Abstract
Percutaneous cardiopulmonary support (PCPS) is a widely accepted treatment for severe cardiopulmonary failure. This system, which uses a percutaneous approach and autopriming devices, can be rapidly applied in emergency situations. We sought to identify the risk factors that could help predict in-hospital mortality, and to assess its outcomes in survivors. During a 2-yr period, 50 patients underwent PCPS for the treatment of severe cardiopulmonary failure, and of those, 22 (44%) were classified as survivors and 28 (56%) as non-survivors. We compared the 2 groups for risk factors of in-hospital mortality and to establish proper PCPS timing. Twenty patients underwent PCPS for acute myocardial infarction, 20 for severe cardiopulmonary failure after cardiac surgery, 7 for acute respiratory distress syndrome, and 3 for acute myocarditis. Multivariate analysis showed that an acute physiology, age, and chronic health evaluation (APACHE) III score ≥50 prior to PCPS was the only significant predictor of in-hospital mortality (P=0.001). Overall 18-month survival was 42.2%. Cox analysis showed patients with APACHE III scores ≥50 had a poor prognosis (P=0.001). Earlier application of PCPS, and other preemptive strategies designed to optimize high-risk patients, may improve patient outcomes. Identifying patients with high APACHE scores at the beginning of PCPS may predict in-hospital mortality. Survivors, particularly those with higher APACHE scores, may require more frequent follow-up to improve overall survival.
The percutaneous cardiopulmonary support system (PCPS) has gained wide acceptance in circulatory support because it produces favorable results and remarkable advances in catheters and membrane oxygenators (1, 2). PCPS is currently used for severe cardiac failure, cardiogenic shock, and/or postoperative cardiac support (3-5). Although PCPS can easily be started using a heparin-coated circuit, a centrifugal pump, and membrane oxygenators, some PCPS patients cannot be easily weaned from its support. In addition, PCPS has been associated with clinical problems, including left ventricular afterload, limb ischemia, decreased platelet count, bleeding, inguinal infection, and complications from multiple organ failure (MOF) (6). Thus, determining the indicators for starting and discontinuing PCPS remain clinically problematic. To determine factors predicting the outcome of PCPS, we retrospectively reviewed results of patients treated with PCPS for severe cardiopulmonary failure.
We retrospectively reviewed the medical records of patients treated with PCPS at Yonsei University Health System between November 2005 and December 2007. Our study followed the guidelines of the Institutional Review Board of Yonsei University College of Medicine (Yonsei IRB No. 4-2007-0248).
The PCPS system consists of a hollow-fiber microporous membrane oxygenator, a centrifugal pump, arterial and venous cannulae, and standard 3/8-inch tubing. The blood-contact surfaces of these components were heparin-coated. PCPS was established with venous drainage (17 Fr or 19 Fr) from the femoral vein (the tip of the tube was placed in the right atrium) and arterial blood was basically returned to the femoral artery using a 17 Fr or 19 Fr arterial cannula. We used a Capiox SP Pump Controller Sp-101 and Capiox circuit (Terumo Co., Tokyo, Japan). Initial PCPS flow ranged from 2.0 to 3.0 L/min/m2 to maintain optimal hemodynamics, adjusted for each patient. Activated clotting time was maintained at 180-200 sec and a heparin bolus was used at the time of cannulation followed by a continuous intravenous infusion of heparin during PCPS use.
Patients with severe cardiac failure are indicated for PCPS at our hospital if their peak systolic blood pressure is less than 80 mmHg and their cardiac index is less than 1.8 L/min/m2 for more than 30 min after the correction of hypovolemia, hypoxemia, and acidosis while under maximal medical treatment. PCPS is also indicated for rapid deterioration of cardiac output that is unresponsive to intra-aortic balloon pumping (IABP), in patients who could not be discontinued from cardiopulmonary bypass after cardiovascular surgery, for respiratory arrest, and for acute respiratory distress syndrome (ARDS). The decision to initiate and continue PCPS therapy was made by the physician in charge (Table 1).
PCPS flow was gradually decreased while monitoring hemodynamics through a transesophageal or transthoracic echocardiogram when terminating PCPS. If an indwelling Swan-Ganz catheter was present, continuous cardiac output or pulmonary artery pressure was maintained using a sufficient preload of catecholamine followed by administration of the required dose after hemodynamic stabilization. PCPS could then be terminated when PCPS flow was between 1.5 and 2.0 L/min and the hemodynamics were stable, i.e., mean systolic blood pressure was greater than 80 mmHg, central venous pressure was less than 15 mmHg, and pulse pressure was greater than 30 mmHg.
The patients were divided into 2 groups: those who were successfully weaned from PCPS and discharged from the ICU, and those who eventually died in hospital. The two groups were compared with respect to age, gender, body surface area, cardiopulmonary resuscitation (CPR), CPR time, surgery, ischemic heart disease, use of IABP, use of continuous renal replacement therapy, and whether or not the patient had methicillin-resistant Staphylococcus aureus (MRSA) infection. The PCPS flow, acute physiology, age, and chronic health evaluation (APACHE) III score, and dose of catecholamine used (epinephrine, norepinephrine, dopamine, and dobutamine) over the 72-hr period beginning at the time PCPS began were also compared between the 2 groups (Table 2).
The APACHE III prognostic system, which was developed in the United States based on data collected from 17,440 ICU admissions at 42 ICUs, consists of 2 components: an APACHE III score, which can provide initial risk stratification for severely ill hospitalized patients within independently defined patient groups; and an APACHE III predictive equation, which uses the APACHE III score and reference data on major disease categories and treatment locations immediately prior to ICU admission to provide risk estimates for inhospital mortality of individual ICU patients. A 5-point increase in APACHE III score (range, 0 to 299) has been shown to be independently associated with a statistically significant increase in the relative risk of hospital death within each of the 78 major medical and surgical disease categories. All of the 50 patients who required PCPS were scored according to the APACHE III prognostic system (7). APACHE III scores were calculated by summing the acute physiological score, age score, and chronic health evaluation scores. Acute physiological scores were calculated by summing scores for 17 variables before initiating PCPS. APACHE III scores were recorded for 72 hr after PCPS application.
Data were analyzed using SPSS for Windows, version 12.0 (SPSS, Inc, Chicago, IL, U.S.A). Categorical variables were compared using chi-square or Fisher's exact tests, and continuous variables were compared using Student's t or Mann-Whitney U tests as appropriate. The risk of ICU mortality associated with selected factors was evaluated using stepwise binary logistic regression analysis to estimate odds ratio (OR) and their 95% confidence interval (CI). Continuous variables were dichotomized using the median values as cutoff. A P value ≤0.05 according to univariate analysis was the criterion for submitting variables to the model. Goodness of fit was assessed using the Hosmer and Lemeshow chi-square test. The relative risk, defined as the ratio of incidence among exposed to that among non-exposed subjects, was used to summarize the strength of the association between risk factors and pulmonary complications. The 95% CIs of the relative risk were calculated using Miettinen's test-based approach. Unless otherwise stated, results are expressed as mean±standard deviation (SD) for continuous variables, and as percentages for categorical variables. Estimates of survival were obtained using the Kaplan-Meier method. Cox proportional hazards methodology was used to model the probability of survival as a function of time and to assess differences in survival associated with various patient characteristics. Risk ratios (also referred to as hazard ratios) and 95% CIs are presented to indicate significance in multivariate models. Multivariate modeling was initially executed using forward selection, followed by confirmation using backward selection. No variable was forced to remain in a model, and variables associated with a P value ≤0.05 were maintained in the model. Statistical comparisons were made using chi-square analysis or analysis of variance (ANOVA) followed by Fisher's protected least significant difference.
In total, 50 patients (30 men, 20 women), of mean age 64.6±11.6 yr (range, 46 to 92 yr), were treated with PCPS for severe cardiopulmonary failure in the ICU. Of the 20 patients who had undergone cardiovascular surgery, 15 used cardiopulmonary bypass (4 on-pump coronary artery bypass grafting, 4 valve surgery, 4 aortic surgery, 3 congenital heart surgery; mean total cardiopulmonary bypass time, 215 min; mean aortic cross clamp time, 175 min), 3 underwent off-pump coronary artery bypass grafting, 1 pericardiectomy, and 1 pericardial window formation. Twenty patients suffered from acute myocardial infarction with unstable hemodynamics. The indications for PCPS are listed in Table 1.
Nineteen patients (38%) went into cardiac arrest prior to PCPS application, 3 went into cardiogenic shock before percutaneous coronary intervention (PCI), 3 after PCI, 11 after cardiac surgery (including 1 patient with postoperative intractable arrhythmia), and 2 had ARDS. The mean CPR time before PCPS application was 40.7±42.6 min (range, 7 to 144 min). Intraaortic balloon pumps were needed in 9 patients (18%). Renal failure was evident in 17 patients (34%) who were treated with continuous infusions of diuretics, low-dose dopamine, and eventually renal replacement therapy (hemodialysis in 16 patients, and peritoneal dialysis in 1 patient). Invasive nutritional support was used in almost all patients. Nineteen patients (38%) were diagnosed with a clinically significant MRSA infection at some stage during hospitalization.
PCPS was successfully terminated in 22 patients (44%). Of 28 patients (56%) in whom PCPS could not be terminated, 9 died of persistent cardiac failure, 9 of MOF, 9 of sepsis, and 1 of respiratory failure due to ARDS. For all patients, the mean duration of PCPS support was 29.1±33.0 hr (range, 18 min to 126.2 hr) and the mean ICU stay was 17±25 days (range, 2 to 110 days). Bleeding complications occurred in 2 patients, with 1 each having upper gastrointestinal tract bleeding and hemopericardium. Lower limb ischemia occurred in 2 patients as a thrombotic complication associated with the insertion of the arterial cannula. One of these patients had to undergo a below-knee amputation, despite a Fogarty thromboembolectomy in the right popliteal artery. The other patient required transmetatarsal amputation of the left foot.
Twenty one variables were examined for possible associations with hospital mortality (Table 2). Variables first underwent univariate analysis and then underwent multivariate analysis, adjusting for confounders, if they were found to be significant. Univariate analysis showed that the following 6 variables were associated with in-hospital mortality: a higher APACHE III score, surgery, continuous renal replacement therapy, MRSA infection, initial PCPS flow, and a longer total pump time. The incidence of cardiac arrest prior to PCPS application did not differ between survivors and non-survivors, nor did the incidence of IABP insertion (P=0.339). Figs. 1, 2 show the serial change of catecholamine dose required (dopamine, dobutamine, epinephrine, and norepinephrine). Non-survivors required a higher dosage of catecholamine for the first 72 hr after initiation of PCPS, but the difference was not significant (P>0.05). Fig. 3 shows the change of APACHE III scores over 72 hr. The 2 groups showed significant differences on a repeated generalized linear model (P=0.025).
Stepwise forward binary logistic regression analysis identified that an APACHE III score 50 or greater prior to PCPS was the most significant factor related to prognosis (OR, 14.351; CI, 3.127-72.338; P=0.001). This result was confirmed using a stepwise, backward binary logistic regression analysis. Patients with an APACHE III score higher than 50 on the initial day of PCPS had an in-hospital mortality of 73.5% (25 of 34) (Table 3).
Patient follow up was complete (median follow-up, 12.7 months; range, 2.0 to 19.6 months). Overall 18-month survival was 42.2%. Cox proportional hazard regression analysis showed that patients with APACHE III scores ≥50 had a poor prognosis. Overall survival at 18 months was 78.8% for patients with APACHE scores <50 and 26.1% for patients with APACHE III scores ≥50 (P=0.001) (Fig. 4). At last follow up, 11 patients were in the NYHA functional class I, 7 patients in class II, and 4 patients in class III.
Recent developments in medical engineering have resulted in innovations that have transformed PCPS into a compact, battery-powered, portable heart-lung machine that can be implemented rapidly in any area of the hospital using thin-walled cannulas inserted via the femoral vessels (8). Because PCPS is a portable and powerful resuscitative tool, it has been effectively used for the treatment of cardiac failure in various situations, including postcardiotomy low cardiac output syndrome (6, 9), prolonged cardiopulmonary resuscitation (10), and acute myocardial infarction (10). In addition, PCPS has been used prophylactically in high-risk coronary patients needing percutaneous stent revascularization (12). When used for cardiac arrest during coronary intervention in the catheterization laboratory, PCPS has demonstrated a late survival rate ranging between 57% and 64% (13-15) and a late survival rate ranging between 56% and 66.7% for postoperative low output syndrome (9).
Between February 1998 and October 2005, before the introduction of the PCPS system, we used an extracorporeal membrane oxygenator (ECMO), but the outcomes were dismal, with an ECMO in-hospital mortality rate of 91.6% (11 of 12) (data not shown here). After switching to the PCPS system, however, this rate was reduced significantly, to 56% (28 of 50). However, PCPS is limited in its ability to promote the recovery of left ventricular function in the presence of seriously damaged myocardium.
To clarify the effectiveness of PCPS, we analyzed the background, characteristics, and the prognosis of patients who underwent PCPS for the treatment of severe cardiopulmonary failure due to various causes, including postcardiac surgery, ARDS, acute myocardial infarction, and acute myocarditis. We found that a higher APACHE III score at the beginning of PCPS, higher initial pump flow, and longer duration of bypass time were predictors of poor outcome of PCPS. Although PCPS was initially used to save the lives of patients with severe cardiac failure who required an extreme dose of catecholamine and in whom IABP was not sufficient to maintain circulation, indications for PCPS have widened. We found that APACHE III score ≥50 and serial changes in APACHE III score during the first 72 hr were predictive of in-hospital mortality.
Then, how can we reduce PCPS in-hospital mortalities? This study revealed several factors could predict PCPS mortality. To improve APACHE III scores at the beginning of PCPS, an earlier application of PCPS would be helpful to break a vicious circle and reduce initial pump flow, and the duration of bypass time. Since October 2005, our policies for PCPS application have changed in several aspects. We performed early orotracheal intubation and full sedation for several days, especially in ARDS patients, with early, low-dose steroid therapy as guidelines indicated. When deciding to apply PCPS, we did not hesitate to apply PCPS to patients who suffered from severe cardiopulmonary failure with hemodynamic compromise. If needed, early bedside tracheotomies were performed. Ultimately, we have undertaken aggressive and early preemptive management to break this vicious circle.
We observed 2 instances of PCPS-related bleeding and 2 thrombotic complications. Before using the PCPS system, cannulas were not heparin-coated, requiring us to maintain an activated clotting time of 250 sec or greater, thus leading to a 50% (6/12, data not shown here) incidence of bleeding complications. Use of heparin-coated cannulas and tubes has enabled us to maintain an activated clotting time of about 180-200 sec. Thrombotic complications after removing PCPS cannulas may be prevented by routine performance of distal lower limb perfusion at the beginning of PCPS. Moreover, when removing the PCPS catheter, the proximal and distal parts of the femoral artery should be clamped, a sufficient amount of blood should be flushed to remove any thrombus in the lumen, and the femoral artery should be repaired.
Among the limitations of this study were its retrospective design and the presence of typical institutional biases regarding patient selection. However, we sought to analyze a relatively homogenous population by using patients with cardiovascular disease. Although survival from PCPS was the primary end point, we should have evaluated other significant patient outcomes after discharge, including comfort, advancement of oral nutrition, improved patient-family communication, and simplified nursing care. Since these measurements could not be easily abstracted and quantified, these analyses were not undertaken.
In conclusion, our findings indicate that earlier application of PCPS, which lowers initial APACHE III scores, as well as other preemptive strategies designed to optimize high-risk patients, may improve patient outcomes. Identifying patients with high APACHE scores at the beginning of PCPS may predict the risk of in-hospital mortality. Survivors from PCPS, particularly those with higher initial APACHE scores, may require more careful and frequent short-term follow up.
Figures and Tables
Fig. 1
Serial catecholamine dose administered during PCPS to survivors and nonsurvivors. (A) Dopamine, (B) Dobutamine. The two groups did not differ significantly using a repeated generalized linear model (P>0.05).

Fig. 2
Serial catecholamine dose administered during PCPS to survivors and non-survivors. (A) Epinephrine, (B) Norepinephrine. The two groups did not differ significantly using a repeated generalized linear model (P>0.05)

Fig. 3
Serial APACHE III scores during PCPS of survivors and non-survivors. The two groups differed significantly using a repeated generalized linear model (P=0.025).
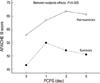
Fig. 4
Overall survival in patients with PCPS relative to initial APACHE III scores. Overall survival at 18 months was 87.5% for patients with APACHE scores <50 and 28.8% for patients with APACHE III scores ≥50 (P=0.001).

Table 2
Univariate analysis of in-hospital mortality

Values are expressed as mean±SD or as n (%).
OR, odds ratio; CI, confidence interval; BSA, body surface area; APACHE, acute physiology, age, and chronic health evaluation; CPR, cardiopulmonary resuscitation; IABP, intraaortic balloon pump; CRRT, continuous renal replacement therapy; MRSA, methicillin-resistant Staphylococcus aureus; ICU, intensive care unit.
ACKNOWLEDGMENTS
The authors are grateful to Soon-Young Sul, RN, Hee-Jung Lee, RN, Sun-Hee Lim, RN, and Eun-A Kang, RN for their contributions in collecting data found in this article.
References
1. Phillips SJ, Ballentine B, Slonine D, Hall J, Vandehaar J, Kongtahworn C, Zeff RH, Skinner JR, Reckmo K, Gray D. Percutaneous initiation of cardiopulmonary bypass. Ann Thorac Surg. 1983. 36:223–225.

2. Vogel RA, Shawl F, Tommaso C, O'Neill W, Overlie P, O'Toole J, Vandormael M, Topol E, Tabari KK, Vogel J. Initial report of the National Registry of Elective Cardiopulmonary Bypass Supported Coronary Angioplasty. J Am Coll Cardiol. 1990. 15:23–29.

3. Magovern GJ Jr, Magovern JA, Benckart DH, Lazzara RR, Sakert T, Maher TD Jr, Clark RE. Extracorporeal membrane oxygenation: preliminary results in patients with postcardiotomy cardiogenic shock. Ann Thorac Surg. 1994. 57:1462–1468.

4. Mair P, Hoermann C, Moertl M, Bonatti J, Falbesoner C, Balogh D. Percutaneous venoarterial extracorporeal membrane oxygenation for emergency mechanical circulatory support. Resuscitation. 1996. 33:29–34.

5. Younger JG, Schreiner RJ, Swaniker F, Hirschl RB, Chapman RA, Bartlett RH. Extracorporeal resuscitation of cardiac arrest. Acad Emerg Med. 1999. 6:700–707.

6. Hata M, Shiono M, Orime Y, Yagi SY, Yamamoto T, Okumura H, Kimura SI, Nakata KI, Kashiwazaki S, Choh S, Negishi N, Sezai Y. Strategy of circulatory support with percutaneous cardiopulmonary support. Artif Organs. 2000. 24:636–639.
7. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991. 100:1619–1636.
8. Kurusz M, Zwischenberger JB. Percutaneous cardiopulmonary bypass for cardiac emergencies. Perfusion. 2002. 17:269–277.

9. Hayashi Y, Ohtake S, Sawa Y, Nishimura M, Ichikawa H, Satoh H, Yamaguchi T, Suhara H, Sakaguchi T, Matsuda H. Percutaneous cardiopulmonary support with heparin-coated circuits in postcardiotomy cardiogenic shock. Efficacy and comparison with left heart bypass. Jpn J Thorac Cardiovasc Surg. 2000. 48:274–279.
10. Chen YS, Chao A, Yu HY, Ko WJ, Wu IH, Chen RJ, Huang SC, Lin FY, Wang SS. Analysis and results of prolonged resuscitation in cardiac arrest patients rescued by extracorporeal membrane oxygenation. J Am Coll Cardiol. 2003. 41:197–203.

11. Aiba T, Nonogi H, Itoh T, Morii I, Daikoku S, Goto Y, Miyazaki S, Sasako Y, Nakatani T. Appropriate indications for the use of a percutaneous cardiopulmonary support system in cases with cardiogenic shock complicating acute myocardial infarction. Jpn Circ J. 2001. 65:145–149.

12. Suárez de Lezo J, Pan M, Medina A, Pavlovic D, Romero M, Segura J, Ruiz M, Ojeda S, Muñoz J, Rodriguez M. Percutaneous cardiopulmonary support in critical patients needing coronary interventions with stents. Catheter Cardiovasc Interv. 2002. 57:467–475.

13. Mooney MR, Arom KV, Joyce LD, Mooney JF, Goldenberg IF, Von Rueden TJ, Emery RW. Emergency cardiopulmonary bypass support in patients with cardiac arrest. J Thorac Cardiovasc Surg. 1991. 101:450–454.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download