Abstract
To investigate the gender difference of early symptoms appearing before the onset of the psychotic symptoms in patients with first-episode schizophrenia, we reviewed the medical records of 63 patients (38 males, 25 females), who were hospitalized for first-episode schizophrenia. The frequency and duration of prodromal and psychotic symptoms, Clinical Global Impression scale scores, Global Assessment of Functioning (GAF) scale scores at admission, and other clinical characteristics were recorded for all patients. Overall, the most common prodromal symptoms were attenuated positive symptoms (89%), followed by mood symptoms (86%). Negative symptoms were the most common in male patients (97.4%), whereas attenuated positive symptoms were the most common in female patients (84%). Male patients demonstrated more frequent negative, cognitive, and obsessive-compulsive symptoms than female patients did and also showed a tendency of having negative symptoms for the longer period. Correlational analysis showed a significant negative correlation between the duration of negative symptoms and GAF scores at admission in male patients. Our findings suggest that different patterns of prodromal symptoms between male and female begin before the onset of the psychosis. Further prospective studies should be needed.
Recently, the focus of management in schizophrenia has been shifting to early detection and intervention of the disorder. The primary prevention is to eliminate etiological risk factors or to strengthen individual resistibility to the morbid risk; however, these have not been shown to be effective in schizophrenia to date. Instead, many researchers have been interested in secondary early intervention, which is preventing or postponing the onset of psychosis, reducing the severity of illness, and enhancing treatment outcomes.
During the past decade, clinical studies on first-episode schizophrenia have revealed that the duration of untreated psychosis (DUP) may be associated with short-term and/or long-term outcomes, that is, a longer DUP is associated with a poorer outcome of schizophrenia (1, 2). Also, according to McGorry et al. (3), early therapeutic intervention during the prodromal phase of schizophrenia may influence the overall course of the disease. The onset of psychotic symptoms observed in schizophrenia is frequently preceded by nonspecific changes in behavior, emotional state, and/or cognitive state (4), with common signs and symptoms of the prepsychotic stage of schizophrenia including sleep disturbance, anxiety, anger/irritability, depressed mood, deterioration in functioning, social withdrawal, poor concentration, suspiciousness, loss of motivation, and low energy (5, 6). Therefore, it is critical that these signs and symptoms should be detected as early as possible to reduce the duration of the prodromal phase.
There have been studies about the sex differences in the manifestation of schizophrenia. According to Goldstein and Lewine (7), males with schizophrenia generally have an earlier onset of illness and a more severe form of the disease as reflected in greater cognitive or social impairment, while female patients are more likely to suffer from anxiety and affective symptoms (8). This sexual difference is regarded as a consequence of different neuroendocrine and affective arousal systems (9). Thus, the early symptoms and signs experienced and observed during the prodromal stage of schizophrenia may differ between males and females with regard to their frequency and relationship with other clinical characteristics. However, relatively little work examined the gender difference of clinical manifestation in this population (10), although several prospective studies examined gender as a predictive variable of conversion to psychosis and found mixed results (11, 12). Therefore, in the present study, we examined gender differences in the prodromal symptoms experienced by the patients or observed by caregivers before the onset of first psychotic symptoms in patients with first-episode schizophrenia. We hypothesized more affective symptoms in women and more cognitive or negative symptoms in men would be found during prodromal phase, as in patients with schizophrenia in previous studies.
This study was performed according to regulations on the use of human subjects established by the institutional review board of Seoul National University Hospital. We reviewed the medical records of all patients admitted to the psychiatric inpatient ward between March 2005 and February 2007 in Seoul National University Hospital whose diagnoses at the time of discharge were schizophrenia.
Subjects included in the study met the following criteria. First, the admission records were complete with detailed present illness including all past psychiatric diagnoses, tentative DSM-IV multi-axial diagnoses, Clinical Global Impression (CGI) and Global Assessment of Functioning (GAF) scores. Second, the discharge records were complete with definite DSM-IV multi-axial diagnoses, CGI and GAF scores, and signed by at least two psychiatrists. Third, the patients had experienced either delusions or hallucinations for at least 1 month, regardless of the subtypes of schizophrenia they were diagnosed with. Fourth, from previous medical records, it was evident that patients had never been diagnosed with schizophrenia before the admission.
The authors discarded cases in which the section for present illness lacked the evidence for the DSM-IV diagnosis of schizophrenia, estimated onset of noticeable symptoms, or CGI and GAF scores. The subjects either had never taken psychotropic medication or had received pharmacotherapy for less than 1 month. Patients who met the criteria for substance use disorder, mental retardation, or major general medical conditions associated with psychotic symptoms were also excluded from the study.
A total of 214 patients were admitted during the study period and received a diagnosis of schizophrenia on discharge. Among them, 63 patients (38 males, 25 females) met these criteria. All had been admitted under the mental health act with the permission of at least one eligible caregiver. The numbers of subjects diagnosed with each subtype of schizophrenia were as follows: paranoid (n=46), undifferentiated (n=12), disorganized (n=4), and catatonic (n=1). Thirty-nine patients (25 males, 14 females) had been treated with psychotropic medication such as antipsychotics, antidepressants, and benzodiazepines. The duration of pharmacotherapy did not exceed 1 month in any of them.
The onsets of the prodromal phase and the psychotic phase were estimated to the nearest 1 month according to the admission and discharge records by one of the authors. The onset of the prodromal phase was defined as the appearance of the first symptoms noticeable either to the patient him/herself or to the caregiver(s) that were considered to indicate the appearance of the disease. The duration from the onset of prodromal symptom to the onset of psychotic symptom was considered as the duration of prodromal symptom. The onset of the psychotic phase was defined as the appearance of active psychotic symptoms. In this study, prodromal symptoms were categorized into 7 dimensions as follows: 1) attenuated positive symptoms (unusual thought content, suspiciousness, unusual perceptual experiences, and disorganized speech), 2) negative symptoms (social withdrawal, decreased energy, and flat affect), 3) cognitive changes (difficulties with concentration and memory problems), 4) mood symptoms (depression, elation, and irritability), 5) anxiety, 6) obsessive compulsive symptoms, and 7) somatic symptoms. These dimensions were derived from the Instrument for the Retrospective Assessment of Onset of Schizophrenia (13) and Criteria of Prodromal Syndrome (14). The presence of symptoms from each dimension was determined 1) if the symptom dimension was directly mentioned in the medical record either in English or Korean, i.e, for dimension of mood symptoms, phrases such as "mood disturbance", "depression (or depressive mood)", "elation (or elated mood)", "irritability" or their Korean equivalents or 2) if the authors could conclude the presence of symptoms from each dimension from the description of the subjects??thought, emotion and behavior from the medical record.
Differences in the frequency of prodromal symptoms between male and female patients were analyzed using a chi-square test. Clinical characteristics or duration of overall and individual prodromal symptoms were compared between male and female patients using a t-test. Correlational analysis was used to examine the relationships between the duration of prodromal and/or psychotic symptoms and, CGI or GAF scale score at admission in each gender. All analyses were two-tailed, and significance was established at P<0.05
The mean age of the study population was 24.66±5.62 yr. The duration of prodromal symptoms and psychotic symptoms were 5.63±4.53 yr and 0.82±1.07 yr, respectively. On average, patients were admitted for 34.57±25.53 days. At admission, mean CGI score and GAF scores were 5.71±0.58 and 35.08±12.33, respectively.
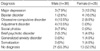
A total of 17 males had axis I psychiatric diagnoses, including obsessive-compulsive disorder (OCD), adjustment disorder, social phobia, and major depression, prior to the onset of psychotic symptoms, whereas 12 females had prior axis I diagnoses, including bipolar disorder, major depression, and OCD before the onset of psychotic symptoms (Table 1).
As shown in Table 2, no significant differences were detected between genders in terms of age, age of onset, duration of psychotic symptoms before admission, duration of admission, as well as CGI and GAF scores.
Fig. 1 shows the frequencies of the prodromal symptoms in male and female patients. Overall, the most common symptoms were attenuated positive symptoms (89%) and mood symptoms (86%). However, the most common symptoms in males were negative symptoms (97.4%), whereas the most common in females were attenuated positive symptoms (84%). Significant differences were observed in the frequency of negative, cognitive, and obsessive-compulsive symptoms between males and females. A total of 37 males (97.4%) and 14 females (56%) experienced negative symptoms (χ2=14.16, P=0.000), and 29 males (76.3%) and 10 females (40%) experienced cognitive symptoms (χ2=6.96, P=0.008). Twenty males (52.6%) and 5 females (20%) experienced obsessive-compulsive symptoms (χ2=4.55, P=0.033). No significant differences in other symptoms were observed between two groups. Duration of symptoms from each of the 7 dimensions did not significantly differ between genders, although male patients suffered from negative symptoms for a longer period than female patients did (t=1.754, P=0.086). Further analyses showed that there was a significant negative correlation between the duration of negative symptoms (5.32±4.98 yr) and GAF score at admission in male patients (r=-0.341, P=0.039). This correlation was not significant in female patients.
Our findings demonstrated differences in the frequency of prodromal symptoms between male and female patients with first-episode schizophrenia. Negative symptoms and attenuated positive symptoms were frequent in males, whereas attenuated positive symptoms and mood symptoms in females. In addition, male patients showed more frequent prodromal symptoms in negative, cognitive, and obsessive-compulsive symptom dimensions than female patients did.
In several studies, a prolonged DUP has been predictive of poor prognosis (2, 15) and associated with sustained neuropsychological deficits, increased negative symptoms and disorganization, and unfavorable functional outcome of schizophrenia (16). Moreover, untreated psychosis may constitute an active morbid process toxic to the brain. Lieberman et al. (17) suggested that the process underlying toxic brain damage may be halted by administering proper doses of olanzapine. So far, therefore, there have been many efforts to detect patients presenting active psychotic symptoms and decrease DUP. However, prior to the onset of psychotic symptoms, many patients are usually suffering from various nonspecific symptoms, such as depression, cognitive impairment, or negative symptoms. Additionally, duration of the prodromal phase influenced grey and white matter volumes at the onset of psychosis. That is, the severity of volumetric abnormalities in first-episode psychosis was correlated with the duration of the prodromal phase (18). In light of suffering, functional decline and brain change of patients before the onset of active psychotic symptoms, strategies for early detection and intervention during the prodromal phase will likely gain further prominence in the clinical setting.
According to a retrospective examination of early course of patients with first-episode schizophrenia by Hafner et al. (19), the 10 most frequent and earliest signs of schizophrenia such as restlessness, depression, anxiety, trouble with thinking and concentration, were reported by patients with a first-episode illness. No gender differences were observed in the earliest prodromal symptoms, except worrying, and the first signs of a prodromal phase were depressive and negative symptoms. Whereas they reported the frequency of initial symptoms during the prodromal phase, we emphasized on the frequency of all prodromal symptoms that patients had experienced. Thus, negative, cognitive, and obsessive-compulsive symptoms were more frequent in male patients than in female patients. Cognitive change and negative symptoms such as social withdrawal and decreased energy, may be associated with impaired role functioning. In the present study, the GAF score at admission was inversely correlated with the duration of negative symptoms during the prodromal phase in male patients, although there was no significant difference in the GAF score between genders. Therefore, functional impairment in males may be influenced by the duration of negative symptoms even in the prodromal phase (R2=0.116). This finding agrees with a report by Norman et al. (20) that showed a correlation between impaired functioning in the prepsychosis period and increased negative symptoms in schizophrenia spectrum disorders.
Psychiatric syndromes such as mood disorders, cannabis dependence (21), or anxiety disorders (22) are known to be often comorbid with prodromal schizophrenia. Of 63 patients included in this study, 29 (17 males, 12 females) had prior psychiatric axis I diagnoses before the onset of active psychotic symptoms. Interestingly, there were some differences in the frequency of psychiatric diagnoses between the genders, although a statistical power was not sufficient. Diagnoses among male patients included OCD (n=4), adjustment disorder (n=4), and social phobia (n=3), whereas diagnoses among female patients comprised bipolar disorder (n=4) and major depression (n=3). Female patients tended to have a diagnosis of mood disorder more often. On the contrary, male patients had more frequent diagnoses associated with anxiety disorder. Considering that both male and female patients had mostly attenuated positive symptoms during the prodromal phase, clinicians may need to pay attention to diagnose patients presenting mood symptoms or anxiety symptoms combined with attenuated positive symptoms.
Previous studies have indicated that the DUP and duration of the prodromal phase differ between males and females. Hafner et al. (23) reported that the prodromal period was longer in females than in males, and the DUP has been shown to be significantly longer in males than in females (24). Some factors such as strength of social networks, degree of family involvement, gender difference in help-seeking behavior, and relative frequency of gender-specific stressors may lead to differences in the DUP and the duration of the prodromal period between genders (10, 25). Although no significant differences were observed in the DUP and the duration of prodromal symptoms between males and females in the present study, the differences in the frequency of prodromal symptoms and prior psychiatric diagnoses, and correlation of the duration of negative symptoms with the GAF score at admission in male may have been influenced by several factors. First, females tend to express their emotions more readily and behave in a relatively unobtrusive way. Thus, female patients may be more likely to be misdiagnosed, for example, to be a mood disorder (26). Second, a relative younger age at onset of the prodromal phase in males may also adversely affect their social and cognitive development, resulting in more frequent negative and cognitive symptoms and a negative correlation between the duration of negative symptoms and the GAF score at admission in male patients. Additionally, these phenomenological differences may be derived from neurobiological differences between males and females. Estrogen protects neural circuits by reducing the sensitivity of D2 receptors in the central nervous system and by acting as a neuromodulator with agonistic effects on other transmitter systems, such as serotonin and glutamate (19, 27). Pohjalainen et al. (28) conducted a positron emission tomography study to evaluate the striatal dopamine D2 receptor binding characteristics in 33 healthy males and in 21 healthy females and found that the female group had lower dopamine D2 receptor affinity than the male group. In addition, the prolactin response to neuroleptic medications was greater in females than in males. Kinon et al. (29) reported that among patients receiving treatment with risperidone, females were 2.6 times more likely to develop hyperprolactinemia than males. Moreover, subjective tolerability of antipsychotics differed between genders. Extrapyramidal and anticholinergic reactions were more frequent among female patients, whereas sexual problems were more frequent among male patients (30). In terms of these neurobiological and symptomatological differences, males and females could not be regarded as homogenous group, and therefore, clinicians and researchers should consider the role of gender in the evaluation and treatment of patients.
The present study had several limitations. First, our retrospective chart review is prone to recall and report bias. The onset of prodromal and active psychotic symptoms was determined according to the information provided by patients and their family members. The extent of exploration in the history taking between doctors may have varied. However, we excluded cases whose sources were lacking and chose only cases with comprehensive information. Furthermore, as all of our subjects were admitted for the first time, they may be less prone to recall bias compared to recurrent or chronic patients, although diagnostic stability of these patients may be somewhat compromised. Second, as all subjects in our study were hospitalized, presumably having more severe symptoms, they might represent the patient population with more severe symptoms. Third, data in this study were descriptive and none pertained to the severity of prodromal and psychotic symptoms, except the GAF and CGI scores at admission. The purpose of this study was to investigate the differences in the frequency of early symptoms and signs during the prodromal phase between male and female patients. Therefore, we did not have systematic data to evaluate the severity of symptoms.
In conclusion, our present findings provide evidence for gender differences in the pattern of prodromal symptoms in patients with first-episode schizophrenia. Although our study was retrospective and explorative in its nature, our result alone points that gender differences in prodromal symptoms should be considered when assessing patients presenting nonspecific symptoms combined with attenuated positive symptoms. Further prospective studies exploring the relationship between gender differences in prodromal symptoms and long-term outcomes are warranted.
Figures and Tables
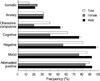 | Fig. 1Frequency of early symptoms during the prodromal phase in patients with first-episode schizophrenia.
*P<0.05 between male and female patients.
|
References
1. Jeppesen P, Petersen L, Thorup A, Abel MB, Ohlenschlaeger J, Christensen TO, Krarup G, Jorgensen P, Nordentoft M. The association between pre-morbid adjustment, duration of untreated psychosis and outcome in first-episode psychosis. Psychol Med. 2008. 38:1157–1166.

2. Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005. 162:1785–1804.

3. McGorry PD, Yung AR, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, Germano D, Bravin J, McDonald T, Blair A, Adlard S, Jackson H. Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry. 2002. 59:921–928.

4. Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophr Res. 2004. 67:131–142.

5. Gourzis P, Katrivanou A, Beratis S. Symptomatology of the initial prodromal phase in schizophrenia. Schizophr Bull. 2002. 28:415–429.

6. Yung AR, McGorry PD. The initial prodrome in psychosis: descriptive and qualitative aspects. Aust N Z J Psychiatry. 1996. 30:587–599.

7. Goldstein J, Lewine R. Castle DJ, McGrath J, Kulkarni J, editors. Overview of sex differences in schizophrenia: Where have we been and where do we go from here? Women and Schizophrenia. 2000. Cambridge: Cambridge University Press;111–143.
8. Leung A, Chue P. Sex differences in schizophrenia, a review of the literature. Acta Psychiatr Scand Suppl. 2000. 401:3–38.
9. Goldstein JM. Sex, hormones and affective arousal circuitry dysfunction in schizophrenia. Horm Behav. 2006. 50:612–622.

10. Willhite RK, Niendam TA, Bearden CE, Zinberg J, O'Brien MP, Cannon TD. Gender differences in symptoms, functioning and social support in patients at ultra-high risk for developing a psychotic disorder. Schizophr Res. 2008. 104:237–245.

11. Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008. 65:28–37.
12. Amminger GP, Leicester S, Yung AR, Phillips LJ, Berger GE, Francey SM, Yuen HP, McGorry PD. Early-onset of symptoms predicts conversion to non-affective psychosis in ultra-high risk individuals. Schizophr Res. 2006. 84:67–76.

13. Hafner H, Riecher-Rossler A, Hambrecht M, Maurer K, Meissner S, Schmidtke A, Fatkenheuer B, Loffler W, van der Heiden W. IRAOS: an instrument for the assessment of onset and early course of schizophrenia. Schizophr Res. 1992. 6:209–223.
14. McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller TJ, Woods SW, Hawkins KA, Hoffman R, Lindborg S, Tohen M, Breier A. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis. I. Study rationale and design. Schizophr Res. 2003. 61:7–18.
15. Norman RM, Malla AK. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol Med. 2001. 31:381–400.

16. Bottlender R, Strauss A, Moller HJ. Impact of duration of symptoms prior to first hospitalization on acute outcome in 998 schizophrenic patients. Schizophr Res. 2000. 44:145–150.

17. Lieberman JA, Tollefson G, Tohen M, Green AI, Gur RE, Kahn R, McEvoy J, Perkins D, Sharma T, Zipursky R, Wei H, Hamer RM. Comparative efficacy and safety of atypical and conventional antipsychotic drugs in first-episode psychosis: a randomized, double-blind trial of olanzapine versus haloperidol. Am J Psychiatry. 2003. 160:1396–1404.

18. Lappin JM, Dazzan P, Morgan K, Morgan C, Chitnis X, Suckling J, Fearon P, Jones PB, Leff J, Murray RM, McGuire PK. Duration of prodromal phase and severity of volumetric abnormalities in first-episode psychosis. Br J Psychiatry Suppl. 2007. 51:S123–S127.
19. Hafner H, Loffler W, Maurer K, Hambrecht M, an der Heiden W. Depression, negative symptoms, social stagnation and social decline in the early course of schizophrenia. Acta Psychiatr Scand. 1999. 100:105–118.

20. Norman RM, Scholten DJ, Malla AK, Ballageer T. Early signs in schizophrenia spectrum disorders. J Nerv Ment Dis. 2005. 193:17–23.

21. Rosen JL, Miller TJ, D'Andrea JT, McGlashan TH, Woods SW. Comorbid diagnoses in patients meeting criteria for the schizophrenia prodrome. Schizophr Res. 2006. 85:124–131.

22. Svirskis T, Korkeila J, Heinimaa M, Huttunen J, Ilonen T, Ristkari T, McGlashan T, Salokangas RK. Axis-I disorders and vulnerability to psychosis. Schizophr Res. 2005. 75:439–446.

23. Hafner H, Maurer K, Loffler W, Riecher-Rossler A. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993. 162:80–86.

24. Larsen TK, McGlashan TH, Moe LC. First-episode schizophrenia: I. Early course parameters. Schizophr Bull. 1996. 22:241–256.

25. Cohen RZ, Gotowiec A, Seeman MV. Duration of pretreatment phases in schizophrenia: women and men. Can J Psychiatry. 2000. 45:544–547.

26. Folnegovic Z, Folnegovic-Smalc V. Schizophrenia in Croatia: age of onset differences between males and females. Schizophr Res. 1994. 14:83–91.
27. Behl C, Skutella T, Lezoualc'h F, Post A, Widmann M, Newton CJ, Holsboer F. Neuroprotection against oxidative stress by estrogens: structure-activity relationship. Mol Pharmacol. 1997. 51:535–541.

28. Pohjalainen T, Rinne JO, Nagren K, Lehikoinen P, Anttila K, Syvalahti EK, Hietala J. The A1 allele of the human D2 dopamine receptor gene predicts low D2 receptor availability in healthy volunteers. Mol Psychiatry. 1998. 3:256–260.

29. Kinon BJ, Gilmore JA, Liu H, Halbreich UM. Prevalence of hyperprolactinemia in schizophrenic patients treated with conventional antipsychotic medications or risperidone. Psychoneuroendocrinology. 2003. 28:Suppl 2. 55–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download