Abstract
A refractory and resistant disease to conventional induction chemotherapy and relapsed disease are considered as the most important adverse prognostic factors for acute myeloid leukemia (AML). Sixty-one patients (median age, 33.6 yr) with relapsed or refractory AML were treated with the FLAG regimen that consisted of fludarabine (30 mg/m2, days 1-5), cytarabine (2.0 g/m2, days 1-5) and granulocyte colony-stimulating factor. Of the treated patients 29 patients (47.5%) achieved complete remission (CR). Higher CR rates were observed for patients with a first or second relapse as compared to patients with a primary refractory response or relapse after stem cell transplantation (HSCT). There was a significant difference in the response rates according to the duration of leukemia-free survival (pre-LFS) before chemotherapy (P=0.05). The recovery time of both neutrophils (≥500/µL) and platelets (≥20,000/µL) required a median of 21 and 18 days, respectively. Treatment-related mortality (TRM) occurred in seven patients (11.4%), of which 71.4% of TRM was caused by an invasive aspergillosis infection. After achieving CR, 18 patients underwent consolidation chemotherapy and six patients underwent allogeneic HSCT. In conclusion, FLAG chemotherapy without idarubicin is a relatively effective and well-tolerated regimen for relapsed or refractory AML and the use of FLAG chemotherapy has allowed intensive post-remission therapy including HSCT.
Despite an improvement in the treatment and remission rate for patients with acute myeloid leukemia (AML), only 30-40% of patients show long-term survival (1). Modern induction chemotherapy will result in complete remission in 50-90% of patients with de novo disease, but between 10 and 25% of patients will have primary refractory disease and the majority of those who gain remission will relapse within 3 yr of diagnosis (2). Treatment of relapsed leukemia is difficult and well-controlled trials in this group of patients are uncommon.
Combination therapy with fludarabine phosphate (F-AMP) and cytarabine (ara-C) has been advocated as a potentially useful chemotherapeutic regimen for the treatment of relapsed AML. This recommendation arises from the observation that F-AMP potentiates the intracellular accumulation of the active metabolite, ara-C 5'triphosphate (ara-CTP) in leukemic cells (3), thereby increasing the cytotoxic effect of high-dose ara-C, one of the most useful agents in the treatment of AML (4, 5). Gandhi et al. (3, 6) demonstrated that the combination of fludarabine and ara-C resulted in a significant increase in intracellular retention of ara-CTP. Prior to fludarabine treatment, granulocyte colony stimulating factor (G-CSF) increases the fraction of cells in cycle when they are most vulnerable to ara-C and enhances the incorporation of ara-C in to DNA (7, 8). The FLAG regimen, which combines fludarabine, high dose ara-C, and G-CSF, has recently been used with encouraging results in poor risk AML, myelodysplastic syndrome, and refractory or relapsed acute lymphoblastic leukemia (ALL). In addition, the toxicity of the combination was also low (9-15).
In this study, we report the clinical effectiveness and toxicities of FLAG chemotherapy in 61 patients with relapsed or refractory AML.
Sixty-one eligible patients with refractory and relapsed AML were treated with FLAG chemotherapy without idarubicin between November 2003 and September 2007. To be eligible for treatment with the FLAG regimen, patients had to have a serum bilirubin level ≤2 mg/dL, a creatinine ≤2 mg/dL, and no evidence of cardiac dysfunction. The patients were recruited from three National University Hospitals and provided informed consent for this treatment.
The diagnosis and classification of AML were determined according to the French-American-British (FAB) classification and was confirmed by cytochemical staining and immunophenotyping of the pretreatment marrow or blood samples. In addition, cytogenetic and molecular studies were also performed in all patients. The enrolled patients consisted of patients with M0 (n=1), M1 (n=6), M2 (n=19), M4 (n=9), M5 (n=10), M6 (n=5), M7 (n=1), mixed (n=4), and secondary (n=6) AML. Six patients were identified as having favorable cytogenetic abnormalities confined to t (8;21) and inv (16), regardless of other abnormalities. In contrast, 15 patients were identified as having poor cytogenetic abnormalities confined to t (11p,12q), del (8), t (1:16), trisomy 8, and Ph chromosome or other complex karyotypes. Moreover, 38 patients had normal karyotypes classified as intermediate risk. Performance status (PS) was determined for each patient according to World Health Organization (WHO) criteria; 40 patients were PS 0 or 1, 19 patients were PS 2, and 2 patients were in PS 3.
The primary induction regimen for remission was consisted of idarubicin (IDA) (12 mg/m2/day IV over 30 min on days 1-3) in combination with ara-C (100 or 200 mg/m2/day IV continuously on days 1-7) or N4-behenoyl-1-D-arabinofuranosyl-cytosine (BH-AC) (16) (age ≤40 yr, 300 mg/m2/day IV over 4 hr on days 1-7; age >40 yr, 200 mg/m2/day). The patients who achieved a remission were treated with post-remission chemotherapy that included high-dose ara-C (3 g/m2 IV every 12 hr on days 1, 3, and 5) as consolidation. The patients who had a matched donor underwent allogeneic hematopoietic stem cell transplantation (HSCT).
The FLAG regimen consisted of fludararbine (30 mg/m2/day IV over 30 min on days 1-5) in combination with ara-C (2 g/m2/day IV over 4 hr on days 1-5; age between 50 and 60 yr or for those >60 yr the standard infusion doses of fludarabine and ara-C were reduced by one-third). G-CSF was administered at 5 µg/kg from day 0 until neutrophil recovery (≥a neutrophil count of 500/µL).
We considered complete remission (CR) to be morphologically normal marrow with ≤5% blasts concomitant with normal peripheral and differential counts, including a neutrophil count ≥1×109/L and a platelet count ≥100×109/L. Patients who did not respond to induction therapy were considered to be in non-remission (NR), whereas patients whose response could not be measured were considered to be non-measurable (NM).
Hematologic and non-hematologic toxicity were measured and graded according to the criteria of the WHO. Additional side effects and other adverse events not covered by the WHO toxicity system were documented, including an assessment of the severity of response to therapy. Post-chemotherapy cytopenia was monitored by hematologic assessments ≥three times weekly, until neutrophil and platelet counts recovered. Treatment-related mortality (TRM) was defined as deaths resulting from a complication developing prior to recovery from chemotherapy.
Statistical analyses were performed using SPSS statistical software version 12.0 (SPSS, Inc., Chicago, IL, U.S.A.). Comparisons between proportions were assessed with the chi-squared test. Overall survival (OS) was defined as the time from transplantation to the date of last follow-up or death from any cause. Leukemic-free survival (LFS) was calculated from the date of CR to the recording of disease relapse or death from any cause. Patients who died in CR were plotted as censored. The actuarial curve for OS was plotted corresponding to the Kaplan-Meier method. P values <0.05 were considered statistically significant.
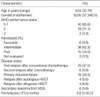
As shown in Table 1, the disease status and hematologic features in the 61 patients were variable. The median preleukemic free survival (pre-LFS) before FLAG chemotherapy was 8.8 months (range, 0-56.5 months).
Forty-nine patients were evaluated for response and the clinical outcomes of FLAG chemotherapy as summarized in Table 2. Twelve patients (19.7%) could not be evaluated for clinical responses; specifically, 7 patients (11.4%) had TRM and 5 patients could not undergo marrow examination due to debilitating conditions.
Overall, 29 patients (47.5%) achieved a CR and 19 patients (32.8%) had a resistant disease to FLAG chemotherapy. Patients with 1st or 2nd relapses had response rates 58.6 and 66.7%, respectively. However, patients with primary refractoriness or relapse after HSCT showed lower response rates of 38.9 and 12.5%, respectively. Patients who had ≥6 months duration of pre-LFS had relatively high CR rates compared to those who had ≤6 months (71.4% vs. 33.3% respectively, P=0.05). The CR rate was 50.9% in de novo AML, while the CR rate was 16.7% in secondary AML. The patients with de novo AML had higher response rates than those with secondary AML, although not statistically significance (P=0.08). However, when patients were stratified by cytogenetic prognostic group, the patients with favorable cytogenetics failed to show a significant difference in therapeutic outcomes compared to those with intermediate or poor cytogenetics. Also, there were no statistical differences in CR rates according to age (age <50 yr or age ≥50 yr) and disease status before FLAG chemotherapy.
The median duration of survival of all patients was 14.3 months (range, 1.3-75.1 months) and the 3-yr probability of OS was 29.8±7.1% (Fig. 1). After achieving CR in 29 patients, 6 patients underwent allogeneic HSCT and 18 patients received consolidation chemotherapy. The remaining five patients did not receive further therapy because of relapse or poor PS. After consolidation, the median LFS after FLAG chemotherapy was 17.1 months (range, 0.2-27.6 months) and 17 patients are still in continuous CR with a median follow-up of 7.59 months (range, 0.2-27.6 months).
All patients experienced profound granulocytopenia. The median recovery time for neutrophils (≥0.5×109/L) and platelets (≥50×109/L) from the day chemotherapy commenced was 21 and 20 days, respectively. A median of 10 red cell units (range, 2-44 red cell units) were required. Non-hematologic toxicity was mild-to-moderate; infection was the most common side effect. The toxicities (≥grade 3) consisted of infection (26.2%), mucositis (9.8%), hepatic dysfunction (8.1%) and gastro-intestinal dysfunction including nausea and vomiting (11.4%) (Table 3).
The TRM was 11.4%; 5 patients died due to acute respiratory failure from fungal pneumonia, one patient died due to sepsis, and one patient died due to hemorrhagic complications after FLAG consolidation. Most cases of fungal pneumonia were caused by an invasive aspergillosis.
The prognosis of patients with relapsed or refractory AML is poor and has thus prompted a search for novel drugs or drug combinations to improve the initial response rate and prolong the survival. Indeed, several chemotherapy regimens have been used in patients with refractory or relapsed AML with response rates of 29-44% (17-19).
Recently, the FLAG regimen or with idarubicin has been proposed as a more effective and relatively safe treatment for relapsed or refractory patients with AML, characterized by relatively high CR rates and a low TRM. In addition, FLAG chemotherapy or with idarubicin is suggested to be a valuable remission induction regimen for poor risk leukemias and myelodysplastic syndrome. The combination of fludarabine and ara-C is potentially a useful chemotherapeutic regimen for the treatment of AML. Various studies have determined the clinical response of the FLAG regimen or with idarubicin (9, 10, 12-14, 20) to be between 50 and 81%. Yavuz et al. (21) and Pastore et al. (22) suggested that the CR rate of FLAG-ida was 53.6 and 52.1% in the treatment of the patients with relapsed and refractory AML, respectively. In our study, the complete remission rate of FLAG without idarubicin was 47.5%, similar to that of FLAG with idarubicin. When compared with FALG-ida with respect to toxicity, the incidence of severe infection and mucositis (≥grade 3) was 26.2% and 9.8%, respectively. This is relatively low compared with other studies that reported incidences of 45-65% for relapsed and refractory patients.
When we classified the patients according to the duration of pre-LFS before chemotherapy, the response rates were somewhat different (11, 12). We also found that disease type (de novo or secondary) showed a slight trend in relation to CR rates, although the relationship was not significant. In our study, we found that the clinical response after the FLAG regimen was greater in the first or second relapsed patients (55 and 67%, respectively) than in primary refractory patients. These results are consistent to those of previous studies (14, 23). We observed relatively lower CR rates in patients with primary refractory (38.9%) or relapse after HSCT (12.5%). On the other hand, we did not find that the patient's age and karyotyping risks had a significant influence on CR rates.
As with previous studies that have suggested that additional therapy is required to achieve long term survival in responsive patients, we found that the duration of remission after FLAG chemotherapy remained short-term. Autologous or allogeneic HSCT after FLAG chemotherapy represented the best consolidation strategies for the responsive patients because FLAG chemotherapy showed a low TRM and a high response rate (20, 23-25). Following CR achievement, six patients underwent allogeneic HSCT in this study. Five of these patients remained in CR at the time of analysis.
The toxicity of this regimen was acceptable, especially considering that most patients had been heavily pretreated. The major cause of early mortality in TRM was fungal infections (71.4%). There were reports that HEPA filters could provide the protection for highly immunocompromised patients with hematologic malignancies and are also effective at controlling outbreaks due to air contamination of aspergillosis and candidiasis (26, 27). The situation of this study was quite different because most patients were managed in regular rooms after chemotherapy. However, the incidence of TRM seemed to be acceptable and hematologic recovery was relatively fast, compared to the previous studies (12, 13, 15, 20, 28-30).
In conclusion, our results suggest that FLAG chemotherapy is a well-tolerated regimen for relapsed or refractory AML patients. In particular, FLAG chemotherapy may be especially useful for patients who have a sibling or unrelated donor for performing allogeneic HSCT.
Figures and Tables
 | Fig. 1The probability of leukemic free survival (LFS) and overall survival (OS) after FLAG chemotherapy in patients with relapsed or refractory AML (n=61). |
References
3. Gandhi V, Plunkett W. Modulation of arabinosylnucleoside metabolism by arabinosylnucleotides in human leukemia cells. Cancer Res. 1988. 48:329–334.
4. Mayer RJ, Davis RB, Schiffer CA, Berg DT, Powell BL, Schulman P, Omura GA, Moore JO, McIntyre OR, Frei E 3rd. Cancer and Leukemia Group B. Intensive postremission chemotherapy in adults with acute myeloid leukemia. N Engl J Med. 1994. 331:896–903.

5. Bishop JF, Matthews JP, Young GA, Szer J, Gillett A, Joshua D, Bradstock K, Enno A, Wolf MM, Fox R, Cobcroft R, Herrmann R, Van Der Weyden M, Lowenthal RM, Page F, Garson OM, Juneja S. A randomized study of high-dose cytarabine in induction in acute myeloid leukemia. Blood. 1996. 87:1710–1717.
6. Gandhi V, Estey E, Keating MJ, Plunkett W. Fludarabine potentiates metabolism of cytarabine in patients with acute myelogenous leukemia during therapy. J Clin Oncol. 1993. 11:116–124.

7. Tafuri A, Andreeff M. Kinetic rationale for cytokine-induced recruitment of myeloblastic leukemia followed by cycle-specific chemotherapy in vitro. Leukemia. 1990. 4:826–834.
8. Tosi P, Visani G, Ottaviani E, Manfori S, Zinzani PL, Tura S. Fludarabine+Ara-C+G-CSF: cytotoxic effect and induction of apoptosis
on fresh acute myeloid leukemia cells. Leukemia. 1994. 8:2076–2082.
9. Estey E, Thall P, Andreeff M, Beran M, Kantarjian H, O'Brien S, Escudier S, Robertson LE, Koller C, Kornblau S, Pierce S, Freireich EJ, Deisseroth A, Keating M. Use of granulocyte colony-stimulating factor before, during, and after fludarabine plus cytarabine induction therapy of newly diagnosed acute myelogenous leukemia or myelodysplastic syndromes: comparison with fludarabine plus cytarabine without granulocyte colony-stimulating factor. J Clin Oncol. 1994. 12:671–678.

10. Visani G, Tosi P, Zinzani PL, Manfroi S, Ottaviani E, Testoni N, Clavio M, Cenacchi A, Gamberi B, Carrara P, Gobbi M, Tura S. FLAG (fludarabine+high-dose cytarabine+G-CSF): an effective and tolerable protocol for the treatment of 'poor risk' acute myeloid leukemias. Leukemia. 1994. 8:1842–1846.
11. Clavio M, Carrara P, Miglino M, Pierri I, Canepa L, Balleari E, Gatti AM, Cerri R, Celesti L, Vallebella E, Sessarego M, Patrone F, Ghio R, Damasio E, Gobbi M. High efficacy of fludarabine-containing therapy (FLAG-FLANG) in poor risk acute myeloid leukemia. Haematologica. 1996. 81:513–520.
12. Montillo M, Mirto S, Petti MC, Latagliata R, Magrin S, Pinto A, Zagonel V, Mele G, Tedeschi A, Ferrara F. Fludarabine, cytarabine, and G-CSF (FLAG) for the treatment of poor risk acute myeloid leukemia. Am J Hematol. 1998. 58:105–109.

13. Nokes TJ, Johnson S, Harvey D, Goldstone AH. FLAG is a useful regimen for poor prognosis adult myeloid leukaemias and myelodysplastic syndromes. Leuk Lymphoma. 1997. 27:93–101.

14. Jackson G, Taylor P, Smith GM, Marcus R, Smith A, Chu P, Littlewood TJ, Duncombe A, Hutchinson M, Mehta AB, Johnson SA, Carey P, MacKie MJ, Ganly PS, Turner GE, Deane M, Schey S, Brookes J, Tollerfield SM, Wilson MP. A multicentre, open, non-comparative phase II study of a combination of fludarabine phosphate, cytarabine and granulocyte colony-stimulating factor in relapsed and refractory acute myeloid leukaemia and de novo refractory anaemia with excess of blasts in transformation. Br J Haematol. 2001. 112:127–137.
15. Virchis A, Koh M, Rankin P, Mehta A, Potter M, Hoffbrand AV, Prentice HG. Fludarabine, cytosine arabinoside, granulocyte-colony stimulating factor with or without idarubicin in the treatment of high risk acute leukaemia or myelodysplastic syndromes. Br J Haematol. 2004. 124:26–32.

16. Park HS, Kim DW, Kim CC, Kim HK, Kim JS, Hwang TJ, Kim HJ, Kim HS, Song HS, Park JW, Ahn HS, Chung TJ, Cho KS, Lee KS, Choi YM. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen--a prospective, cooperative multicenter study. Semin Hematol. 1996. 33:24–29.
17. Martinez JA, Martin G, Sanz GF, Sempere A, Jarque I, de la Rubia J, Sanz MA. A phase II clinical trial of carboplatin infusion in high-risk acute nonlymphoblastic leukemia. J Clin Oncol. 1991. 9:39–43.
18. Larrea L, Martinez JA, Sanz GF, Martin G, de la Rubia J, Jimenez C, Jarque I, Cid A, Lopez A, Sanz MA. Carboplatin plus cytarabine in the treatment of high-risk acute myeloblastic leukemia. Leukemia. 1999. 13:161–165.

19. Sanz MA, Sanz GF, Martinez JA, Senent L, Lopez F, Palau J, Martin G, Jarque I. Carboplatin alone or in combination in high-risk acute nonlymphoblastic leukemia. Ann Oncol. 1992. 3:39–42.

20. Huhmann IM, Watzke HH, Geissler K, Gisslinger H, Jager U, Knobl P, Pabinger I, Korninger L, Mannhalter C, Mitterbauer G, Schwarzinger I, Kalhs P, Haas OA, Lechner K. FLAG (fludarabine, cytosine arabinoside, G-CSF) for refractory and relapsed acute myeloid leukemia. Ann Hematol. 1996. 73:265–271.

21. Yavuz S, Paydas S, Disel U, Sahin B. IDA-FLAG regimen for the therapy of primary refractory and relapse acute leukemia: a single-center experience. Am J Ther. 2006. 13:389–393.

22. Pastore D, Specchia G, Carluccio P, Liso A, Mestice A, Rizzi R, Greco G, Buquicchio C, Liso V. FLAG-IDA in the treatment of refractory/relapsed acute myeloid leukemia: single-center experience. Ann Hematol. 2003. 82:231–235.

23. Carella AM, Cascavilla N, Greco MM, Melillo L, Sajeva MR, Ladogana S, D'Arena G, Perla G, Carotenuto M. Treatment of "poor risk" acute myeloid leukemia with fludarabine, cytarabine and G-CSF (flag regimen): a single center study. Leuk Lymphoma. 2001. 40:295–303.

24. Byrne JL, Dasgupta E, Pallis M, Turzanski J, Forman K, Mitchell D, Haynes AP, Russell NH. Early allogeneic transplantation for refractory or relapsed acute leukaemia following remission induction with FLAG. Leukemia. 1999. 13:786–791.

25. Pawson R, Potter MN, Theocharous P, Lawler M, Garg M, Yin JA, Rezvani K, Craddock C, Rassam S, Prentice HG. Treatment of relapse after allogeneic bone marrow transplantation with reduced intensity conditioning (FLAG +/- Ida) and second allogeneic stem cell transplant. Br J Haematol. 2001. 115:622–629.
26. Hahn T, Cummings KM, Michalek AM, Lipman BJ, Segal BH, McCarthy PL Jr. Efficacy of high-efficiency particulate air filtration in preventing aspergillosis in immunocompromised patients with hematologic malignancies. Infect Control Hosp Epidemiol. 2002. 23:525–531.

27. Oren I, Haddad N, Finkelstein R, Rowe JM. Invasive pulmonary aspergillosis in neutropenic patients during hospital construction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol. 2001. 66:257–262.

28. Clavio M, Gatto S, Beltrami G, Cerri R, Carrara P, Pierri I, Canepa L, Miglino M, Balleari E, Masoudi B, Damasio E, Ghio R, Sessarego M, Gobbi M. First line therapy with fludarabine combinations in 42 patients with either post myelodysplastic syndrome or therapy related acute myeloid leukaemia. Leuk Lymphoma. 2001. 40:305–313.

29. Ferrara F, Melillo L, Montillo M, Leoni F, Pinto A, Mele G, Mirto S. Fludarabine, cytarabine, and G-CSF (FLAG) for the treatment of acute myeloid leukemia relapsing after autologous stem cell transplantation. Ann Hematol. 1999. 78:380–384.

30. Ferrara F, Palmieri S, Pocali B, Pollio F, Viola A, Annunziata S, Sebastio L, Schiavone EM, Mele G, Gianfaldoni G, Leoni F. De novo acute myeloid leukemia with multilineage dysplasia: treatment results and prognostic evaluation from a series of 44 patients treated with fludarabine, cytarabine and G-CSF (FLAG). Eur J Haematol. 2002. 68:203–209.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download