Abstract
The goal of this study was to evaluate the prevalence of first-line anti-tuberculosis drug resistance and risk factors associated with multidrug-resistant tuberculosis (MDR TB) among young soldiers in the Korean military, which has a strict tuberculosis control program. All patients with culture-confirmed pulmonary tuberculosis during their service at the Armed Forces Capital Hospital from January 2001 to December 2006 were enrolled in the study. Drug resistant Mycobacterium tuberculosis was isolated from 18 patients (12.2%) and multidrug-resistant M. tuberculosis was isolated from 12 patients (8.1%). Previous treatment of tuberculosis and the presence of a cavity on the patient's chest computed tomography scan were associated with MDR TB; military rank, smoking habits, and positive acid-fast bacilli smears were not associated with MDR TB. In a multiple logistic regression analysis, previous treatment of tuberculosis was a significant independent risk factor for MDR TB (odds ratio 6.12, 95% confidence interval 1.53-24.46). The prevalence of drug resistant tuberculosis among young soldiers in the Korean military was moderately high and the majority of resistant cases were found in patients who had undergone previous treatment of tuberculosis. Based on our results, we suggest that relapsed tuberculosis cases within communal settings should be cautiously managed until the drug susceptibility tests report is completed, even if previous treatment results were satisfactory.
Pulmonary tuberculosis remains a major public health problem and economic burden worldwide. Despite advances in chemotherapy policies, the prevalence of tuberculosis is still high. Resistance to anti-tuberculosis drugs is an increasing problem in many parts of the world. Therefore, quantifying drug-resistance rates and identifying potential risk factors are critical for controlling drug-resistant strains (1).
In the Republic of Korea, which has an intermediate burden of tuberculosis (2), military service is compulsory for all young men. Military personnel are at risk for tuberculosis due to crowded living conditions and the specific age groups involved (3, 4). In the Korean military, the incidence of pulmonary tuberculosis has been declining steadily; however it is still high (5). In response, the Korean military has implemented a strict tuberculosis control program, which includes the followings. At the time of enlistment, tuberculosis patients who have undergone treatment for less than six months are deferred; and military service is rejected for patients with a history of tuberculosis resistance to isoniazid (INH) or rifampicin (RFP), or for those who have had a positive culture after three months of treatment. Following a physical examination during conscription, chest radiograph screening is performed on all recruits and further evaluations are carried out if there are any suspicious active lesion. During military service, diagnosis and treatment of pulmonary tuberculosis is performed according to the recommended guidelines of both the National Tuberculosis Program and the Korean Academy of Tuberculosis and Respiratory Disease (6). This includes isolation of the patient from military units and undertaking directly observed therapy for at least two weeks.
Despite these efforts, tuberculosis outbreaks are still reported in the Korean military (7). Furthermore, because drug susceptibility tests can only be confirmed two months after diagnosis (8), multidrug-resistant tuberculosis (MDR TB) outbreaks are a major concern when the index case lives and works in a crowded unit. In this type of situation, it is important to know the current status of all individuals and to identify personnel that have a high probability of contracting MDR TB, prior to the arrival of report of drug susceptibility test. However, no data are available regarding the drug resistance rates and risk factors associated with MDR TB among young soldiers in a communal setting. Here, we evaluated the prevalence of first-line drug resistant tuberculosis and risk factors associated with MDR TB in young Korean soldiers.
All patients enrolled in the study were diagnosed with pulmonary tuberculosis by positive culture at the Armed Forces Capital Hospital between January 2001 and December 2006. Patients referred from other military hospitals, patients without drug susceptibility test reports, and sergeants (higher rank than staff sergeant) and officers who did not live in communal settings were excluded from the study. The Armed Forces Capital Hospital (a referral military hospital) is responsible for maintaining the health of soldiers who work in the area adjacent to Seoul, the capital city of the Republic of Korea. Military populations occupying ranks lower than sergeant or officer reside in the first-assigned area throughout their military service. Therefore, our study population appears to be a representative sample of all young soldiers at risk for pulmonary tuberculosis that are stationed in the area adjacent to Seoul.
We retrospectively reviewed medical records, laboratory data, radiological findings, and personal detailed reports of all enrolled patients. In addition, we obtained sputum acidfast bacilli (AFB) smear results, smoking histories, previous treatment history for tuberculosis (>1 month), and military rank at diagnosis. Because ranks of soldiers performing compulsory military service are promoted at regular intervals of 6 months (with rare exceptions), military rank reflects the time from enlistment to diagnosis.
Clinical specimens were stained using the Ziehl-Neelsen method (9). Microscopy results for sputum smears were reported semi-quantitatively; a positive smear was defined as >1 AFB per 100 in a field under high-power (9). Clinical specimens were cultured on 3% Ogawa medium. Mycobacterium tuberculosis was confirmed in cultures using measurements of growth rate, colony morphology, and pigmentation. Additionally, commercial biochemical tests were performed (BLL Taxo TB niacin test; BD Diagnostics, Franklin Lakes, NJ, U.S.A.). All isolates of M. tuberculosis were referred to the Korean Institute of Tuberculosis for drugs usceptibility test. Drug resistance was determined by the absolute concentration method. Briefly, Lowenstein-Jensen medium containing anti-tuberculosis drugs were used at the following critical concentrations: INH 0.2 µg/mL; RMP 40 µg/mL; ethambutol (EMB) 2.0 µg/mL (10). Pyrazinamide (PZA) susceptibility was determined using the pyrazinamidase test (11).
Data are presented as the percentage and absolute frequency for categorical variables and the median and range for continuous variables. We compared the clinical and radiological findings between patients with MDR TB and those with non-MDR TB. Frequencies were analyzed using either a chi-square test or Fisher's exact test, where appropriate. A multiple logistic regression analysis was used to identify independent risk factors associated with MDR TB. The development of MDR TB was the dependent variable and all clinical and radiological findings were the independent variables in the forward stepwise multiple logistic regression model. All data were analyzed by using SPSS 13.0. (SPSS Inc, Chicago, IL, U.S.A.).
A total of 198 patients were diagnosed with culture-confirmed pulmonary tuberculosis at the Armed Forces Capital Hospital between January 2001 and December 2006. Of these, 24 patients, consisted of 20 sergeants, two officers, and four individuals without drug susceptibility test reports, were excluded because they were referred from other military hospitals. Therefore, the total number of patients enrolled in the study was 148. The median age was 21 yr (range: 20-22 yr) and all patients were male. Sixty-five patients (43.9%) were current smokers. AFB sputum smears were positive in 90 patients (60.8%). One hundred-nineteen patients (80.4%) were new cases, and 29 (19.6%) had a history of previous treatment of tuberculosis; 23 (79.3%) had completed treatment with confirmation of cure, but six (20.7%) had not been confirmed the cure after treatment for more than 6 months. Median length of time from completion of previous treatment prior to diagnosis is two years (6 months-7 yr). Chest computerized tomography (CT) scans were performed on all enrolled patients; and 63 patients (42.6%) showed the presence of a cavity on the chest CT.
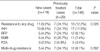
M. tuberculosis, that was resistant to at least one drug, was isolated from 18 patients (12.2%; Table 1). Drug resistance rates were higher in previously treated cases (24.1%) compared to new cases (9.2%, P=0.028; Table 1). Multidrugresistant M. tuberculosis was isolated from 12 patients (8.1%). The rate of MDR TB was also higher in previously treated cases (24.1%) compared to new cases (4.2%, P=0.002; Table 1).
There was no relationship between the development of MDR TB and military rank (P=0.225, test for trends; Fig. 1). In addition, no significant differences were observed in terms of smoking history or sputum smear results between groups (P=0.658 and 0.367, respectively; Table 2). Patients with MDR TB were more likely to have received previous treatment of tuberculosis compared to patients with non-MDR TB (58.3% vs. 16.2%, P=0.002; Table 2). In addition, patients with MDR TB were more likely to have exhibited a cavity on the chest CT (75.0%) compared to patients with non-MDR TB (39.7%, P=0.018; Table 2). In the multiple logistic regression analysis, previous treatment of tuberculosis was a significant independent risk factor for MDR TB (odds ratio 6.12, 95% confidence interval 1.53-24.46). However, military rank, smoking, positive AFB smear and cavity on chest CT were not associated with development of MDR TB (Table 2).
In this study, we evaluated the prevalence of drug resistant tuberculosis and identified risk factors associated with MDR TB in individuals in the Korean military. The proportion of MDR TB was 8.1%; and previous treatment of tuberculosis was the only significant independent risk factor for MDR TB among young Korean soldiers with culture-confirmed pulmonary tuberculosis.
In a recent drug resistance survey among Korean patients in their twenties, drug resistance rates are 14.3% for new cases and 22.5% for previously treated cases, respectively (10). These proportions are similar to those found in our study. However, this result is somewhat difficult to accept when considering that a well-organized tuberculosis control program should reduce drug resistant tuberculosis (12, 13), and when Korean military has a stricter control program than the private sector. However, communal living and intense physical training in military life may diminish the effectiveness of this strict control program. Other studies have reported that imprisonment is associated with drug resistant tuberculosis (14).
Previous treatment of tuberculosis has been consistently reported as the risk factor within various clinical conditions and populations (14-20). We found that previous treatment of tuberculosis was strongly associated with MDR TB in Korean military personnels. It is intriguing given that any person who has history of MDR TB, a poor treatment outcome, incomplete treatment for tuberculosis, or suspicious active lesion of tuberculosis on chest radiograph screening was excluded from enlistment. These results suggest that previous treatment can be a risk factor for drug resistance even if the treatment had a favorable course and if the patient had been clinically cured. Chest cavities are also associated with MDR TB in some reports (15, 17, 20). However, in almost all previous studies, cavities were confirmed only by chest radiograph, and some cavities may have been missed. To minimize this possibility, chest CT scans were performed on all patients in our study. We found that the presence of a cavity was associated with MDR TB; however, this result was not significant in a multivariate analysis.
This study has several limitations. First, this study was performed in a central referral military hospital where the most severe cases are treated. We cannot exclude the possibility that particularly severe or complicated cases were inadvertently included in this study. However, we excluded patients referred from other military hospitals to avoid this selection bias. Second, some parts of the patients' medical history at conscription depend on the soldier's memory. We attempted to obtain medical records prior to the conscription examination; however, these records could not be traced in some cases. Difficulty in tracing back past documents may be a potential weakness in the Korean military TB control program. In addition, treatment history of tuberculosis before military service was analysed depending on the memory of soldiers himself in most cases. This was inevitable because of low notification rate of tuberculosis in private sector and difficulty in getting past medical record during military service. Third, relatively small number of tuberculosis cases was enrolled. Although our study population was a representative sample of young soldiers at risk for pulmonary tubeculosis that are stationed in the area adjacent to Seoul, it may be a small portion of patients considering the incidence of tuberculosis in Korean military (5).
In conclusion, the prevalence of drug resistant tuberculosis among young soldiers in the Korean military was still high, even with a strict tuberculosis control program in place. Based on our results and the limited data available, we suggest that relapsed tuberculosis cases in the military should be cautiously managed until the drug susceptibility test report is completed, even if the previous treatment results were satisfactory.
Figures and Tables
 | Fig. 1Multi-drug resistance (MDR) among pulmonary tuberculosis (TB) cases according to military rank. |
ACKNOWLEDGEMENT
The authors are grateful to Dr. Won-Jung Koh, Samsung Medical Center, for critical reviewing of the manuscript.
References
1. Espinal MA, Kim SJ, Suarez PG, Kam KM, Khomenko AG, Migliori GB, Baez J, Kochi A, Dye C, Raviglione MC. Standard short-course chemotherapy for drug-resistant tuberculosis: treatment outcomes in 6 countries. JAMA. 2000. 283:2537–2545.
2. Global tuberculosis control: surveillance, planning, financing. WHO report 2007. Geneva: World Health Organization;(WHO/HTM/TB/2007.376).
3. Smith B, Ryan MA, Gray GC, Polonsky JM, Trump DH. Tuberculosis infection among young adults enlisting in the United States Navy. Int J Epidemiol. 2002. 31:934–939.

4. Ciftci F, Tozkoparan E, Deniz O, Bozkanat E, Kibaroglu E, Demirci N. The incidence of tuberculosis in the armed forces: a good reflection of the whole population. Int J Tuberc Lung Dis. 2004. 8:965–968.
5. Kang CI, Choi CM, Kim DH, Kim CH, Lee DJ, Kim HB, Kim NJ, Oh MD, Choe KW. Pulmonary tuberculosis in young Korean soldiers: incidence, drug resistance and treatment outcomes. Int J Tuberc Lung Dis. 2006. 10:970–974.
6. Seung KJ, Bai GH, Kim SJ, Lew WJ, Park SK, Kim JY. The treatment of tuberculosis in South Korea. Int J Tuberc Lung Dis. 2003. 7:912–919.
7. Ji SH, Kim HJ, Choi CM. Management of tuberculosis outbreak in a small military unit following the Korean national guideline. Tuberc Respir Dis. 2007. 62:5–10.

8. Joh JS, Lee CH, Lee JE, Park YK, Bai GH, Kim EC, Han SK, Shim YS, Yim JJ. The interval between initiation of anti-tuberculosis treatment in patients with culture-positive pulmonary tuberculosis and receipt of drug-susceptibility test results. J Korean Med Sci. 2007. 22:26–29.

9. Diagnostic Standards and Classification of Tuberculosis in Adults and Children. Am J Respir Crit Care Med. 2000. 161:1376–1395.
10. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, Lee JK, Kim SJ. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
11. Wayne LG. Simple pyrazinamidase and urease tests for routine identification of mycobacteria. Am Rev Respir Dis. 1974. 109:147–151.
12. Centers for Disease Control (CDC). Nosocomial transmission of multidrug-resistant tuberculosis among HIV-infected persons-Florida and New York, 1988-1991. MMWR Morb Mortal Wkly Rep. 1991. 40:585–591.
13. Frieden TR, Sterling T, Pablos-Mendez A, Kilburn JO, Cauthen GM, Dooley SW. The emergence of drug-resistant tuberculosis in New York City. N Engl J Med. 1993. 328:521–526.

14. Ruddy M, Balabanova Y, Graham C, Fedorin I, Malomanova N, Elisarova E, Kuznetznov S, Gusarova G, Zakharova S, Melentyev A, Krukova E, Golishevskaya V, Erokhin V, Dorozhkova I, Drobniewski F. Rates of drug resistance and risk factor analysis in civilian and prison patients with tuberculosis in Samara Region, Russia. Thorax. 2005. 60:130–135.

15. Choi JC, Lim SY, Suh GY, Chung MP, Kim H, Kwon OJ, Lee NY, Park YK, Bai GH, Koh WJ. Drug resistance rates of Mycobacterium tuberculosis at a private referral center in Korea. J Korean Med Sci. 2007. 22:677–681.

16. Lee JH, Chang JH. Drug-resistant tuberculosis in a tertiary referral teaching hospital of Korea. Korean J Intern Med. 2001. 16:173–179.
17. Kim SY, Jeong SS, Kim KW, Shin KS, Park SG, Kim AK, Cho HJ, Kim JO. Drug-resistant pulmonary tuberculosis in a tertiary referral hospital in Korea. Korean J Intern Med. 1999. 14:27–31.
18. Granich RM, Oh P, Lewis B, Porco TC, Flood J. Multidrug resistance among persons with tuberculosis in California, 1994-2003. JAMA. 2005. 293:2732–2739.

19. Arevalo M, Solera J, Cebrian D, Bartolome J, Robles P. Risk factors associated with drug-resistant Mycobacterium tuberculosis in Castilla-la-Mancha (Spain). Eur Respir J. 1996. 9:274–278.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download