Abstract
We investigated the correlation between Cyclooxygenase-2 (COX-2) expression and the tumor response in patients with cervical cancer that were treated with curative radiotherapy (RT). Fifty-seven patients with squamous cell carcinoma were treated with concurrent radiochemotherapy (CRCT, n=29) or RT alone (n=28). The response of each patient was evaluated by three serial Magnetic Resonance Imaging examinations: before the start of RT, at four weeks after the start of RT (mid-RT) and at four weeks after the completion of RT (post-RT). Forty-three patients had positive COX-2 expression. The COX-2 negative patients achieved a higher rate of complete response (CR) at mid-RT than did the COX-2 positive patients (28.6% vs. 7.0%, P=0.054), but not at post-RT (64.3% vs. 69.8%). The initial tumor volume was a significant predictor of CR at mid-RT (P=0.003) and post-RT (P=0.004). The multivariate analysis showed that the initial tumor volume (at mid-RT and post-RT) and CRCT (at post-RT) were significant predictors of CR; however, the COX-2 expression was not. In conclusion, the COX-2 expression status has no significant correlation with the tumor response. Further studies on the changes in COX-2 expression levels during RT may be helpful for determination of its role in the tumor response to treatment and patient prognosis.
Cyclooxygenase-2 (COX-2) has been associated with the biology of tumors including carcinogenesis, inhibition of apoptosis, proliferation, promotion of angiogenesis, enhanced invasiveness, immune modulation, and increased mutagenesis (1, 2). Clinical studies have shown that COX-2 overexpression might be related to the extent of tumors at diagnosis and treatment outcomes of several cancers (3-12). In addition, COX-2 overexpression has been reported to shorten the disease-free and overall survival after radiation therapy (RT) in patients with cervical cancer (7, 8, 10). Recently, COX-2 overexpression has been reported to reduce the tumor response to RT in esophageal cancer, cervical cancer and rectal cancer (13-16). Inhibitory effect of COX-2 on apoptosis is thought to be the cause of the reduced response rate in such cases.
In squamous cell carcinoma (SCC) of the uterine cervix, COX-2 overexpression has been reported to have an adverse effect on tumor response in two studies (14, 16); however, the relationship between COX-2 expression and tumor response remains to be elucidated. In these studies, the methods for evaluation of the tumor response after RT were not described, and possible confounding factors such as tumor volume were not analyzed. Traditional methods including gynecological examination or computerized tomography scanning have limitations with regard to the evaluation of responses; they cannot exactly determine alterations in the extent of tumors. However, assessment of tumors using magnetic resonance imaging (MRI) could offer more accurate and objective information compared to clinical evaluations (17).
In this study, we used MRI to evaluate the tumor response to RT, and investigated the correlation between COX-2 expression and tumor response in patients with SCC of the uterine cervix treated with RT.
We enrolled 57 patients treated with curative radiotherapy for SCC of the uterine cervix from 1997 to 2004 at Samsung Medical Center. All patients had three serial MRIs performed before, during and after radiotherapy and had an available paraffin block sample for immunohistochemical staining. The patient's age range was from 34 to 83 yr with a median age of 61 yr. The number of patients with FIGO stages I, II, III, and IV was 7, 33, 12, and 5, respectively. Lymph node metastasis was suspected in the pelvis in 29 patients and the paraaortic region in five patients. The mean tumor size was 4.8 cm (range 1.2-8.2 cm).
All patients were treated with external beam RT plus intracavitary brachytherapy (ICR). The external beam RT was performed with a 15-MV photon delivered daily in 1.8 Gy, five fractions per week. Whole-pelvic external irradiation was given up to a dose of 39.6 Gy (for stage IB or IIA) or 45 Gy (for stage IIB, III, and IV), and then midline shielding was used. The total dose delivered to the parametrium ranged from 45 Gy to 66.6 Gy (median 50.4 Gy). Patients with paraaortic lymph node metastasis were treated with extended pelvic RT, including the paraaortic lymph node region up to 45 Gy. High dose rate ICR using an 192Ir source was used to deliver a total dose of 24 Gy at point A with six insertions, two fractions per week.
Twenty-nine patients (50.9%) received concurrent radiochemotherapy (CRCT). Eighteen patients were given concurrent and adjuvant chemotherapy including cisplatin (60 mg/m2) plus 5-fluorouracil (1,000 mg/m2 in a continuous infusion over 96 hr) every three weeks; a median of three cycles was administered (range 1-6 cycles). Eleven patients were given weekly cisplatin (30 mg/m2) concurrently with RT. The median overall treatment time for all patients was 55 days (range 37-85 days).
The patients underwent three serial MRI examinations within four weeks before the start of RT (pre-RT), at four weeks after the start of RT (mid-RT) and at four weeks after the completion of RT (post-RT). The tumor volume of each MRI examination was calculated by multiplying the sum of the areas by the slice thickness of T2-weighted axial or sagittal images using the Picture Archiving Communication System (General Electric Medical Systems, Milwaukee, WI, U.S.A.). The mid-RT and post-RT responses were classified into four categories: complete response (CR) was the complete disappearance of the primary cervical tumor, partial response was a reduction of 50% or more in the pretreatment volume of the primary cervical tumor; stable disease was a reduction of less than 50% or an increase of less than 25%; progressive disease was an increase of 25% or more.
Immunohiostochemical staining was performed with a COX-2 monoclonal antibody (Cayman Chemical, Ann Arbor, MI, U.S.A.). Two pathologists analyzed the immunostaining without knowledge of the patient outcome. They evaluated the slides based on the percentage of tumor cells stained as follows: 0, totally negative; 1, <10% reactive; 2, 10-50% reactive; 3, >50% reactive. Scores 0 and 1 were regarded as negative and scores 2 and 3 as positive. Cases with discordant results were discussed until a consensus was reached (Fig. 1).
The correlations between patient characteristics and COX-2 expression were evaluated by the Fisher's exact test. The relationships between variables and tumor response at mid-RT and post-RT were evaluated by the same method. The generalized estimating equation was used to verify the significance of the change of the CR rate from mid-RT to post-RT according to the treatment modality. In addition, we used the multiple logistic regression analysis to evaluate significant predictors of CR at mid-RT and post-RT. P values of less than 0.05 were considered statistically significant. All statistical analyses were performed with the SAS® System (SAS 8.0, SAS Institute Inc., Cary, NC, U.S.A.).
The mean tumor volume of all patients at pre-RT, mid-RT and post-RT was 58 mL (range 1.1-166.4 mL), 15.6 mL (range 0-132.6 mL) and 14.2 mL (range 0-96.8 mL), respectively. Seven patients (12.3%) achieved CR at mid-RT and 39 patients (68.4%) at post-RT.
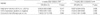
COX-2 expression was positive in 43 patients (75.4%). COX-2 expression was not related to age, hemoglobin level, initial tumor volume, the FIGO stage or treatment modality (Table 1). Evaluation based on the initial tumor size showed that COX-2 positive cases were more common in patients with larger tumors (>4 cm); however, the difference was marginally significant (P=0.059).
At mid-RT, CR was more common in COX-2 negative patients than in COX-2 positive patients (28.6% vs. 7.0%, respectively) but the correlation was marginally significant (P=0.054). At post-RT, CR was achieved in 64.3% of COX-2 negative patients and in 69.8% of COX-2 positive patients (P=0.747).
Table 2 shows the relationship between COX-2 expression and tumor response according to the initial tumor volume or treatment modality. For patients with a small pretreatment tumor volume (≤32 mL), the COX-2 negative tumors tended to achieve a higher rate of CR at mid-RT than COX-2 positive tumors (P=0.057); however, there was no difference in the CR rate at post-RT. In patients who received RT alone, COX-2 negative tumors achieved a significantly higher rate of CR than did COX-2 positive tumors at mid-RT (44.4% vs. 5.3%, P=0.026); however, this was not observed at post-RT. The tumor response was related to COX-2 expression in neither patients with a large pretreatment tumor volume (>32 mL) nor the CRCT group.
Tables 3, 4 show the relationship between the variables and tumor response during and after RT. Patients with a small pretreatment tumor volume achieved a higher rate of CR both at mid-RT (33.3% for ≤32 mL vs. 2.6% for >32 mL, P=0.003) and at post-RT (94.4% for ≤32 mL vs. 56.4% for >32 mL, P=0.005). Patients with a small pretreatment tumor size achieved similar results at mid-RT (P=0.006) but not at post-RT.
According to the treatment modalities, the CR rate was not different at mid-RT and post-RT. However, the CR rate increased more in the CRCT group from 6.9% at mid-RT to 75.9% at post-RT than in the RT alone group from 17.9% to 60.7%; these findings were marginally significant (P=0.057).
The multivariate analysis revealed that the initial tumor volume and concurrent chemotherapy were significant predictors of CR at mid-RT and post-RT (Table 5). Tumors with an initial volume >32 mL had a lower probability of CR at mid-RT (odds ratio [OR]=0.052; 95% confidence interval [CI], 0.005-0.588) and post-RT (OR=0.037; 95% CI, 0.004-0.379) compared to those with an initial volume ≤32 mL. The patients treated with CRCT had a greater probability of CR at post-RT than did those treated with RT alone (OR=4.152; 95% CI, 1.081-15.948). The COX-2 expression status was not related to tumor response.
The tumor volume prior to RT is a known prognostic factor for cervical cancer, but Gong et al. (18) confirmed an exponential relationship between tumor regression rates (TRR) and time regardless of the tumor volume by estimating TRR during external beam RT with serial MRI. They suggested that tumors with a small pretreatment volume have a higher probability of early disappearance after RT. We also found that small volume tumors achieved a higher rate of CR at mid-RT and post-RT compared to large volume tumors.
Currently, chemotherapy is used concurrently with RT to improve the treatment results for patients with locally advanced cervical cancer (19, 20). Ohara et al. (21) investigated the difference of TRR according to the treatment modality (CRCT vs. RT alone) by fitting an exponential regression equation to the respective curve of each patient. Although TRR was not significantly different between the CRCT group (median, 0.032 per day) and the RT alone group (median, 0.024 per day), rapid TRR (>0.05 per day) was more common in the CRCT group. In addition, TRR for large tumors (>5 cm in diameter) was greater in the CRCT group. In a randomized trial reported by Keys et al. (22), the rate of residual disease in hysterectomy specimens at three to six weeks after treatment was lower in the CRCT group compared to the RT alone group. In our study, the CR rate was not different according to the use of chemotherapy. However, the initial tumor volume of the CRCT group was significantly larger than that of the RT alone group (average 70.9 mL vs. 44.6 mL, P=0.034). Therefore, we analyzed the extent of change of the CR rate from mid-RT to after-RT, and the increase of the CR rate was prominent in the CRCT group. The CR rate at post-RT was higher in the CRCT group than in the RT alone group where the CR rate was higher at mid-RT. It is therefore reasonable to conclude that chemotherapy accelerated the tumor response to RT.
COX-2 overexpression has been accepted as an independent prognostic factor for recurrence and survival in patients with cervical cancer (7, 8, 10). Kim et al. (8) reported that the 5-yr overall and disease free survival was worse in COX-2 positive patients than in COX-2 negative patients, and COX-2 overexpression was the only significant prognostic factor in the multivariate analysis. Chen et al. (10) also reported similar results. COX-2 overexpression was related to a reduced tumor response to radiotherapy in esophageal and rectal cancer (13, 15). For SCC of the esophagus, COX-2 negative patients achieved a higher CR rate after preoperative radiochemotherapy (60% vs. 0%, P=0.01); however, this result is limited by the small number of patients and confounding factors affecting tumor response. In rectal cancer, COX-2 overexpression in pretreatment biopsies was related to a poor response to neoadjuvant radiochemotherapy (P=0.026) (15).
Two studies investigating the correlation between COX-2 overexpression and complete remission after RT have been reported in patients with uterine cervical cancer (14, 16). Kim et al. (14) reported that all COX-2 negative patients achieved a CR; however, 83% of COX-2 positive patients with SCC and 68% of those with adenocarcinoma achieved a CR (P<0.001). Ishikawa et al. (16) found that COX-2 overexpression before RT was related to reduced apoptosis after 9 Gy, and tumors without COX-2 overexpression achieved a higher rate of CR after RT although this was not statistically significant (80% vs. 59%, P=0.12). In our study, multiple logistic regression analysis showed that the COX-2 status was not a predictive factor of a CR. Although the COX-2 status seemed to be correlated with tumor response in some selected subgroups, the tumors that achieved a CR, at mid-RT, were significantly smaller than the tumors that did not achieve a CR (10.5±14.1 mL vs. 64.6±46.5 mL, P<0.001), Furthermore, COX-2 negative tumors, in the small volume group and RT alone group, were significantly smaller than COX-2 positive tumors in each of the subgroups. This could have caused COX-2 overexpression to be misinterpreted as a significant predictor of the tumor response. However, we cannot conclude that COX-2 does not have influence on tumor response to radiotherapy on the basis of our study results due to the retrospective study design and potential for selection bias.
Although there is no data on the change of COX-2 protein expression during radiotherapy in patients with cervical cancer, COX-2 protein expression increased after single or fractionated irradiation in PC-3 cells in vitro (23, 24), and after radiotherapy for rectal cancer patients in vivo (25-29). For the patients with rectal cancer treated with preoperative radiotherapy, with or without chemotherapy, the distribution of COX-2 positive tumors or the intensity of COX-2 protein expression increased, and even the tumors without COX-2 expression newly expressed the COX-2 protein. One study reported that the initial COX-2 expression was not correlated with tumor regression (28). However, another study reported that the intensity of COX-2 protein expression, after radiochemotherapy, was inversely correlated with tumor regression (29). Therefore, COX-2 protein expression in patients with cervical cancer might also increase during radiotherapy. Investigation of the change in COX-2 expression levels during RT, by repeated biopsies, might be indicated to determine the relationship between COX-2 expression and the tumor response.
In conclusion, the results of this study show no correlation between the pretreatment COX-2 expression status and the tumor response. However, the COX-2 expression status is known as an important prognostic factor in patients with cervical cancer based on previous studies. Therefore, further studies are needed to clarify the alteration of COX-2 expression levels during RT to determine its association with the tumor response to treatment and patient prognosis
Figures and Tables
Fig. 1
Immunohistochemical staining of COX-2. (A) negative (<10% of distribution of immunoreactivity), (B) positive (≥10% of distribution of immunoreactivity) (original magnification ×200).

References
1. Choy H, Milas L. Enhancing radiotherapy with cyclooxygenase-2 enzyme inhibitors: a rational advance? J Natl Cancer Inst. 2003. 95:1440–1452.

2. Kanaoka S, Takai T, Yoshida K. Cyclooxygenase-2 and tumor biology. Adv Clin Chem. 2007. 43:59–78.

3. Fujita T, Matsui M, Takaku K, Uetake H, Ichikawa W, Taketo MM, Sugihara K. Size- and invasion-dependent increase in cyclooxygenase 2 levels in human colorectal carcinomas. Cancer Res. 1998. 58:4823–4826.
4. Murata H, Kawano S, Tsuji S, Tsuji M, Sawaoka H, Kimura Y, Shiozaki H, Hori M. Cyclooxygenase-2 overexpression enhances lymphatic invasion and metastasis in human gastric carcinoma. Am J Gastroenterol. 1999. 94:451–455.

5. Sheehan KM, Sheahan K, O'Donoghue DP, MacSweeney F, Conroy RM, Fitzgerald DJ, Murray FE. The relationship between cyclooxygenase-2 expression and colorectal cancer. JAMA. 1999. 282:1254–1257.

6. Ryu HS, Chang KH, Yang HW, Kim MS, Kwon HC, Oh KS. High cyclooxygenase-2 expression in stage IB cervical cancer with lymph node metastasis or parametrial invasion. Gynecol Oncol. 2000. 76:320–325.

7. Gaffney DK, Holden J, Zempolich K, Murphy KJ, Dicker AP, Dodson M. Elevated COX-2 expression in cervical carcinoma: reduced cause-specific survival and pelvic control. Am J Clin Oncol. 2001. 24:443–446.
8. Kim YB, Kim GE, Cho NH, Pyo HR, Shim SJ, Chang SK, Park HC, Suh CO, Park TK, Kim BS. Overexpression of cyclooxygenase-2 is associated with a poor prognosis in patients with squamous cell carcinoma of the uterine cervix treated with radiation and concurrent chemotherapy. Cancer. 2002. 95:531–539.

9. Nix P, Lind M, Greenman J, Stafford N, Cawkwell L. Expression of Cox-2 protein in radioresistant laryngeal cancer. Ann Oncol. 2004. 15:797–801.

10. Chen HH, Su WC, Chou CY, Guo HR, Ho SY, Que J, Lee WY. Increased expression of nitric oxide synthase and cyclooxygenase-2 is associated with poor survival in cervical cancer treated with radiotherapy. Int J Radiat Oncol Biol Phys. 2005. 63:1093–1100.

11. Khor LY, Bae K, Pollack A, Hammond ME, Grignon DJ, Venkatesan VM, Rosenthal SA, Ritter MA, Sandler HM, Hanks GE, Shipley WU, Dicker AP. COX-2 expression predicts prostate-cancer outcome: analysis of data from the RTOG 92-02 trial. Lancet Oncol. 2007. 8:912–920.

12. Yoshikawa R, Fujiwara Y, Koishi K, Kojima S, Matsumoto T, Yanagi H, Yamamura T, Hashimoto-Tamaoki T, Nishigami T, Tsujimura T. Cyclooxygenase-2 expression after preoperative chemoradiotherapy correlates with more frequent esophageal cancer recurrence. World J Gastroenterol. 2007. 13:2283–2288.

13. Kulke MH, Odze RD, Mueller JD, Wang H, Redston M, Bertagnolli MM. Prognostic significance of vascular endothelial growth factor and cyclooxygenase 2 expression in patients receiving preoperative chemoradiation for esophageal cancer. J Thorac Cardiovasc Surg. 2004. 127:1579–1586.

14. Kim YB, Kim GE, Pyo HR, Cho NH, Keum KC, Lee CG, Seong J, Suh CO, Park TK. Differential cyclooxygenase-2 expression in squamous cell carcinoma and adenocarcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 2004. 60:822–829.

15. Smith FM, Reynolds JV, Kay EW, Crotty P, Murphy JO, Hollywood D, Gaffney EF, Stephens RB, Kennedy MJ. COX-2 overexpression in pretreatment biopsies predicts response of rectal cancers to neoadjuvant radiochemotherapy. Int J Radiat Oncol Biol Phys. 2006. 64:466–472.

16. Ishikawa H, Ohno T, Kato S, Wakatsuki M, Iwakawa M, Ohta T, Imai T, Mitsuhashi N, Noda SE, Nakano T, Tsujii H. Cyclooxygenase-2 impairs treatment effects of radiotherapy for cervical cancer by inhibition of radiation-induced apoptosis. Int J Radiat Oncol Biol Phys. 2006. 66:1347–1355.

17. Narayan K, McKenzie A, Fisher R, Susil B, Jobling T, Bernshaw D. Estimation of tumor volume in cervical cancer by magnetic resonance imaging. Am J Clin Oncol. 2003. 26:e163–e168.

18. Gong QY, Tan LT, Romaniuk CS, Jones B, Brunt JN, Roberts N. Determination of tumour regression rates during radiotherapy for cervical carcinoma by serial MRI: comparison of two measurement techniques and examination of intraobserver and interobserver variability. Br J Radiol. 1999. 72:62–72.

19. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, Rotman M, Gershenson DM, Mutch DG. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.

20. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, Clarke-Pearson DL, Insalaco S. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.

21. Ohara K, Tanaka YO, Tsunoda H, Oki A, Satoh T, Onishi K, Kagei K, Sugahara S, Hata M, Igaki H, Tokuuye K, Akine Y, Yoshikawa H. Preliminary estimation of treatment effect on uterine cervical squamous cell carcinoma in terms of tumor regression rate: comparison between chemoradiotherapy and radiotherapy alone. Radiat Med. 2005. 23:25–29.
22. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, Walker JL, Gersell D. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999. 340:1154–1161.

23. Steinauer KK, Gibbs I, Ning S, French JN, Armstrong J, Knox SJ. Radiation induces upregulation of cyclooxygenase-2 (COX-2) protein in PC-3 cells. Int J Radiat Oncol Biol Phys. 2000. 48:325–328.

24. Ohneseit PA, Krebiehl G, Dittmann K, Kehlbach R, Rodemann HP. Inhibition of cyclooxygenase-2 activity by celecoxib does not lead to radiosensitization of human prostate cancer cells in vitro. Radiother Oncol. 2007. 82:229–238.

25. Watwe V, Javle M, Lawrence D, Groth J, Iyer R, El-Hajjar D, Geradts J. Cyclooxygenase-2 (COX-2) levels before and after chemother apy: a study in rectal cancer. Am J Clin Oncol. 2005. 28:560–564.
26. Debucquoy A, Goethals L, Geboes K, Roels S, McBride WH, Haustermans K. Molecular responses of rectal cancer to preoperative chemoradiation. Radiother Oncol. 2006. 80:172–177.

27. Kobayashi H, Hashiguchi Y, Ueno H, Shinto E, Kajiwara Y, Mochizuki H. Absence of cyclooxygenase-2 protein expression is a predictor of tumor regression in rectal cancer treated with preoperative short-term chemoradiotherapy. Dis Colon Rectum. 2007. 50:1354–1362.

28. Bouzourene H, Yan P, Sandmeier D, Zouhair A, Matter M, Vuilleumier H, Coucke P. The role of COX-2 in rectal cancer treated with preoperative radiotherapy. Virchows Arch. 2008. 452:499–505.

29. Debucquoy A, Libbrecht L, Roobrouck V, Goethals L, McBride W, Haustermans K. Morphological features and molecular markers in rectal cancer from 95 patients included in the European Organisation for Research and Treatment of Cancer 22921 trial: prognostic value and effects of preoperative radio (chemo) therapy. Eur J Cancer. 2008. 44:791–797.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download