Abstract
Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) have been reported to be related to certain clinical characteristics (i.e., female, non-smokers with adenocarcinoma) and gefitinib responsiveness. This exploratory analysis was performed to determine the incidence of EGFR mutations in male smokers with squamous cell carcinoma, who were treated with EGFR tyrosine kinase inhibitor, gefitinib. Sixty-nine Korean NSCLC patients were treated with gefitinib in a prospective study. For a subset of 20 male patients with squamous cell carcinoma and a history of smoking, pretreatment tumor tissue samples were obtained and analyzed for EGFR mutations (exons 18 to 21). EGFR mutations were found in 3 (15%) patients, including in-frame deletions within exon 19 (n=2) and L858R missence mutation in exon 21 (n=1). These 3 patients with EGFR mutations responded to gefitinib, whereas only one of remaining 17 patients with wild-type EGFR achieved clinical response. Trend toward longer progression-free (5.8 vs. 2.4 months; P=0.07) was noted in patients with EGFR mutations compared to those with wild-type EGFR. Although male smokers with squamous cell carcinoma have not been considered ideal candidates for gefitinib treatment, significant incidence of EGFR mutations was observed. The molecular markers should be considered to predict clinical benefits from gefitinib.
There have been important advances within the last decade in the medical treatment of advanced non-small cell lung cancer (NSCLC). The current treatment guidelines have established two-drug combination chemotherapy as the standard of care for patients with advanced NSCLC (1). More recently, oncogenic genes have been explored as target molecules for cancer therapy. One example is the human epidermal growth factor receptor (EGFR). Based on the positive results of two randomized phase II trials (2, 3), the small molecule EGFR tyrosine kinase inhibitor gefitinib (Iressa®, Astra Zeneca Korea, Seoul, Korea) has been approved in Korea as second- or third-line therapy for advanced NSCLC after failure of standard platinum-based chemotherapy. In these early trials, the response rate ranged from 12% to 20%, and the median survival time was 7 to 8 months. Unfortunately, the promising results have not been confirmed by the subsequent phase III randomized trial in which gefitinib was compared with placebo (4).
Although gefitinib has been used in unselected patients with NSCLC, the clinical characteristics and molecular markers associated with clinical benefit have been identified. Considering the observations that EGFR tyrosine kinase inhibitors are effective in patients who have particular clinical or biological characteristics, appropriate patient selection based on these markers is one of the most extensively studied areas in clinical research. Clinical responses to gefitinib, and/or survival advantage, were seen in selected patient subsets (Asians with no smoking history and/or adenocarcinoma) (5). Furthermore, works have been conducted to identify possible molecular markers, including somatic mutations in the EGFR gene, EGFR gene amplification, and phosphorylation of the downstream EGFR effector proteins, that could be linked to gefitinib sensitivity or resistance, as well as the specific genotype variations that are harbored by different ethnicities (6). Years have passed since mutations of the EGFR tyrosine kinase domain were discovered in patients with NSCLC, and these patients had dramatic clinical responses to treatment with gefitinib. Mutations in the exons encoding the tyrosine kinase domains of EGFR, including in-frame deletions in exon 19 and a T-to-G substitution in exon 21 (L858R), have been found in a subset of lung adenocarcinoma (7-9). The majority of patients with these mutations exhibit durable clinical responses to EGFR tyrosine kinase inhibitor therapy. These EGFR mutations have been known to be found more frequently in patients with favorable clinical factors (5).
Accordingly, this exploratory analysis was performed to determine the incidence of EGFR mutations and the clinical outcome in male smokers with squamous cell carcinoma of the lung. The study population consisted of NSCLC patients who were treated with gefitinib as second- or third-line therapy.
This is a retrospective, exploratory analysis of the patients who were drawn from a prospective phase II clinical study, performed in Korean NSCLC patients. To enter the clinical study, patients were required to have histologically confirmed NSCLC that had failed after first-line chemotherapy for advanced disease. Patients had to be under 76 yr of age and they had to have an adequate performance status (0 to 2 according to the Eastern Cooperative Oncology Group [ECOG] scale), measurable lesion(s) and adequate organ function. They received gefitinib as second- or third-line therapy for their pretreated NSCLC. Patients were included for the current analysis if they were treated with gefitinib, if they were male smokers with squamous cell carcinoma, and if their paraffin-embedded tumor samples were available. At the time of analysis, there was no significant difference in survival between patients with and without EGFR mutation data.
The primary objective of this study was to determine the incidence of EGFR mutations in the specific subset of patients (Korean male smokers with squamous cell carcinoma of the lung) and their clinical outcomes (clinical response rate [RR], progression-free survival [PFS] and the overall survival [OS]). All the tumor samples were collected for routine histopathologic diagnosis before the start of therapy. All patients gave a written informed consent and the study was approved by the Gil Medical Center (Incheon, Korea) institutional review board. Patients were reassessed every 4 weeks by chest radiography and/or computed tomography, and the clinical responses were evaluated according to the Response Evaluation Criteria in Solid Tumor (RECIST) criteria (10).
EGFR mutation was determined according to previous reports (11, 12). Genomic DNA was prepared from formalin-fixed, paraffin-embedded sections of the tumor specimens. DNA was extracted, with using the QIAamp DNA Mini kit (Qiagen, Hilden, Germany), from five paraffin sections of 10 µm thickness containing a representative portion of each tumor block. Fifty nanograms of DNA were amplified in a 20 µL reaction solution containing 2 µL of 10×buffer (Roche, Mannheim, Germany), 1.7 to 2.5 mM/L of MgCl2, 0.3 µM of each primer pair (exon 18, F: 5'-tccaaatgagctggcaagtg, R: 5'-tcccaaacactcagtgaaacaaa; exon 19, F: 5'-atgtggcaccatctcacaattgcc, R: 5'-ccacacagcaaagcagaaactcac; exon 20, F: 5'-cattcatgcgtcttcacctg, R: 5'-catatccccatggcaaactc; exon 21, F: 5'-gctcagagcctggcatgaa, R: 5'-catcctcccctgcatgtgt), 250 µM of deoxynucleotide triphosphate, and 2.5 units of DNA polymerase (Roche). Amplifications were performed using a 5-min initial denaturation at 94℃; followed by 30 cycles of 1 min at 94℃, 1 min at 57℃, 1 min at 72℃, and a 10-min final extension step at 72℃ was done. The polymerase chain reaction (PCR) products were purified with a QIAgen gel extraction kit (Qiagen). DNA templates were then processed for the DNA sequencing reaction using the ABI-PRISM BigDye Terminator version 3.1 (Applied Biosystems, Foster, CA, U.S.A.) with both forward and reverse sequence-specific primers. Twenty nanograms of the purified PCR products were used in a 20 µL sequencing reaction solution that contained 8 µL of BigDye Terminator v3.1 and 0.1 µM of the same PCR primer. Sequencing reactions were performed using 25 cycles of 10 sec at 96℃, 5 sec at 50℃ and 4 min at 60℃. The sequence data was generated with the ABI PRISM 3100 DNA Analyzer (Applied Biosystems). The sequences were analyzed by Sequencer 3.1.1. software (Applied Biosystems) to compare the variations.
The clinical outcome variables in this analysis were RR, PFS and OS. The correlation between RR and EGFR mutations was evaluated by using chi-square test. PFS and OS were assessed by the Kaplan-Meier method. Log-rank test was used to compare PFS and OS between the patients with EGFR mutations and those with wild-type EGFR. All P values were two-sided, with P<0.05 indicating statistical significance.
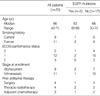
Of the 69 patients enrolled for the clinical study of gefitinib, there were 25 male smokers with squamous cell carcinoma, in whom, 20 patients provided tumor samples for DNA analysis. These 20 patients were treated with gefitinib as third-line therapy. Overall, EGFR mutations were found in 3 (15%) out of the 20 patients, including in-frame deletions within exon 19 (n=2) and L858R missence mutaion in exon 21 (n=1). The patient characteristics according to EGFR mutations are listed in Table 1. There was no statistically significant association between EGFR mutations and the clinical characteristics. Gefitinib was generally well-tolerated. One patient developed interstitial pneumonia after 4 months of therapy, which was recovered with discontinuing gefitinib. Salvage chemotherapy was offered to 8 patients after gefitinib failure: 7 patients received gemcitabine-based chemotherapy and one received pemetrexed.
Objective response was observed in 4 patients (20%). The 3 patients with EGFR mutations responded to gefitinib therapy, whereas only one of remaining 17 patients with wildtype EGFR achieved clinical response (100% vs. 6%, respectively; P<0.01). Besides wild-type EGFR, another possible factor associated with the lack of optimal response was performance status (27% for ECOG performance status 0-1 vs. 0% for ECOG performance status 2; P=0.25). With the median follow-up duration of 14.9 months (95% confidence interval [CI], 13.3-16.4 months), the median PFS and OS for all patients were 5.0 months (95% CI, 2.1-8.0 months) and 9.1 months (95% CI, 7.4-10.9 months), respectively. The estimated PFS was longer for the patients with EGFR mutations (median, 5.8 months vs. 2.4 months), but this difference was not statistically significant (P=0.07). OS was similar for patients with or without EGFR mutations (9.6 vs. 7.2 months, respectively; P=0.76).
In this small study, the incidence of EGFR mutations and the clinical outcome were evaluated in male smokers with squamous cell carcinoma of the lung who were treated with gefitinib as second-line or third-line therapy. As expected, the presence of EGFR mutations resulted in a significantly higher RR. Trends toward longer, although statistically insignificant, PFS was noted in patients with EGFR mutations compared to those with wild-type EGFR.
The incidence of EGFR mutations in this study (15%) was consistent with Western (13) and other Korean data (11, 12), although lower than that reported in the previous studies from Taiwan and Japan (14, 15). Our result should be interpreted with caution because it represents only a small group of patients with advanced NSCLC, and the patients had unfavorable clinical characteristic. However, it is indicated that male smokers with squamous cell carcinoma could present with EGFR mutations. All 3 patients with squamous cell carcinoma bearing EGFR mutations had partial responses to gefitinib therapy, whereas only one of the remaining 17 patients with wild-type EGFR achieved clinical response.
EGFR tyrosine kinase inhibitors expand and improve the treatments available for patients with NSCLC, although oncologists now have more factors to consider when prescribing therapy, particularly in the setting of second-line treatment where there are several new treatment options. In the Iressa Survival Evaluation in Lung Cancer (ISEL) trial that explored the efficacy of gefitinib compared with placebo in the second- or third-line therapy of advanced NSCLC, the overall survival benefit was not significant (4), although subsets of never-smokers and Asian patients had a significant survival benefit. In a phase III trial comparing erlotinib with placebo for the second-line or third-line therapy of advanced NSCLC (16), there was a pronounced survival benefit for never-smokers and the Asian patients.
Mutations in the EGFR gene are suggested to be associated with a high RR to EGFR tyrosine kinase inhibitors, irrespective of the clinical characteristics, and are prognostic for a favorable outcome, irrespective of therapy (17). EGFR mutations are thought to be more frequent in patients of an Asian origin and associated with improved survival in these patients. Yet predicting survival was not apparent in the phase II studies with gefitinib (18) and in the phase III study with another EGFR tyrosine kinase inhibitor erlotinib (19). The recent interest in EGFR mutations as a possible predictive factor for a response to gefitinib is largely derived from studies that have been performed in a retrospective fashion. Although EGFR mutations may be used to identify the patients who are most likely to benefit from EGFR tyrosine kinase inhibitors, they only identify a fraction of these patients. Moreover, the lack of a uniformly approved method for detecting EGFR mutations suggests that any conclusions must still be regarded as preliminary at best. While it was done retrospectively, our patients were selected from a prospective clinical study that was concerned with gefitinib treatment. The methods for detecting EGFR mutations were consistent with those described in the previous reports (11, 12). However, there were too few mutations to allow for meaningful comparisons with regard to the clinical characteristics or treatment outcomes. Because of the low incidence of EGFR mutations found in patients with NSCLC, its positive predictive value in selecting patients who would benefit from EGFR inhibitor therapy is limited.
At present, it is not possible to infer that patients with EGFR mutations may have a survival advantage because the prognosis of their disease is more favorable (17). We currently do not know how much of the improved clinical outcome of the patients harboring EGFR mutations is attributable to the gefitinib therapy or to the biology of the disease. Furthermore, such molecular markers as EGFR mutations would be cumbersome to routinely evaluate in clinical practice and their prognostic value has not been validated in prospective trials. Decisions to commence therapy with EGFR tyrosine kinase inhibitors often depend on the clinical characteristics or performance status (20).
Our analysis clearly shows that the clinical characteristics are not perfect in determining the responsiveness of patients to EGFR tyrosine kinase inhibitors, although they are important. In addition, we question the validity of selecting patients who would benefit from gefitinib solely based on the clinical factors. Selection of patients in such a manner would lead to inappropriate avoidance of patients who would otherwise be benefited from gefitinib. Although male smokers with squamous cell carcinoma have not been considered ideal candidates for treatment with gefitinib, significant incidence of EGFR mutations was observed in this specific patient subset. While clinical characteristics can be applied as a predictive factor for determining the response to gefitinib in patients with advanced NSCLC, it seems apparent that those molecular markers should also be considered to effectively predict the clinical benefit from gefitinib.
Figures and Tables
References
1. Pfister DG, Johnson DH, Azzoli CG, Sause W, Smith TJ, Baker S Jr, Olak J, Stover D, Strawn JR, Turrisi AT, Somerfield MR. American Society of Clinical Oncology treatment of unresectable non-small-cell lung cancer guideline: update 2003. J Clin Oncol. 2004. 22:330–353.

2. Fukuoka M, Yano S, Giaccone G, Tamura T, Nakagawa K, Douillard JY, Nishiwaki Y, Vansteenkiste J, Kudoh S, Rischin D, Eek R, Horai T, Noda K, Takata I, Smit E, Averbuch S, Macleod A, Feyereislova A, Dong RP, Baselga J. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial) [corrected]. J Clin Oncol. 2003. 21:2237–2246.
3. Kris MG, Natale RB, Herbst RS, Lynch TJ Jr, Prager D, Belani CP, Schiller JH, Kelly K, Spiridonidis H, Sandler A, Albain KS, Cella D, Wolf MK, Averbuch SD, Ochs JJ, Kay AC. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA. 2003. 290:2149–2158.
4. Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, Thongprasert S, Tan EH, Pemberton K, Archer V, Carroll K. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet. 2005. 366:1527–1537.

5. Park K, Goto K. A review of the benefit-risk profile of gefitinib in Asian patients with advanced non-small-cell lung cancer. Curr Med Res Opin. 2006. 22:561–573.

6. Shah NT, Kris MG, Pao W, Tyson LB, Pizzo BM, Heinemann MH, Ben-Porat L, Sachs DL, Heelan RT, Miller VA. Practical management of patients with non-small-cell lung cancer treated with gefitinib. J Clin Oncol. 2005. 23:165–174.

7. Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004. 350:2129–2139.

8. Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004. 304:1497–1500.

9. Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, Mardis E, Kupfer D, Wilson R, Kris M, Varmus H. EGF receptor gene mutations are common in lung cancers from "never smokers" and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A. 2004. 101:13306–13311.

10. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. European Organization for Research and Treatment of Cancer. National Cancer Institute of the United States. National Cancer Institute of Canada. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000. 92:205–216.

11. Han SW, Kim TY, Hwang PG, Jeong S, Kim J, Choi IS, Oh DY, Kim JH, Kim DW, Chung DH, Im SA, Kim YT, Lee JS, Heo DS, Bang YJ, Kim NK. Predictive and prognostic impact of epidermal growth factor receptor mutation in non-small-cell lung cancer patients treated with gefitinib. J Clin Oncol. 2005. 23:2493–2501.

12. Han SW, Kim TY, Lee KH, Hwang PG, Jeon YK, Oh DY, Lee SH, Kim DW, Im SA, Chung DH, Heo DS, Bang YJ. Clinical predictors versus epidermal growth factor receptor mutation in gefitinib-treated non-small-cell lung cancer patients. Lung Cancer. 2006. 54:201–207.

13. Bell DW, Lynch TJ, Haserlat SM, Harris PL, Okimoto RA, Brannigan BW, Sgroi DC, Muir B, Riemenschneider MJ, Iacona RB, Krebs AD, Johnson DH, Giaccone G, Herbst RS, Manegold C, Fukuoka M, Kris MG, Baselga J, Ochs JS, Haber DA. Epidermal growth factor receptor mutations and gene amplification in non-small-cell lung cancer: molecular analysis of the IDEAL/INTACT gefitinib trials. J Clin Oncol. 2005. 23:8081–8092.

14. Chou TY, Chiu CH, Li LH, Hsiao CY, Tzen CY, Chang KT, Chen YM, Perng RP, Tsai SF, Tsai CM. Mutation in the tyrosine kinase domain of epidermal growth factor receptor is a predictive and prognostic factor for gefitinib treatment in patients with non-small cell lung cancer. Clin Cancer Res. 2005. 11:3750–3757.

15. Satouchi M, Negoro S, Funada Y, Urata Y, Shimada T, Yoshimura S, Kotani Y, Sakuma T, Watanabe H, Adachi S, Takada Y, Yatabe Y, Mitsudomi T. Predictive factors associated with prolonged survival in patients with advanced non-small-cell lung cancer (NSCLC) treated with gefitinib. Br J Cancer. 2007. 96:1191–1196.

16. Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S, Smylie M, Martins R, van Kooten M, Dediu M, Findlay B, Tu D, Johnston D, Bezjak A, Clark G, Santabarbara P, Seymour L. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005. 353:123–132.

17. Eberhard DA, Johnson BE, Amler LC, Goddard AD, Heldens SL, Herbst RS, Ince WL, Janne PA, Januario T, Johnson DH, Klein P, Miller VA, Ostland MA, Ramies DA, Sebisanovic D, Stinson JA, Zhang YR, Seshagiri S, Hillan KJ. Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J Clin Oncol. 2005. 23:5900–5909.

18. Cappuzzo F, Hirsch FR, Rossi E, Bartolini S, Ceresoli GL, Bemis L, Haney J, Witta S, Danenberg K, Domenichini I, Ludovini V, Magrini E, Gregorc V, Doglioni C, Sidoni A, Tonato M, Franklin WA, Crino L, Bunn PA Jr, Varella-Garcia M. Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst. 2005. 97:643–655.

19. Tsao MS, Sakurada A, Cutz JC, Zhu CQ, Kamel-Reid S, Squire J, Lorimer I, Zhang T, Liu N, Daneshmand M, Marrano P, da Cunha Santos G, Lagarde A, Richardson F, Seymour L, Whitehead M, Ding K, Pater J, Shepherd FA. Erlotinib in lung cancer-molecular and clinical predictors of outcome. N Engl J Med. 2005. 353:133–144.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download