Abstract
Despite advances in surgical techniques and instrumentation, current intra-operative estimations of acetabular version in total hip arthroplasty are of limited accuracy. In the present study, two experienced orthopedic surgeons compared intra-operatively measured (using portable imaging) anteversions and vertical inclinations of acetabular components with those measured using standardized radiographs post-operatively in 40 patients. Of the all vertical inclinations measured from intra-operative radiographs, 72.5% (n=29) were within ±2°, and 97.5% (n=39) were within ±5° of those determined using post-operative radiographs, and for anteversion, 52.5% (n=21) were within ±2°, and 97.5% (n=39) were within ±5°. Post-operative radiographs demonstrated that 90.0% (n=36) of vertical inclinations and anteversions were within the adequate zone. Obviously, our method has its limitations, but the authors conclude that the method described in this article better allows surgeons to verify acetabular version intra-operatively. In particular, the described method is suitable in cases with a deformed acetabular anatomy and difficult revision surgery.
It is widely accepted that acetabular component positioning is one of the most important success factors of total hip arthroplasty (1). Despite the many improvements that have been made in terms of the manufacture and design of ceramic implants, the ease with which ceramic component fractures occur is disappointing. Impingement of the femoral neck on the edge of the acetabular component is a well recognized mechanism of acetabular component fracture, and thus, the achievements of correct degrees of anteversion and vertical inclination of the acetabular component are more critical for ceramic-on-ceramic total hip arthroplasty than for polyethylene liner total hip arthroplasty (2). However, the intra-operative estimation of acetabular version in total hip arthroplasty is of limited accuracy and little information is available concerning the accuracy of component placement during the procedure. Thus, the purpose of this study was to evaluate whether portable radiographs enable surgeons to assess acetabular cup version intra-operatively.
A picture archiving communication system (PACS; PiViewSTAR, Infinitt, Seoul, Korea) has been available at our hospital since March 2004. After its installation, intra-operative radiographs became readily available and measurements of angles in radiographs could be performed easily and accurately. Accordingly, we retrospectively reviewed the radiographs of 40 patients who underwent cementless total hip arthroplasty (including one case of acetabular revision only) from March 2004 to December 2006. Radiographs that demonstrated a marked pelvic obliquity in pelvic anteroposterior (AP) view were excluded. There were 25 male and 15 female patients, and mean patient age at index operation was 54 yr (range, 31-86 yr) (Table 1). Patients were fitted with one of two acetabular components from one company (VerSys, Zimmer, Warsaw, IN, U.S.A.), i.e., Trilogy AB (ceramic on ceramic articulation) or Trilogy (metal on polyethylene [PE] articulation). Twenty nine cases underwent ceramic on ceramic total hip arthroplasty and 11 metal on PE total hip arthroplasty.
A posterolateral surgical approach was adopted in all cases, with the patient firmly anchored in a lateral decubitus position on the operating table. To achieve an adequate position, we sometimes estimated the bilateral symmetry of the obturator foramen in pelvic AP view using a C-arm image intensifier. During surgery, an alignment guide rod was used to determine the correct vertical inclination and anteversion of the acetabular prosthesis. Two surgeons specifically recruited for this study were asked to measure vertical inclinations and anteversions of acetabular cups using the intra-operative portable AP and lateral (Lat) views; these were later compared with post-operative standard radiographs. Beneath the operating table at our hospital, there is a space for inserting an radiography cassette to obtain a hip Lat. view before operation. Thus, in each patient, after acetabular cup insertion had been achieved, a portable hip Lat. view was taken. Subsequently, both hip portable AP views were taken; we refer to these as initial portable radiographs. When surgeons did not achieve a satisfactory acetabular cup position according to initial portable radiographs, the acetabular cup concerned was extracted, reinserted, and its position rechecked, and when the position of an acetabular cup was agreed, we refer to these as the confirmed portable radiograph. Final post-operative radiographs are referred to as post-operative standard radiographs. The method used to obtain the intra-operative portable Lat. view differed from that used to obtain a postoperative Lat. view. Specifically, post-operative views were taken in the supine position and intra-operative views were taken in the lateral position. On portable Lat. view, an imaginary elliptical orbit and a line passing through the long axis of the elliptical orbit were drawn, and the angle between this line and the vertical line drawn from the surface of the earth was defined as anteversion (Fig. 1). Even though there are some argues about definition of an anteversion, we used plain radiographs to measure anteversion in the present study. Vertical inclination was defined as the angle between the line joining the ischial tuberosities and the line through the long axis of the cup (Fig. 2). In the present study, we defined an adequate zone of vertical inclination as between 30° and 50° and an adequate zone of anteversion as between 5° and 30°. These ranges taken from the literature (3), but the maximum anteversion angle set at 5° greater than literature value due to Korean life style. Inter-obsever correlations were evaluated using the intraclass correlation coefficients (ICC), which provide a measure of the degree of agreement among raters. ICCs range between 0.0 and 1.0, and a higher score indicates better agreement.
Differences between intra-operative and post-operative measurements of vertical inclination and anteversion were determined. For all measured vertical angles in intra-operative radiographs, 72.5% (n=29) were within ±2° of post-operative standard radiographs, 97.5% (n=39) were within ±5°, and 2.5% (n=1) were over ±5° (Fig. 3). In terms of anteversion, 52.5% (n=21) were within ±2°, and 97.5% (n=39) were within ±5° of values in post-operative standard radiographs (Fig. 4). Among the safe cases (n=37, 92.5%) confirmed in portable radiographs for vertical inclination, one case was found to be inadequate in post-operative standard radiographs. In terms of anteversion, 95% (n=38) of cases had an adequate confirmed portable radiograph and two cases of them had an inadequate in post-operative standard radiograph. Finally, post-operative standard radiographs demonstrated that 90% (n=36) of vertical inclinations and anteversions were within the adequate zone (Table 2). The mean inter-observer correlation between the two orthopedic surgeons was 0.96 and ranged from 0.73 to 0.98 (Table 3).
Accurate positioning of the femoral and acetabular components is important for successful total hip arthroplasty (1). Correct component orientation is vital to prevent dislocation, reduce component wear, and provide a maximum range of motion (3-8). Moreover, these factors all contribute to arthroplasty survival and longevity and have significant implications on long-term clinical and economic outcomes of total hip arthroplasty. The importance of adequate acetabular cup positioning was emphasized after ceramic-on-ceramic articulations were introduced in total hip arthroplasty. According to Hassan et al. (7), despite advances in material manufacturing, concerns about component fracture remain. These workers found that impingement of the femoral neck on the edge of the acetabular component can cause acetabular component failure. Thus, acetabular cups must be oriented in an optimal cup position to minimize this risk of impingement. However, one practical problem encountered is that sockets tend to revert when total hip arthroplasty is performed through a posterolateral approach. This is usually caused by inadequate anterior retraction of the femur, which forces the acetabular positioning device posteriorly during component insertion. Moreover, during cup fixing (particularly in terms of anteversion) the surgeon must be able to judge the position of the pelvis in both horizontal and vertical planes. Furthermore, errors associated with patient positioning on the operating table are a common cause of acetabular malpositioning, and although several jigs and guide rods have been devised to determine proper positioning, these instruments are not fool proof. Rather, they should be viewed as crude measuring devices that are subject to errors associated with patient positioning. Nonetheless, it is not uncommon for an orthopedic surgeon to be surprised by acetabular anteversion discrepancies shown by true lateral films obtained during follow up. Thus, despite the popularity of total hip arthroplasty, intra-operative estimations of acetabular version are of limited accuracy, and furthermore, little information is available concerning the accuracy of component placement. Several investigators have introduced techniques for measuring anteversion and vertical inclination on radiographs. The first such study in total hip arthroplasty was conducted by McLaren, who used the wire ring in the Charnley-Muller prosthesis to calculate version (9). However, despite the presumed reliabilities of intra-operative assessments of vertical inclination and anteversion using the alignment guide, 42% of cups were still found to be outside the safe zone, as defined by Lewinnek et al. (3). In addition, Wines and McNicol (10) found that only 45% of acetabular components were within the expected clinical version range. In a study by Hassan et al. (7), vertical inclination was found to be reasonably assessable during surgery, but anteversion could not be accurately assessed during surgery, even using the alignment guide. In 1987, Cohn et al. (11) described a new technique for the intra-operative determination of acetabular anteversion using a plastic overlay. According to this study, obtaining a true lateral view of the hip intra-operatively is difficult, but overlays on easily obtained AP views allow the accurate assessments of degrees of anteversion. In this previous study, difficulty was encountered identifying the apex of the acetabular cup ellipse when measuring the acetabular anteversion angle, and this was particularly evident at higher degrees of version when the apex was more rounded. Moreover, although plain pelvic AP view can show some degree of acetabular cup rotation, it does not differentiate retroversion and anteversion. Thus, Cohn recommended that surgeons should not solely rely on this method, but rather use it to help verify acetabular position in difficult cases, when the anatomy is significantly distorted. It was also recommended that a radiograph in a second plane must be taken. Our method was driven by the necessity for a lateral view to determine the direction of version. According to our study, of all measured vertical inclinations in intra-operative radiographs 97.5% were within ±5° as compared with post-operative standard radiographs, and in terms of anteversion, 52.5% were within ±2°, and 97.5% were within ±5°. Moreover, post-operative radiographs demonstrated that 90.0% of anteversions were within the adequate zone. Even though, some cases were found to be beyond the adequate range by post-operative radiography, we consider that the errors observed during this study fell into the clinically acceptable during follow up. When vertical inclination and anteversion were compared individually, intra-operative assessments of vertical inclination were found to be more reliable than those of anteversion, which occurs with the results of Hassan et al. Interestingly, one case in the present study showed 9° of retroversion in the initial portable radiograph, and the author extracted and reinserted the cup. Finally, the cup was positioned 16° anteverted (Fig. 5). It should be borne in mind that the detection of the retroverted state in AP. view is sometimes so difficult, in the present study, only lateral view visualized an inadequately retroverted position. It is evident that our method is not without shortcomings, as changes in pelvis flexion/extension will alter acetabular version, and thus, we do not consider that our method is routinely recommendable in normal cases. However, the combination of intra-operative AP and Lat views can allow surgeons to assess acetabular version intra-operatively. In particular, we recommend the described method in cases with a deformed acetabular anatomy and for difficult revision surgery.
Figures and Tables
 | Fig. 1The angle between the line passing through the long axis of the imaginary elliptical orbit and a vertical line from the bottom was defined as the angle of anteversion in intra-operative portable Lat view. |
 | Fig. 2The angle between the line joining the ischial tuberosities and the line through the long axis of the acetabular cup was defined as the angle of vertical inclination in a portable pelvic AP view. |
 | Fig. 3Points represent vertical inclination differences between final post-operative standard radiographs and confirmed portable radiographs for each cup.
F.I, Final Inclination; C.P.I, Confirmed Portable Inclination.
|
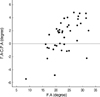 | Fig. 4Points represent anteversion differences between final post-operative and confirmed portable radiographs for each cup.
F.A, Final Anteversion; C.P.A, Confirmed Portable Anteversion.
|
References
1. Garcia-Cimbrelo E, Munuera L. Dislocation in low-friction arthroplasty. J Arthroplasty. 1992. 7:149–155.
2. Ha YC, Kim SY, Kim HJ, Yoo JJ, Koo KH. Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasty. Clin Orthop Relat Res. 2007. 458:106–110.

3. Lewinnek GE, Lewis JL, Tarr R, compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978. 60:217–220.

4. Carlsson AS, Gentz CF. Postoperative dislocation in the Charnley and Brunswik total hip arthroplasty. Clin Orthop Relat Res. 1977. 125:177–182.

5. D'Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000. 82:315–321.
6. Eftekhar NS. Dislocation and instability complicating low friction arthroplasty of the hip joint. Clin Orthop Relat Res. 1976. 121:120–125.

7. Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998. 13:80–84.

8. Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999. 14:509–513.

10. Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006. 21:696–701.

11. Cohn BT, Katz MM, Krackow KA, Lennox DW, Loeb P. A new technique for the intraoperative determination of acetabular anteversion. Orthopedics. 1987. 10:1565–1566.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download