Abstract
The World Health Organization (WHO) classification of central nervous system (CNS) tumors incorporates morphology, cytogenetics, molecular genetics, and immunologic markers. Despite the relatively large number of CNS tumors with clonal chromosome abnormalities, only few studies have investigated cytogenetic abnormalities for CNS tumors in Korea. Thus, we investigated 119 CNS tumors by conventional G-banded karyotypes to characterize patterns of chromosomal abnormalities involving various CNS tumors, and 92.4% of them were cultured and karyotyped successfully. Totally, 51.8% of karyotypable CNS tumors showed abnormal cytogenetic results, including neuroepithelial tumors (75.0%), meningeal tumors (71.1%), pituitary adenomas (4.2%), schwannomas (44.4%), and metastatic tumors (100.0%). Glioblastomas had hyperdiploid, complex karyotypes, mainly involving chromosomes Y, 1, 2, 6, 7, 10, 12, 13, and 14. Monosomy 22 was observed in 56.4% of meningiomas. There was a significant increase in the frequencies of karyotypic complexity according to the increase of WHO grade between grades I and II (P=0.0422) or IV (P=0.0101). Abnormal karyotypes were more complex at high-grade tumors, suggesting that the karyotype reflects the biologic nature of the tumor. More detailed cytogenetic and molecular characterizations of CNS tumors contribute to better diagnostic criteria and deeper insights of tumorigenesis, eventually resulting in development of novel therapeutic strategies.
Central nervous system (CNS) tumors include a broad spectrum of diseases and reveal various histological, biological, and clinical characteristics. Worldwide, cancers of the brain and nervous system accounted for some 189,000 new cases and 142,000 deaths annually (1.7% of new cancers; 2.1% of cancer deaths) in the year 2002 (1). Anaplastic astrocytomas and glioblastomas account for approximately 38% of primary CNS tumors; meningiomas and other mesenchymal tumors account for approximately 27%. Other less common primary CNS tumors include pituitary tumors, schwannomas, CNS lymphomas, oligodendrogliomas, ependymomas, low-grade astrocytomas, and medulloblastomas, in decreasing orders (2). The recently revised and commonly used World Health Organization (WHO) classification of CNS tumors incorporates and interrelates morphology, cytogenetics, molecular genetics, and immunologic markers to be universally applicable and prognostically valid (3, 4).
Cytogenetic information is essential for the identification of key genes in tumorigenesis by focusing on specific chromosomal sites. To assess the relevance of chromosomal and genetic abnormalities in CNS tumors, the careful assessment of cytogenetic characteristics for individual type of CNS tumors are needed. Several studies have shown that the majority of meningiomas with loss of chromosome 22 carry mutations in the neurofibromatosis type 2 gene (NF2) on 22q12.2 (5). According to recent statistics, clonal chromosome abnormalities have been described in approximately 932 CNS tumors from 161 references (6). In spite of the relatively large number of CNS tumors with clonal chromosome abnormalities, only few studies have investigated cytogenetic abnormalities for CNS tumors in Korea. Thus, in the present study, 119 CNS tumors were investigated by conventional karyotypes to characterize patterns of chromosomal abnormalities involving various CNS tumors. We also aimed to compare those cytogenetic abnormalities and complexities with WHO classification and grade.
One hundred nineteen CNS tumors from 110 patients who were diagnosed, operated, and followed up at Department of Neurosurgery, Dong-A University Medical Center between July, 2002 and June, 2007 were studied. The patient ages at diagnosis ranged between 6 and 79 yr (mean 46 yr); 44 were male and 66 female. Nine patients were analyzed twice due to recurrent or residual CNS tumors from two meningiomas and seven astrocytic tumors. Informed consent was obtained from all of the patients in accordance with the guidelines of Institutional Review Board.
The revised 2002 WHO classification for CNS tumors was adopted to formulate the histological analysis (3). The WHO grading of CNS tumors establishes a malignancy scale and predicts the biological behavior based on histological features of the tumor (3, 4). WHO grade I included two pilocytic astrocytomas, 41 meningiomas, two craniopharyngiomas, three hemangioblastomas, and nine schwannomas. WHO grade II included five diffuse astrocytomas, two atypical meningiomas, one oligodendroglioma, one ependymoma, and one hemangiopericytoma. WHO grade III included three anaplastic astrocytomas. WHO grade IV contained 16 glioblastomas and one medulloblastoma. Thirty-two tumors including 25 pituitary adenomas, one yolk sac tumor, three lymphomas, and three metastatic tumors could not be graded due to the insufficiencies of clinicopathologic data.
Cytogenetic analysis was carried out on fresh surgical tumor specimens, which proved to contain tumors by pathologic reading of frozen sections. Fresh tissues were mashed and finely minced to dissociate the cells in Petri dish containing RPMI 1640 medium with L-glutamine. The cells were in situ cultured with Chang medium supplemented with L-glutamine and P-streptomycin at 37℃ in a 5% CO2 atmosphere for 7-10 days. When there were sufficient numbers of growing cells in the coverslips, the cell cultures were harvested. G-banded karyotypes were interpreted according to the recommendation of the International System for Human Cytogenetic Nomenclature (ISCN), 2005 (7). Twenty metaphases were examined whenever possible. The clonal abnormalities were defined as two or more cells with the same additional whole chromosome or structural chromosome rearrangement and three or more cells with the same chromosome missing. A complex karyotype was defined as the presence of three or more abnormalities.
Statistical analysis was performed using MedCalc version 9.3 (MedCalc Software, Mariakerke, Belgium). The two-tailed Fisher's exact test was used for comparisons of chromosomal results according to their WHO grades in the CNS tumors. P value of <0.05 was considered statistically significant.
Successful cultures were obtained on 110 of the 119 CNS tumors (92.4%) including 23 neuroepithelial tumors (21 astrocytic tumors [two pilocytic, five diffuse, and one anaplastic astrocytomas, and 13 glioblastomas], one oligodendoglioma, one ependymoma, and one medulloblastoma), 45 meningeal tumors (41 meningiomas [nine meningothelial, seven fibrous, 16 transitional, one psammomatous, three angiomatous, two microcytic, one sclerosing, and two atypical meningiomas], one hemangiopericytoma, and three hemangioblastomas), 24 pituitary adenomas, nine schwannomas, two metastatic tumors, one yolk sac tumor, two craniopharyngiomas, and three lymphomas (one case each NK cell, diffuse large B cell lymphoma, and Hodgkin disease). Culture failures were attributed to too tiny sample sizes, delay in sample transfer, low mitotic activities, and bacterial contaminations. Of the case successfully cultured, complete karyotypes were obtained on 108 of 110 CNS tumors (98.2%). Two CNS tumors (one diffuse astrocytoma and one glioblastoma) were not karyotyped and interpreted perfectly due to the complex nature of the abnormalities.
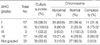
Totally, 57 of 110 CNS tumors (51.8%) had abnormal karyotypes. Eighteen of 24 neuroepithelial tumors (73.9%), 32 of 45 meningeal tumors (71.1%), one of 24 pituitary adenomas (4.2%), four of nine schwannomas (44.4%), and two of two metastatic tumors (100.0%) showed abnormal karyotypes. All of the others, including one yolk sac tumor, two craniopharyngiomas, and three lymphomas showed normal karyotypes. The results are summarized in Table 1.
According to WHO grades of CNS tumors, 35 of 55 WHO grade I (63.6%), eight of 10 WHO grade II (80.0%), and 10 of 14 WHO grade IV (71.4%) showed abnormal karyotypes (Table 2). In WHO grade III, only one tumor was interpretable and it showed a normal karyotype. The frequency of cytogenetic abnormalities showed a tendency to increase according to the change of WHO grade from grade I to grades II or IV, but not statistically significant. On the other hand, of the cases with abnormal karyotypes, 11 of 35 WHO grade I (31.4%), six of eight WHO grade II (75.0%), and eight of 10 WHO grade IV (80.0%) showed complex karyotypes. Accordingly, there was a significant increase in the frequencies of karyotypic complexity with respect to the increase of WHO grade between grades I and II (p=0.0422) or IV (p=0.0101). There was a tendency to increase between grades II and IV, but not statistically significant (p>0.05).
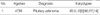
Twenty one astrocytic tumors were cultured, and two anaplastic astrocytomas and three glioblastomas showed the failure of tissue culture. Fifteen of 21 astrocytic tumors (71.4%) had abnormal karyotypes (Table 3) and six had normal karyotypes. Eight cases (38.0%) showed a hyperdiploidy, five of which especially revealing a massive hyperdiploidy, almost tetraploidy or triploidy. Three patients showed a hypodiploidy, mostly losing Y chromosome. A complex karyotype with over three abnormalities was seen in nine cases (42.9%).
Pilocytic astrocytomas (WHO grade I) were studied twice from one patient due to residual tumors, and all cases showed abnormal karyotypes. Additional materials attached to band 16q24 were shown to be primary abnormality in this case.
Five diffuse astrocytomas (WHO grade II) were studied; in two cases the karyotype was normal, in other two cases the karyotype was abnormal and in the remaining one case, the karyotyping was not fully completed because of complex nature of the abnormality. One case of anaplastic astrocytoma (WHO grade III) showed a normal karyotype.
Thirteen cases of glioblastoma (WHO grade IV) were studied, and in three cases the karyotype was normal. One case from resection of a recurrent tumor could not be successfully interpreted due to the complex nature. Of the cases with abnormal cytogenetics, the karyotypes were diploid or near-diploid in six cases, near-tetraploid in one case, and near-triploid in two cases. In the majority of cases with abnormal karyotype, there was a mixture of normal and abnormal metaphases and only three cases had exclusively abnormal clonal cells.
Overall, among the cases with successful karyotypes, numeric changes were predominantly losses of chromosomes Y, 10, 13, and 14, and gains of chromosomes 2 and 12. The most frequent chromosomal loss was the loss of Y chromosome, observed in three cases (23.1%). The most commonly involved chromosomes, numeric or structural, were chromosome 12, observed in five cases (38.5%). Numeric and/or structural abnormality other than chromosome 12 involved chromosomes 1, 6, 7, and 14 in four cases (30.8%), and chromosomes 9, 10, 11, 13, 17, 19, and 22 in three cases (23.1%). The presence of one or more unidentified marker chromosomes was also observed in three cases.
One oligodendroglioma (Table 3) showed a hypodiploidy with a loss of X chromosome, an isochromosome for chromosome Xq10, additions to 1p36.3, 9p24, 13q32, 15q22, 17q23, and deletions of 1q25, 2q31, 4q31.1, 10p12, 10q23, 11q22, 16p22, 17q23, 22q13.
One recurrent ependymoma showed a hyperdiploidy with a reciprocal translocation between the short arm of chromosome 11 and the long arm of chromosome 13, trisomies for chromosomes X, 1, 2, 3, 5, 8, 9, 13, 15, 18, 19, and 21, and monosomies for chromosomes 4, 10, 13, 14, and 22 (Table 3).
In one recurrent medulloblastoma, a highly complex hypodiploid karyotype with multiple numerical and structural abnormalities was observed (Table 3).
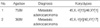
Forty-five meningeal tumors (Table 4) were karyotyped, and in 10 cases the karyotype was normal. Twenty-nine of 39 (74.4%) WHO grade I and all of three (100.0%) WHO grade II (two atypical meningiomas and one hemangiopericytoma) meningeal tumors showed abnormal karyotypes. Of the cases with abnormal cytogenetics, the karyotypes were diploid in six cases, hypodiploid in 20 cases, and hyperdiploid in six cases.
Loss of chromosome 22, which observed in 22 of 39 meningiomas (WHO grade I) (56.4%), was the most common consistent numerical chromosome change. Sole monosomy 22 was observed in seven cases (17.8%). Monosomy 22 with additional chromosome abnormalities was shown in 12 of 22 meningiomas (54.5%), involving chromosomes X (18.2%), 1 (31.8%), 12 (22.7%), and 20 (18.2%). The most common secondary chromosome abnormality associated with monosomy 22 was chromosome 1, observed in seven cases (31.8%). Clonal evolutions were found in six patients and unrelated clones were also noted in one patient. Primary numerical and/or structural chromosome abnormalities other than monosomy 22 were identified in seven patients (17.9%), involving chromosomes 5 (7.7%), 6 (10.3%), 7 (5.1%), 19 (7.7%), and 20 (5.1%).
Two atypical meningiomas (WHO grade II) were analyzed; in one case monosomy 22 with additional abnormalities was observed, in the other case, a reciprocal translocation between long arms of chromosome 2 and 12, gain of chromosomes X, 4, and 5 were shown as complex abnormalities.
One hemangiopericytoma (Table 4) showed a hypodiploidy with a loss of X chromosome.
Of 24 pituitary adenomas (Table 5) only one, carrying extensive necrosis in histopathology, showed a loss of Y chromosome in karyotype.
In schwannoma, loss of chromosome 22 as a sole abnormality was identified in three of nine cases. Other alterations involved an addition to 18p11.2 and deletions of 4q26 and 9q34 (Table 6).
As for metastatic tumors, a loss of Y chromosome was found as the sole chromosome abnormality in two adenocarcinomas, both metastasized from stomach cancers, presented in Table 7.
Cytogenetic information for CNS tumors has been relatively less understandable than the one for hematologic malignancies (8, 9). Although non-random chromosomal alterations have been identified in various CNS tumors, their clinical and molecular significance remains unclear. This lack of significance is partially due to technical difficulties in culture and to the karyotypic complexity. A large number of cytogenetically well-analyzed data for CNS tumors have still been required. To the best of our knowledge, this study reports the first comprehensive cytogenetic aberrations of CNS tumors in Korea. In this study, 92.4% of CNS tumors could be successfully cultured. Of the cases with successful cultures, 98.2% of CNS tumors were completely karyotyped. A cytogenetic analysis may provide an accurate tool for assessing disease risk in patients with CNS tumors. In addition, these cytogenetic results may serve as a target for novel therapeutic approaches in CNS tumors.
Cytogenetic abnormalities might result in aggressive disease behavior in CNS tumors by promoting tumor cell proliferation as likely as in other various types of cancers. WHO grades II (80.0%) or IV (71.4%) had more frequent karyotype abnormalities than with grade I (63.6%). In karyotypic complexity according to WHO grades of CNS tumor, there was a significant increase in the frequencies of karyotypic complexity between grades I and II (P=0.0422) or IV (P=0.0101). High-grade tumors were more likely to demonstrate cytogenetic abnormalities and complexity than low-grade tumors, suggesting that the karyotype reflects the biologic nature of the tumor.
This study might not accurately represent the cytogenetic abnormalities and complexities according to WHO grades, because the incidence differs depending on CNS tumors as well as WHO grades. Besides, WHO grade I tumors were much more than the others in this study. Therefore, we need to include other cases beyond WHO grade II, to make more comprehensive conclusions.
Astrocytomas and glioblastoma account for over 30% of all primary brain and CNS tumors (2, 10). Astrocytic tumors are highly variable tumors and show complex karyotypes, manifesting multi-step tumorigenesis events. Classic cytogenetics of low grade astrocytic tumors (pilocytic and diffuse astrocytomas) are characterized by normal karyotypes or abnormal karyotypes in the near-diploid range (11). Loss of Y chromosome is the most frequent event in glioblastoma, consistent with the results of a survey from the Cancer Genome Anatomy Project (CGAP) site. Among high-grade astrocytomas (WHO grades III-IV), the most common whole chromosomal gains and losses are as follows: -6, +7, -8, -9, -10, -13, -14, -17, and -22 (6).
Recent comparative genomic hybridization (CGH) studies for gliomas have identified novel regions of change, including gains of 1p34-p36, 12p13, and 20q13, amplifications at 1p36.2, 3q26, 3q27, 7p12, 7q21-q31, 8q24.1, 12p13, 12q13-q15, 17q24, 19q13.2, and 20q13.1, and losses at 1p22, 4q33-q35, 6q16, 6q23-q27, 9p21, 10q25-q26, 13q21.1, and 22q13 (12). The most frequently amplification gene in astrocytomas is epidermal growth factor receptor (EGFR at 7p12) gene (13). Classic cytogenetic and CGH studies of grades II and III astrocytomas demonstrated that chromosome 7 gains were among the most common genetic alterations (40-66%) (14, 15). Cyclin-dependent kinase 4 (CDK4) and MDM2 at 12q13-15 are amplified in approximately 10% to 25% of astrocytic tumors (16).
More recently, Cowell et al. (17) examined four glial cell lines derived from primary tumors. A bacterial artificial chromosome (BAC) array based CGH enabled the identification of deletions at the 9p13-p21 region harboring the p16/CDKN2A gene seen in all four tumors, which were confirmed with fluorescence in situ hybridizaiton (FISH) assays. Losses of chromosome 10 are quite frequent in high-grade astrocytomas. Most CGH and FISH studies have identified monosomy 10 as independent poor prognosis predictor (18, 19).
In this study, abnormal karyotypes were seen in 71.4% of astrocytic tumors, 42.9% of which were complex karyotypes. The majority of grades I and II astrocytomas showed normal or abnormal karyotypes with near-diploid and gains of chromosomes Y and 6. In glioblastomas, this study confirms and extends prior reports concerning gains of chromosomes 2 and 12 and losses of chromosomes Y, 10, 13, and 14. We observed common numeric and/or structural abnormality at chromosome 1, 6, 7, 9, 10, 11, 12, 13, 14, 17, 19, and 22.
In glioblastoma, tyrosine kinase inhibitors directed at epidermal growth factor receptor (ZD1839, OSI-774) were being explored as potential treatment modalities. Farnesyltransferase inhibitors (R115777), antagonists of the endothelin receptor, and inhibitors of de novo adenosine synthesis (SDX-102) may be effective. Not only will genetic alterations offer prognostication, but they will also serve as targets for directed therapies (20, 21).
In oligodendrogliomas, chromosomal alterations included deletions of 1p36, 9p, 10, and 22, and gains of chromosome 7, 8q, and 17q (22). The present study corresponds to deletions of 1q24, 10p12, 10q23, and 22q13, and additions to 17q23.
Ependymomas are well-delineated, moderately cellular gliomas and are the third most common brain tumors in children. The loss of heterozygosity (LOH) studies have identified LOH of 22q as the most frequent change, seen in approximately 30% of ependymomas (23). In this study, monosomy 22 was found in one ependymoma with hypertriploidy and multiple numeric changes.
Medulloblastomas (WHO grade IV) are a malignant, invasive embryonal tumor of the cerebellum that occurs primarily in children, having a predominantly neuronal differentiation and a tendency to metastasize through cerebrospinal fluid pathways. In adulthood, 80% of medulloblastomas occur in patients with 21 to 40 yr of age. The most frequent abnormality is loss of 17p, usually through the formation of an isochromosome, observed in 30% of medulloblastomas (24). One medulloblastoma in the current report showed highly complex hypodiploid karyotypes with nullosomy for chromosomes 13, 16, 17, and 18.
Meningiomas are slow growing, mostly benign, WHO grade I tumors. Although most meningiomas are benign tumors, as many as 20% exhibit clinically aggressive features, leading to considerable morbidity and death (25). WHO classification of meningiomas includes benign (grade I), atypical (grade II), and anaplastic (grade III) categories. Meningiomas were generally thought to progress from low-grade to high-grade tumors.
The most frequent cytogenetic abnormality is deletion of the long arm of chromosome 22 or monosomy 22, observed in approximately 50-80% of meningiomas (5, 26). In this study, loss of chromosome 22 was also the most common change, observed in 56.4% of cases. Cytogenetic and molecular studies have identified the NF2 tumor suppressor gene at 22q12.1 and its protein product, schwannomin/merlin (27). Further analysis revealed that the frequency of loss of chromosome 22 exceeds that of NF2 gene abnormalities (26, 27). This discrepancy of incidence has led to the search for a second tumor suppressor gene on 22q, including the BAM22 (28), LARGE (29), MN1 (30), and INI1 (31) genes.
The loss of chromosome 22 associated with other chromosomal aberrations occurs in over 60% of cases. In addition to the loss of one of sex chromosomes, chromosomes 1, 7, 12, 14, 17, 18, 19, and 20 are also frequent secondary abnormalities in meningiomas (6). By decreasing order of frequency, numeric or structural abnormalities of chromosomes 1, 20, X, 12, Y, 17, and 18 were observed in the current study, consistent with prior reports.
According to the CGAP site reports of pituitary adenoma (6), common cytogenetic results are largely diploid with gains of chromosomes 4, 7, 8, 9, 12, and 20, and losses of chromosomes 10, 14, 19, and 22. Only one of pituitary adenomas had abnormal karyotypes, loss of Y chromosome in this study. Its pathogenetic significance still needs further evaluation.
Schwannomas have also shown chromosomal abnormalities involving chromosome 22q (32). In this study, monosomy 22 was shown in three of nine (33.3%).
All patients with adenocarcinomas metastasized from stomach cancers were male and loss of the Y chromosome was noted. In a study of 37 adenocarcinomas in Barrett's esophagus and gastric cardia, loss of the Y chromosome seemed a prominent feature (33).
These cases including oligodendrogliomas, ependymomas, medulloblastomas, pituitary adenomas, schwannomas, and adenocarcinomas with abnormal karyotypes are too few for assessing any recurrent changes and clinical significances. However it is clear that karyotype complexity is far greater in high grade than in lower grades of CNS tumors, even in these types.
In conclusion, we describe cytogenetic results for 110 CNS tumors cultured and karyotyped successfully. Fifty-seven of 110 CNS tumors (51.8%) showed abnormal karyotypes. Common aberrations of chromosomes associated with oncogenes or tumor suppressor genes in the previous reports could be defined in the various type of CNS tumors. To the best of our knowledge, this is the first comprehensive cytogenetic study of CNS tumors in Korea. Abnormal karyotypes are more complex at high-grade tumors, suggesting that the karyotype reflects the biologic nature of the tumor and has clinically prognostic implications as WHO grade. The data presented in this study would be useful as a guide for further advanced molecular studies. More detailed cytogenetic and molecular characterizations of CNS tumors may contribute to better diagnostic criteria and deeper insights of tumorigenesis, eventually resulting in development of novel therapeutic strategies.
Figures and Tables
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005. 55:74–108.

2. Levin VA, Leibel SA, Gutin PH. DeVita VT, Hellman S, Rosenberg SA, editors. Neoplasms of the central nervous system. Cancer: Principles and Practice of Oncology. 2001. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2100–2160.
3. Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavenee WK. The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol. 2002. 61:215–225.

4. Kleihues P, Cavenee WK. World Health Organization Classification of tumors. Pathology and Genetics of Tumors of the Nervous System. 2000. Lyon: IARC Press.
5. Antinheimo J, Sallinen SL, Sallinen P, Haapasalo H, Helin H, Horelli-Kuitunen N, Wessman M, Sainio M, Jaaskelainen J, Carpen O. Genetic aberrations in sporadic and neurofibromatosis 2 (NF2)-associated schwannomas studied by comparative genomic hybridization (CGH). Acta Neurochir (Wien). 2000. 142:1099–1105.

6. Mitelman F, Johansson B, Mertens F, editors. Mitelman database of chromosome aberrations in cancer [Internet]. Updated February 16, 2007. Available from
http://cgap.nci.nih.gov/chromosomes
.
7. Shaffer LG, Tommerup N, editors. ISCN (2005): An International System for Human Cytogenetic Nomenclature. 2005. Basel: S. Karger.
8. Mitelman F, Johansson B, Mandahl N, Mertens F. Clinical significance of cytogenetic findings in solid tumors. Cancer Genet Cytogenet. 1997. 95:1–8.

9. Mertens F, Johansson B, Hoglund M, Mitelman F. Chromosomal imbalance maps of malignant solid tumors; a cytogenetic survey of 3185 neoplasms. Cancer Res. 1997. 57:2765–2780.
10. CBTRUS. Statistical report: primary brain tumors in the United States, 1998-2002. 2005. Central Brain Tumor Registry of the United States.
11. Bhattacharjee MB, Armstrong DD, Vogel H, Cooley LD. Cytogenetic analysis of 120 primary pediatric brain tumors and literature review. Cancer Genet Cytogenet. 1997. 97:39–53.

12. Koschny R, Koschny T, Froster UG, Krupp W, Zuber MA. Comparative genomic hybridization in glioma: a meta-analysis of 509 cases. Cancer Genet Cytogenet. 2002. 135:147–159.
13. Ichimura K, Ohgaki H, Kleihues P, Collins VP. Molecular pathogenesis of astrocytic tumours. J Neurooncol. 2004. 70:137–160.

14. Wessels PH, Twijnstra A, Kessels AG, Krijne-Kubat B, Theunissen PH, Ummelen MI, Ramaekers FC, Hopman AH. Gain of chromosome 7, as detected by in situ hybridization, strongly correlates with shorter survival in astrocytoma grade 2. Genes Chromosomes Cancer. 2002. 33:279–284.

15. Hirose Y, Aldape KD, Chang S, Lamborn K, Berger MS, Feuerstein BG. Grade II astrocytomas are subgrouped by chromosome aberrations. Cancer Genet Cytogenet. 2003. 142:1–7.

16. Reifenberger G, Ichimura K, Reifenberger J, Elkahloun AG, Meltzer PS, Collins VP. Refined mapping of 12q13-q15 amplicons in human malignant gliomas suggests CDK4/SAS and MDM2 as independent amplification targets. Cancer Res. 1996. 56:5141–5145.
17. Cowell JK, Matsui S, Wang YD, LaDuca J, Conroy J, McQuaid D, Nowak NJ. Application of bacterial artificial chromosome array-based comparative genomic hybridization and spectral karyotyping to the analysis of glioblastoma multiforme. Cancer Genet Cytogenet. 2004. 151:36–51.

18. Cianciulli AM, Morace E, Coletta AM, Occhipinti E, Gandolfo GM, Leonardo G, Carapella CM. Investigation of genetic alterations associated with development and adverse outcome in patients with astrocytic tumor. J Neurooncol. 2000. 48:95–101.
19. Arslantas A, Artan S, Oner U, Muslumanoglu H, Durmaz R, Cosan E, Atasoy MA, Basaran N, Tel E. The importance of genomic copy number changes in the prognosis of glioblastoma multiforme. Neurosurg Rev. 2004. 27:58–64.

20. Phuphanich S, Brat DJ, Olson JJ. Delivery systems and molecular targets of mechanism-based therapies for GBM. Expert Rev Neurother. 2004. 4:649–663.

21. Hill C, Hunter SB, Brat DJ. Genetic markers in glioblastoma: prognostic significance and future therapeutic implications. Adv Anat Pathol. 2003. 10:212–217.

22. Jeuken JW, Sprenger SH, Vermeer H, Kappelle AC, Boerman RH, Wesseling P. Chromosomal imbalances in primary oligodendroglial tumors and their recurrences: clues about malignant progression detected using comparative genomic hybridization. J Neurosurg. 2002. 96:559–564.

23. Teo C, Nakaji P, Symons P, Tobias V, Cohn R, Smee R. Ependymoma. Childs Nerv Syst. 2003. 19:270–285.

24. Biegel JA, Rorke LB, Janss AJ, Sutton LN, Parmiter AH. Isochromosome 17q demonstrated by interphase fluorescence in situ hybridization in primitive neuroectodermal tumours of the central nervous system. Genes Chromosomes Cancer. 1995. 14:85–96.
25. Perry A, Gutmann DH, Reifenberger G. Molecular pathogenesis of meningiomas. J Neurooncol. 2004. 70:183–202.

26. Carroll T, Maltby E, Brock I, Royds J, Timperley W, Jellinek D. Meningiomas, dicentric chromosomes, gliomas, and telomerase activity. J Pathol. 1999. 188:395–399.

27. Buckley PG, Jarbo C, Menzel U, Mathiesen T, Scott C, Gregory SG, Langford CF, Dumanski JP. Comprehensive DNA copy number profiling of meningioma using a chromosome 1 tiling path microarray identifies novel candidate tumor suppressor loci. Cancer Res. 2005. 65:2653–2661.

28. Peyrard M, Fransson I, Xie YG, Han FY, Ruttledge MH, Swahn S, Collins JE, Dunham I, Collins VP, Dumanski JP. Characterization of a new member of the human beta-adaptin gene family from chromosome 22q12, a candidate meningioma gene. Hum Mol Genet. 1994. 3:1393–1399.
29. Peyrard M, Seroussi E, Sandberg-Nordqvist AC, Xie YG, Han FY, Fransson I, Collins J, Dunham I, Kost-Alimova M, Imreh S, Dumanski JP. The human LARGE gene from 22q12.3-q13.1 is a new, distinct member of the glycosyltransferase gene family. Proc Natl Acad Sci USA. 1999. 96:598–603.

30. Lekanne Deprez RH, Riegman PH, Groen NA, Warringa UL, van Biezen NA, Molijn AC, Bootsma D, de Jong PJ, Menon AG, Kley NA, Seizinger BR, Zwarthoff EC. Cloning and characterization of MN1, a gene from chromosome 22q11, which is disrupted by a balanced translocation in a meningioma. Oncogene. 1995. 10:1521–1528.
31. Schmitz U, Mueller W, Weber M, Sévenet N, Delattre O, von Deimling A. INI1 mutations in meningiomas at a potential hotspot in exon 9. Br J Cancer. 2001. 84:199–201.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download