Abstract
Phlebosclerotic colitis is a rare form of ischemic colitis characterized by the thickening of the wall of the affected colon due to fibrous degeneration of submucosal layer of colon and fibrotic obstruction of the colono-mesenteric vein, resulting in the disturbance of venous return from the colon. The pathogenic mechanism of this entity remains unknown but chronic liver disease with portal hypertension is maybe thought to be one of the speculated mechanisms. Here we first report the case of surgically confirmed phlebosclerotic colitis, that was in the early stage but showed the aggressive nature, in a 61-yr-old cirrhotic patients with portal hypertension in Korea.
Phlebosclerotic colitis, a rare disease entity of ischemic colitis, is known to be characterized by the thickening of the colonic wall due to fibrotic sclerosis of the colono-mesenteric vein and fibrous degeneration of the submucosal layer of involved colon, resulting in the disturbed venous return from the colon (1, 2). The pathophysiologic mechanism of this disease remains unclear although several reports have suggested that it might be related to portal hypertension secondary to liver cirrhosis or other chronic liver diseases (2, 3). The diagnosis is usually achieved to be based on a combination of radiologic, endoscopic, and histologic findings along with clinical manifestations. There are several cases about this disease entity those have been reported in authorized medical journals around the world but rare in Korea (4-11). Here we report the first case of phlebosclerotic colitis confirmed surgically in a 61-yr-old cirrhotic patient with portal hypertension in Korea.
A 61-yr-old man was admitted to hospital because of right lower quadrant abdominal pain and bloody stool for one month. He had a medical history of regular follow-up for alcoholic liver cirrhosis since four years ago. He had experienced the endoscopic histoacryl injection sclerotherapy for gastric varix with bleeding eight months ago. At the time of admission, physical examination revealed tenderness of the right lower abdomen but no rebound tenderness. Laboratory tests showed a white blood cell count of 2,990/µL, hemoglobin of 11.6 g/dL, platelet count of 119,000/µL, but there were no other abnormal findings in the blood chemistry with liver tests, electrolytes, and prothrombin time. Tumor markers such as alpha-fetoprotein, carcinoembryogenic antigen (CEA), and CA19-9 were within normal limit.
A colonoscopy revealed multiple, geographic, and circumferential ulcerations in the distal ascending and transverse colon and could not get through further proximal portion of ascending colon due to luminal narrowing with fibrotic stenosis (Fig. 1A). Endoscopic biopsy showed ulcerative inflammation without malignant cells. The tests for cytomegalovirus and tuberculosis in biopsy specimens were negative. A follow-up colonoscopy performed one month later showed still remained multiple ulcerations in the transverse colon. The ascending colon was not observed because of no more further advance of endoscopy due to marked stenosis (Fig. 1B).
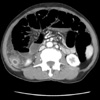
Abdominal computed tomography (CT) demonstrated cirrhotic liver with splenomegaly and multiple porto-systemic venous collaterals. The proximal to mid ascending colon were thick-walled with increased density in the surrounding fatty tissue and diffuse vascular engorgement (Fig. 2A). No definite calcification in the thickened wall and vessels was identified. Virtual CT colonography showed marked luminal narrowing with shortening of ascending colon (Fig. 2B).
Superior mesenteric angiography revealed no occlusion of main branch at arterial phase, but indicated venous pooling along the ascending colon at the delayed phase (Fig. 3).
The right lower abdominal pain of the patient was progressively worsening even though the conservative treatments with total parenteral nutrition for 10 days after admission. His abdomen was markedly distended and showed distinct tenderness with rebound tenderness. Finally, the marked dilatation of small bowel caused by colonic obstruction was observed on CT scan (Fig. 4) and the passage of stool was not identified.
A right hemicolectomy was performed because of the colonic obstruction. Gross findings of operation specimen showed approximately 7×5 cm sized ulcerating mass-like wall thickening of the cecum and the proximal ascending colon (Fig. 5A). Microscopic examination showed chronic ulcerative inflammation, fibrous degeneration of the submucosal layer, and thickening of the venous wall in the mesentery with no evidence of malignancy (Fig. 5B-D).
On the basis of these radiologic, endoscopic, and histologic findings mentioned above, we diagnosed as a phlebosclerotic colitis occurred during regular follow-up of cirrhotic patients with portal hypertension. Until now, eight months after right hemicolectomy, the patient is being followed in the status of compensated liver cirrhosis without any gastrointestinal symptoms.
Phlebosclerotic colitis, first coined by Yao et al. in 2000 (6), is a rare type of ischemic colitis and has different clinicopathologic presentations from the classic type of ischemic colitis. While ischemic colitis is usually caused by insufficient perfusion of mesenteric arterial blood flow and involves left side colon, especially hepatic flexure or sigmoid regions where are known to be watershed area within the colonic blood supply, phlebosclerotic colitis occurs when sclerotic obstruction of veins in the colonic wall and adjacent mesentery produces chronic congestion of affected colon, and involves the right hemicolon preferentially (5-8). The present case also shows the typical manifestations of phlebosclerotic colitis such as fibrous thickening of affected colono-mesenteric vein and wall thickening of right hemicolon. The pathogenesis of this disease still remains unknown, but there are several clinical conditions, diabetes mellitus, hyperlipidemia, cardiac disease, angiitis, CREST syndrome, Churg-Strauss syndrome, lymphocytic phlebitis and portal hypertension, those might be related to phlebosclerotic colitis (6, 12-15). In the presented case, underlying disease of the patient was alcoholic liver cirrhosis with obvious portal hypertension. In Korea, to our knowledge, a similar case has been reported previously as a term of idiopathic mesenteric phlebosclerosis (11), first described by Iwashita et al. in 2003 (12), known to be a synonym of phlebosclerotic colitis.
Clinical symptoms include abdominal pain and bloody diarrhea, as our case presented, nausea, vomiting, constipation and ileus, and depend on the severity of the disease (16). Although this disease usually has long duration of illness indicating chronic nature of the disease, progression to mechanical ileus resulting from intestinal obstruction is not common. Surgical intervention, as we did in our case, is not usually necessary unless intestinal obstruction, perforation or massive bleeding occur as postischemic complications (8, 12).
Colonoscopy usually reveals dark purple and edematous mucosa, erosion, ulceration and luminal narrowing. Saito et al. (4) endoscopically observed a patient of phlebosclerotic colitis for three years and considered deep circumferential ulceration on colonoscopy as the aggressive nature of this disease. In our case, the first colonoscopy showed multiple circumferential ulcerations and luminal narrowing, and could not get through the lesion due to stenosis and fibrosis, which have been worsening in the follow-up colonoscopic finding one month later. We believe these findings suggest as the aggressive form of phlebosclerotic colitis.
The imaging findings of phlebosclerotic colitis are as follow (1, 4-6): multiple thread-like or linear calcifications mainly along the right hemicolon on plain radiographs of abdomen; thickening of the affected colonic wall with calcification of intramural and mesenteric veins on CT scans; haustral disappearance, luminal irregularities, rigidity, narrowing, and thumb-printing on barium enema; and venous pooling and obstruction of the affected colonic wall with dilated collateral flow on angiography (1, 5). In the present case, contrast-enhanced dynamic CT, virtual CT colonography and superior mesenteric angiography also showed typical radiologic features of phlebosclerotic colitis those were described above, except calcification of involved colonic and adjacent mesenteric veins.
Histopathologic characteristics include, macroscopically, dark brown appearance of the right hemicolon and thickening of the colonic wall, and microscopically, thickening of the venous walls and tortuous veins, fibrotic degeneration of the venous walls with calcifications and markedly fibrous thickening in the submucosa of colonic wall (6). Recently, Kusanagi et al. (2) considered calcification of the venous wall to increase gradually over the time and reported the case without definite calcification of the venous wall on radiologic and histologic finding as the early stage of phlebosclerotic colitis. In this case, microscopy revealed submucosal fibrosis of the colonic wall and thickening of venous wall in the mesentery without calcification. It is considered that this change was induced by ischemic colitis due to disturbance in venous return from the colonic wall associated with portal hypertension.
Here we report the first case of surgically confirmed phlebosclerotic colitis, that was in the early stage but showed the aggressive nature, in cirrhotic patients with portal hypertension in Korea.
Figures and Tables
Fig. 1
A colonoscopy revealed multiple circumferential ulcerations in the distal ascending and transverse colon (A), and the follow-up colonoscopy performed one month later showed still remained multiple ulcerations in the transverse colon and the scope could not get through the further proximal portion of ascending colon due to stenosis and fibrosis (B).

Fig. 2
Abdominal CT disclosed thickening of the wall of the ascending colon with surrounding fatty infiltration and diffuse vascular engorgement (A). Virtual CT colonography showed marked luminal narrowing with shortening of ascending colon (B).

Fig. 3
Superior mesenteric angiography revealed no occlusion of main branch at arterial phase (A), and indicated venous pooling (arrows) along the ascending colon at the delayed phase (B).

Fig. 5
Macroscopic examination showed a huge ulcerating mass-like lesion (dotted circle) at the cecum and the proximal ascending colon measuring about 7×5 cm with colonic wall thickening (A). Microscopic examination showed fibrous thickening (arrow) of the mesenteric vein (B) (H&E, ×200), (C) prominent neurovascular bundles and eosinophilic inflammation in submucosa (arrows) (H&E, ×40), and (D) chronic ulcerative inflammation (H&E, ×100) with no evidence of malignancy.

References
2. Kusanagi M, Matsui O, Kawashima H, Gabata T, Ida M, Abo H, Isse K. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005. 185:441–447.

3. Kimura Y, Kashima K, Daa T, Tou Y, Hanzawa K, Nakayama I, Yokoyama S. Phlebosclerotic colitis coincident with carcinoma in adenoma. Pathol Int. 2003. 53:721–725.

4. Saito Y, Taniguchi M, Tagawa K, Ibukuro K, Mori M, Emura F. Phlebosclerotic colitis with deep circumferential ulceration: three-year endoscopic follow-up. Report of a case. Dis Colon Rectum. 2005. 48:2347–2351.

5. Oshitani N, Matsumura Y, Kono M, Tamori A, Higuchi K, Matsumoto T, Seki S, Arakawa T. Asymptomatic chronic intestinal ischemia caused by idiopathic phlebosclerosis of mesenteric vein. Dig Dis Sci. 2002. 47:2711–2714.
6. Yao T, Iwashita A, Hoashi T, Matsui T, Sakurai T, Arima S, Ono H, Schlemper RJ. Phlebosclerotic colitis: value of radiography in diagnosis-report of three cases. Radiology. 2000. 214:188–192.

7. Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005. 184:1584–1586.

9. Maruyama Y, Watanabe F, Kanaoka S, Kanamaru H, Yoshino G, Koda K, Hanai H, Kaneko E, Kinou I. A case of phlebosclerotic ischemic colitis: a distinct entity. Endoscopy. 1997. 29:334.

10. Hoshino Y, Matsumoto R, Takasaki T, Nagahara H, Shiratori K. Education and imaging. Gastrointestinal: phlebosclerotic colitis. J Gastroenterol Hepatol. 2008. 23:670.
11. Jung HG, Koh JW, Lee MY. A case of idiopathic mesenteric phlebosclerosis. Korean J Gastroentrol. 2008. 52:261–264.
12. Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003. 46:209–220.
13. Ikehata A, Hiwatashi N, Kawarada H, Yamazaki H, Ito K, Kinouchi Y, Kimura M, Noguchi M, Maekawa H, Suzuki H, Shimada T, Yamagata J, Toyota T. Chronic ischemic colitis associated with marked calcifications of the mesenteric vessels - report of two cases. Dig Endosc. 1994. 6:355–364.
14. Modigliani R, Muschart JM, Galian A, Clauvel JP, Piel-Desruisseaux JL. Allergic granulomatous vasculitis (Churg-Strauss Syndrome). Report of a case with widespread digestive involvement. Dig Dis Sci. 1981. 26:264–270.
15. Saraga EP, Costa J. Idiopathic entero-colic lymphocytic phlebitis. A cause of ischemic intestinal necrosis. Am J Surg Pathol. 1989. 13:303–308.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download