Abstract
A 70-yr-old woman complained of left sided chest pain and non-bilious vomiting for four days after taking a gastric bloating agent for an upper gastrointestinal study. The chest radiography revealed gastric air-fluid levels and bowel loops in the left thoracic cavity. An emergency thoracotomy was performed. The abdominal organs (stomach, spleen, splenic flexure of the colon) were in the left thorax and the entire left hemidiaphragm was absent. There were no diaphragmatic remnants visible for reconstruction of the left diaphragm. We provided warm saline irrigation and performed a left lower lobe adhesiotomy. Thirteen days after surgery, the chest radiography showed improvement in the herniation but mild haziness remained at the left lower lung field. Here we present the oldest case of congenital diaphragmatic agenesis presenting with transient gastric volvulus and diaphragmatic hernia.
We report a rare case of surgically confirmed total absence of the hemidiaphragm in a 70-yr-old woman with the clinical presentation of an acute mesenteroaxial gastric volvulus and diaphragmatic eventration. The acute gastric volvulus (AGV) and herniated abdominal organs resolved spontaneously without reconstruction of the diaphragm.
A 70-yr-old woman, previously in good health was transferred to our hospital with the history of left sided chest pain, non-bilious vomiting and shortness of breath for four days. Six days before admission, the patient had a routine health check-up including chest radiography and upper gastrointestinal study (UGIS) using a gastric bloating agent at a local clinic. According to the referring clinic, the chest radiography and UGIS were normal (Fig. 1A, 2A). However, after taking the gastric bloating agent the patient developed increasing epigastric pain and nausea.
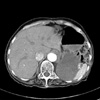
On admission, the respiratory rate of the patient was 38 breaths/min and the oxygen saturation was 91% in room air. Physical examination showed absent breath sounds and dull to percussion findings at the left lung base. The chest radiography revealed gastric air-fluid levels and bowel loops in the left thoracic cavity. After the placement of a nasogastric tube, the chest radiography showed displacement of the tip of the tube to the dilated stomach located in the left thoracic cavity (Fig. 1B). An UGIS using gastrograffin was performed without a bloating agent (Fig. 2B). The UGIS showed no transit of the gastrograffin through the duodenum and a hook-like image was noted at the medial portion of the herniated stomach. A chest CT revealed absence of the left side of the diaphragm (Fig. 3). The impression was that the patient had a mesenteroaxial gastric volvulus with a diaphragmatic hernia. The patient underwent surgical exploration.
A left posterolateral thoracotomy was done at the sixth intercostal space. We examined the surface of the entire lung field but could not find any diaphragmatic tissue. The abdominal organs (stomach, spleen, splenic flexure of colon) were present in the left thoracic cavity (Fig. 4). We attempted to rearrange the contents for devolvulation but could not achieve this due to the presence of severe pleural adhesions. Warm saline irrigation and a left lower lobe adhesiotomy were performed. There was no diaphragmatic tissue; we could not repair the diaphragm and return the abdominal organs, from the thorax, to the abdomen. The pleural cavity was closed in the usual manner. Conservative treatment was continued with nothing per oral and nasogastric drainage. Follow-up UGIS was performed 10 days after surgery (Fig. 2C); the abdominal organs remained in the left thoracic cavity but there was no disturbance of gastric passage. The patient improved by 12 days after surgery, on a soft diet. Thirteen days after surgery the chest radiography showed resolution of the herniation but mild haziness remained at the left lower lung field (Fig. 1C). The patient was discharged 20 days after admission. During the 1 yr of follow-up, the patient continued to do well.
The diaphragm is derived from the septum transversum, pleuroperitoneal membrane and the thoracic wall, while the gastrohepatic ligament and dorsal mesentery are minimally involved. Agenesis of the hemidiaphragm involves non-development of all of the related components and is very rare (1). Cunniff et al. (2) reported a 6% incidence of diaphragmatic agenesis in their review of 102 liveborn children with congenital diaphragmatic defects. This anomaly is usually associated with pulmonary hypoplasia, resulting in progressive respiratory failure and death in the neonatal period. However, some infants survive with this condition. In a review of the literature, asymptomatic presentation of a complete diaphragmatic agenesis has been previously reported (3, 4). In such rare cases, the gastrophrenic and gastrosplenic ligaments may have supported the intraabdominal organs so that they did not protrude into the thorax. In addition, the presence of pleuroperitoneal adhesions may have played a role in preventing herniation (5, 6). Loss of such physiologic balance may result from a sudden increase in the abdominal pressure.
Acute gastric volvulus and herniation of the abdominal organs into the thorax are associated with two factors: gastric distension and diaphragmatic eventration. It may be explained by an increased space around the stomach under a left diaphragmatic defect and by laxity of the gastrophrenic and gastrosplenic ligaments. Conditions that increase the intra-abdominal pressure such as excessive coughing or pregnancy may increase the intra-gastric pressure, leading to strangulation of the stomach with a diaphragmatic defect (5, 7). Singh et al. (7) reported a diaphragmatic agenesis in an adult similar to our case; a 22-yr-old primigravida (gestation 38 weeks) presented with an acute gastric volvulus and diaphragmatic agenesis was confirmed surgically. The elevated abdominal pressure, by the pregnancy, likely played an important role in the pathogenesis of the AGV.
In our case, the patient lived for 70 yr without any medical problems even though she had only a right hemidiaphragm. Just before this event, the patient had an UGIS for routine evaluation at a local clinic. The gastric bloating agent that was used for the UGIS might have led to the gastric distention and pressure overload. Therefore, the pressure imbalance may have caused the gastric volvulus and abdominal organ herniation into the thorax. On surgical exploration, we confirmed the absence of the left diaphragm. However, we could not reconstruct it. Spontaneous resolution of the gastric volvulus and herniation of abdominal organs was observed, as the abdominal pressure decreased.
Figures and Tables
Fig. 1
Chest radiographies. (A) There was no abnormal finding reported on from the local clinic 4 days before admission. (B) On admission, gastric air-fluid and bowel loops were observed in the left thoracic cavity and a coiled nasogastric tube was seen in the stomach. (C) The herniation improved but haziness was still seen at the left lower lobe after surgical intervention.

Fig. 2
Findings of upper gastrointestinal study (UGIS). (A) There was no disturbance of gastric passage at the local clinic 4 days before admission. (B) There were typical signs of a mesenteroaxial gastric volvulus; the stomach was in a vertical position with the pylorus higher than the cardia, and a double air-fluid level was seen; the antrum and pylorus were located inside the hernia with a hook like sign. (C) No passage disturbance of contrast media from the stomach into the duodenum; however, the stomach was still deviated into the thorax.

References
1. Langman J. Medical embryology. 1981. 4th ed. Baltimore: Williams and Willkins;282–317.
2. Cunniff C, Jones KL, Jones MC. Patterns of malformation in children with congenital diaphragmatic defects. J Pediatr. 1990. 116:258–261.

3. Tzelepis GE, Ettensohn DB, Shapiro B, McCool FD. Unilateral absence of the diaphragm in an asymptomatic adult. Chest. 1988. 94:1301–1303.

4. Wakai A, Winter DC, O'Sullivan GC. Unilateral diaphragmatic agenesis precluding laparoscopic cholecystectomy. JSLS. 2000. 4:259–261.
5. Okoye BO, Bailey DM, Cusick EL, Spicer RD. Prophylactic gastropexy in the asplenia syndrome. Pediatr Surg Int. 1997. 12:28–29.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download