim DH, Cardoso AC, Fessler RG. Endoscopic foraminotomy using MED system in cadaveric specimens. Spine. 2000. 25:260–264.

15. O'Toole JE, Sheikh H, Eichholz KM, Fessler RG, Perez-Cruet MJ. Endoscopic posterior cervical foraminotomy and discectomy. Neurosurg Clin N Am. 2006. 17:411–422.
16. Zeidman SM, Ducker TB. Posterior cervical laminoforaminotomy for radiculopathy: review of 172 cases. Neurosurgery. 1993. 33:356–362.
17. Krupp W, Schattke H, Muke R. Clinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniation. Acta Neurochir (Wien). 1990. 107:22–29.

19. Gala VC, O'Toole JE, Voyadzis JM, Fessler RG. Posterior minimally invasive approaches for the cervical spine. Orthop Clin N Am. 2007. 38:339–349.

20. Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997. 3:301–307.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download