Abstract
We herein describe a case of cystic lymphangioma in the greater omentum of the remnant stomach, which is thought it to be related with subtotal gastrectomy 10 yr ago for early gastric cancer. A 76-yr-old man was admitted to our department with postprandial abdominal discomfort and bowel habit change. Intraabdominal multilocular cystic mass was detected by ultrasonography and computed tomography. We performed a complete En-bloc tumor resection including spleen and distal pancreas, and histological examination confirmed cystic lymphangioma originated from the greater omentum of the remnant stomach. Although the etiology of omental lymphangioma remains largely unclear, these findings suggested strongly that obstruction of the lymphatic vessels after gastric resection for gastric carcinoma might be the most plausible cause. The surgical extirpation with resection of organs involved appears to be a treatment of choice for such unusual case.
Lymphangiomas are rare benign tumors, and are located preferentially in head, neck, and axilla in children. However, lymphangiomas in abdomen are extremely rare, particularly in adults. Of all the lymphangiomas in the peritoneal cavity, about 70% of them have been found in the mesentery of small intestine. This report describes a case of omental cystic lymphangioma of the stomach associated with earlier subtotal gastrectomy for gastric cancer.
A 76-yr-old man who presented with an 8-month history of postprandial abdominal discomfort and bowel habits change was referred from a local clinic, because of a huge intraabdominal cystic lesion on abdominal computed tomographic (CT) scan. According to his medical history, he underwent subtotal gastrectomy (Billroth II operation) 10 yr ago for early gastric cancer at St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea. A non-tender left upper quadrant abdominal mass was palpated on physical examination. Laboratory data, including tumor markers, were unremarkable. Gastrointestinal endoscopic examination revealed no local recurrence at the previous gastrojejunostomy anastomosis or intraluminal pathologic lesion. An abdominal computed tomography showed about 12×15 cm sized non-enhancing cystic mass, suspicious of a cystic neoplasm of pancreas, mesenteric cyst, or omental lymphangioma (Fig. 1).
On October 31, 2003, the patient underwent exploration which showed no evidence of ascites, peritoneal dissemination, or metastasis in abdominal cavity. During exploration and resection, the cystic tumor was found not to involve mesentery of the colon, remnant stomach and retroperitoneum, however, technically complete removal of the tumor without resection of distal pancreas and spleen was not feasible. Therefore, Enbloc resection of the cystic tumor with the greater omentum, distal pancreas and spleen with no spillage of cystic fluid was performed. After resection, cystic tumor was grossly measured 16.5×12.0×3.5 cm, but the attached distal pancreas and spleen were grossly unremarkable (Fig. 2). The encapsulated cystic mass had a pinkish smooth external surface attached with distal pancreas and spleen in continuity, and cut sections showed grayish white, trabeculated, and glistening in the inner cut surface of multilocular cyst. The cyst was filled with strawberry colored serous fluid, the thickness of cystic wall was measured less than 0.1 cm, and there was no solid area. Histologically, the cystic wall consisted of a fibroconnective tissue accompanied by dilated lymphatic spaces of varying sizes and lymphoid cell aggregations in the endothelial lining of lymphatic vessels, and there was no evidence of recurrence or metastasis from gastric cancer. Immunohistochemical stainings showed positive for CD31 and smooth muscle actin (SMA) (Fig. 3). These findings were consistent with a diagnosis of cystic lymphangioma. The patient had an uneventful postoperative course, and no evidence of recurrence had also been found in a 3-yr follow-up period.
Cystic lymphangioma is a rare congenital malformation of the lymphatics which is found predominantly in children, and abdominal lymphangioma is far more extremely rare, especially in adult population (1-5). Although the etiology remains unclear, lymphangioma is thought to be due to a developmental failure and possible lymphatic obstruction followed by the inflammation of lymphatic channels (1-5).
Cystic lymphangiomas can be located in any part of the body except the brain, and they are most frequently a single cyst and also affect a single organ (2, 5). The tumors are usually located in the neck (75%), axilla (20%), and other part of the body (4-5%) (2, 5), and less than 1% of lymphangiomas affect the mesentery, greater omentum, and retroperitoneum (5).
Abdominal lymphangiomas can occur at any age and most are asymptomatic. In adults, symptoms and signs are commonly insidious in onset rather than acute (1, 2, 4-6).
It is important to distinguish cystic lymphangioma from other cystic neoplasms such as mesenteric cyst, peritoneal mesothelioma, and retroperitoneal cystic neoplasm. Histologically, lymphangioma is characterized by a flat epithelial endothelium and a wall containing alternatively lymphoid tissue, small lymphatic spaces, smooth muscle, and foam cells (5-7). Furthermore, this endothelial lining and stroma cells are usually stained positively with anti-factor VIII-related antigen or anti-CD 31 by immunohistochemistry (7, 8).
The treatment of choice is complete resection to yield a cure for this benign lesion, but resectability depends on its size, location, and adhesions or invasions to vital structures (1-6). In the present case, En-bloc resection of cystic tumor with distal pancreatectomy and splenectomy was indicated because this huge neoplasm could be a malignant tumor and a possible local recurrence if the resection was incomplete.
In English-written literatures, cystic lymphangiomas arising from the omentum have mostly been described as congenital primary lesions, and some secondary lesions concurrently with other primary tumors have also been reported. To the best of our knowledge, this could be the first case report of an acquired intraabdominal cystic lymphangioma arising from the greater omentum, associated with earlier gastric resection for gastric cancer.
In general, during subtotal gastrectomy for distal gastric cancer, the greater omentum at the high body and around the spleen is not indicated for dissection and resection. In the present case, as described above in the operative findings, cystic lymphangioma was thought to originated from the remnant greater omentum after incomplete omentectomy in the previous subtotal gastrectomy for distal gastric carcinoma. Long standing lymphatic obstruction and stasis during the past 10 yr after subtotal gastrectomy is strongly suggested as the pathophysiologic predisposing factor to the development of this unusual case.
Figures and Tables
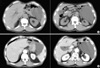 | Fig. 1An abdominal CT scan showed about 12.0×15.0 cm sized non-enhancing cystic mass in the left abdominal cavity. This mass was attached to pancreas body and tail superomedially, and displaced a remnant of stomach medially, spleen laterally, and adjacent bowel loops inferomedially. This cystic mass contained internal septum, like structure in the upper aspect of tumor. |
 | Fig. 2Gross specimen showed an encapsulated cystic tumor combined with distal pancreas and spleen (A, Anterior view; B, Posterior view). |
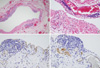 | Fig. 3Histology of lymphangioma. (A, B) Cystic wall was consisted of fibroconnective tissue accompanied by dilated lymphatic spaces and lymphoid cell aggregations in the endothelial lining of lymphatic vessels (H&E ×100, ×400). Immunohistochemical staining. (C) Positive for CD31 in the lining cells of dilated lymphatic vessels (×400). (D) Positive for SMA in the cystic wall, and they were smooth muscle bundles surrounding lymphatic vascular endothelium (×400). |
References
1. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intraabdominal cystic lymphangiomas. Arch Surg. 1985. 120:1266–1269.

2. Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989. 76:485–489.

3. Fonkalsrud EW. Congenital malformations of the lymphatic system. Semin Pediatr Surg. 1994. 3:62–69.
4. de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg. 1998. 85:395–397.

5. Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003. 196:598–603.

6. Allen JG, Riall TS, Cameron JL, Askin FB, Hruban RH, Campbell KA. Abdominal lymphangiomas in adults. J Gastrointest Surg. 2006. 10:746–751.

7. Chung JH, Suh YL, Park IA, Jang JJ, Chi JG, Kim YI, Kim WH. A pathologic study of abdominal lymphangiomas. J Korean Med Sci. 1999. 14:257–262.

8. Miettinen M, Lindenmayer AE, Chaubal A. Endothelial cell markers cd31, cd34, and bnh9 antibody to h- and y-antigens--evaluation of their specificity and sensitivity in the diagnosis of vascular tumors and comparison with von willebrand factor. Mod Pathol. 1994. 7:82–90.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download