Abstract
Recently the prevalence of both asthma and obesity have increased substantially in many countries. The aim of this study was to evaluate the role of retinol-binding protein (RBP) 4 in childhood asthma and its association with atopy markers, pulmonary function, and bronchial hyperresponsiveness in relation to obesity. We studied 160 children between the ages 6 to 10 yr, including 122 asthmatics and 38 controls. The body mass index, pulmonary function tests, and methacholine challenge tests were measured on the same day. Total eosinophil count, serum total IgE, serum eosinophil cationic protein, and serum RBP4 were measured in all subjects. There was no difference in serum RBP4 levels between the asthmatics and the control group. In all subjects or subgroups, serum RBP4 was not associated with total eosinophil count, serum total IgE, serum eosinophil cationic protein, or PC20. There was no relationship between serum RBP4 and pulmonary function in female asthmatics. Forced expiratory volume in 1 second/forced vital capacity (FVC) and forced expiratory flow between 25% and 75% of FVC contributed to serum RBP4 in male asthmatics. Our findings show an association between RBP4 and pulmonary function in prepubertal male asthmatics. This relationship may indirectly affect the high prevalence of childhood asthma in males.
Asthma is one of the most common chronic illnesses in children, and obesity is another important public health problem that can affect children (1, 2). Recently the prevalence of both asthma and obesity have increased substantially in many countries, leading to speculation that obese people might be at an increased risk of developing asthma (3, 4). Although a large number of studies have been performed, the possibility that obesity might increase the risk of asthma development remains controversial (5). Nevertheless, potential mechanisms have been suggested that obesity-related changes in lung volumes, systemic inflammation, and other adipocyte-derived factors such as leptin, adiponectin, resistin, and visfatin, as well as cytokines and chemokines that might alter smooth muscle function in such a way as to promote airway narrowing (2, 6).
Asthma is recognized as a chronic inflammatory disease in the airways (7), and the obese state is characterized by low-grade systemic inflammation, as indicated by increased levels of the inflammatory markers c-reactive protein (CRP) and IL-6 in the circulation of obese subjects (6). The effects of increased body mass index (BMI) on asthma may be mediated by upregulation of inflammatory mechanisms in the airway epithelium (8). The current view of adipose tissue is that of an active secretory organ, sending out and responding to signals that modulate appetite, energy expenditure, insulin sensitivity, endocrine and reproductive systems, bone metabolism, and inflammation and immunity (6). The serum concentrations of many adipokines could impact airway function, which might lead to asthma in both human and murine subjects with obesity (9). A recent study showed that leptin, an adipokine, might play a role in atopic asthma in children (8). Retinol-binding protein (RBP) 4 is highly expressed in isolated mature human adipocytes and secreted by differentiating human adipocytes (10). Previous studies have reported significant associations between RBP4 levels and BMI (11, 12). In contrast, other studies have not found a link between RBP4 levels and BMI (13, 14). Recent reports showed that RBP4 correlated with inflammatory factors such as CRP and IL-6 (15), and RBP4 mRNA had a strong positive correlation with markers of adipose inflammation (monocyte chemoattractant protein-1 and CD68) (16). Several studies have been reported on the relationship between RBP4 and obesity, adipose inflammation but, there has been no reports showing association between RBP4 and childhood asthma.
We evaluated the role of RBP4 in childhood asthma and its association with atopy markers, pulmonary function, and bronchial hyperresponsiveness.
One hundred sixty prepubertal subjects, aged from 6 to 10 yr, were recruited from Severance Hospital, Yonsei University College of Medicine. Asthma was defined as recurrent wheezing or coughing episodes in the absence of common cold in the preceding 12 months. Additionally a physician's diagnosis of bronchial hyperresponsiveness upon methacholine challenge (PC20≤16 mg/mL) and at least 12% reversibility of forced expiratory volume in 1 second (FEV1) after inhaling a β2 agonist, as per criteria of the American Thoracic Society (ATS), were required (17). All participants were enrolled before administering oral or inhaled corticosteroids. Children with history of asthma attacks requiring systemic corticosteroids within the preceding 6 months were excluded. The control participants were age-matched healthy children who visited the hospital for a general health work-up or vaccination and had no history of wheezing, recurrent chronic disease, infection during the preceding two weeks, or hypersensitivity to methacholine.
Height and weight were measured in light clothing without shoes to calculate BMI in kg/m2. Obesity and overweight classification were defined by BMI for age and sex based on an international survey (18). Absolute BMI values were then converted to previously established BMI percentiles of Korean children for data analysis (19). The 85th and 95th percentiles of BMI for age and sex were used as cut off values to identify normal weight, overweight and obesity. Informed written consent was obtained from all participants before inclusion in the study. The study was approved by the Severance Hospital Institutional Review Board beforehand.
Lung function was measured by spirometry (Vmax encore; VIASYS Healthcare Inc., Conshohocken, PA, U.S.A.) according to ATS standards (17). Bronchial hyperresponsiveness was assessed in all participants by the methacholine challenge test. Children were eligible if they could perform reproducible spirometry and had an FEV1 of at least 70% of the predicted value (20). In short, after saline inhalation, doses of methacholine (0.075, 0.15, 0.31, 0.62, 1.25, 2.5, 5, 10, and 25 mg/mL) were delivered for 0.6 sec through a DeVilbiss 646 nebulizer using a Rosenthal-French dosimeter (Ferraris, Hertford, England) until either FEV1 decreased by 20% or more, or the highest dose administered. FEV1 was measured 60 to 90 sec after each inhalation. The methacholine concentration inducing a 20% decrease in FEV1 (PC20) was recorded. The challenge test was considered positive if the PC20 was 16 mg/mL or less. Anti-inflammatory preparations and bronchodilators were withheld for 24 hr before the test.
The NE-8000 system (Sysmex, Kobe, Japan) was used to count eosinophils automatically in peripheral blood. Serum total IgE and ECP were measured by the CAP radioallergosorbent technique (UniCAP; Pharmacia and Upjohn, Uppsala, Sweden). Blood samples to measure serum RBP4 levels were obtained between 6 a.m. and 9 a.m. after an overnight fast. After clotting at 4℃, the serum was separated by centrifugation at 1,300 g for 10 min and stored at -70℃ until the assays. Serum RBP4 concentrations were measured with a human RBP4 Competitive ELISA Kit (AdipoGen, Seoul, Korea) according to the manufacturer's instructions. The minimum RBP4 detection limit was 1 ng/mL and all assays were performed in duplicate for each sample, with the mean values reported here.
Descriptive statistics were calculated as the mean±SD or as median (interquartile range) for continuous variables. Comparisons between groups were made using a Student's t-test, Mann-Whitney U test or chi-square test. Simple linear regression analysis was performed to assess the age, BMI, FEV1, FEV1/forced vital capacity (FVC), forced expiratory flow between 25% and 75% of FVC (FEF25-75%), PC20, eosinophil count, serum total IgE and ECP on RBP4 levels. A P value less than 0.05 was considered statistically significant. All analyses were performed on the Statistical Package for the Social Sciences software (version 13.0, SPSS Inc, Chicago, IL, U.S.A.).
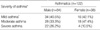
The study included 122 patients with asthma and 38 controls. The participants consisted of 102 boys (63.8%) and 58 girls (36.2%) (mean age, 8.6±1.2 yr). The mean values for age and BMI percentile were not different between the asthmatics and healthy children. Boys were more predominant in the asthmatic group. Eosinophil count, serum total IgE and ECP were statistically higher in the asthmatics than the control subjects. FEF25-75% was significantly lower in the asthmatics than the control subjects (Table 1). In asthmatics, there was no gender difference in asthma severity (P=0.256) (Table 2).
The mean RBP4 concentration, shown in Fig. 1, was not significantly different between the asthmatics and control subjects (mean±SD, 256.91±93.37 µg/mL vs. 264.20±151.79 µg/mL, P=NS).
Simple linear regression analysis was performed with RBP4 as the dependent variable and age, BMI percentile, eosinophil count, serum total IgE, ECP, FEV1, FEV1/FVC, FEF25-75% and PC20 as the independent variables for asthmatics divided by sex (Table 3). The results indicate that FEV1/FVC and FEF25-75% contribute significantly to serum RBP4 level in boys with asthma. No other parameters were shown to contribute to RBP4. No variables significantly contributed to RBP4 in girls with asthma. In normal weight, overweight, and obesity group, no variables were correlated to RBP4 in both sexes and between the asthmatics and the control subjects (data not shown). According to asthma severity, serum total IgE and FEF25-75% contribute to serum RBP4 only in mild asthma group (data not shown). In male asthmatics, serum total IgE, FEV1, and FEF25-75% also contribute significantly to serum RBP4 in mild group (data not shown). No variables were associated with serum RBP4 in moderate and severe group both in all and male asthmatics (data not shown).
The aim of this study was to investigate serum RBP4 levels and its relationship between the parameters of atopy, pulmonary function, and bronchial hyperresponsiveness. There were no differences in mean serum RBP4 concentrations between the asthmatics and the control subjects. There was also no significant correlation between serum RBP4 and BMI for both the asthmatics and control group. FEV1/FVC and FEF25-75% contributed to serum RBP4 levels in male asthmatics.
There are several proposed mechanisms by which obesity can affect airway function (21). A recent review touched on the mechanical, immunological, hormonal and inflammatory effects of obesity that may play a role in the development and persistence of asthma (21, 22). Although a large number of cross-sectional, case-control, prospective and weight loss studies have been performed, the possibility that obesity might increase the risk of asthma development still remains controversial (3, 21). Our findings suggest that there is no direct association between BMI and asthma. Although a small study sample and a relatively small obese group may have affected the results, the proportion of obese people in our study is similar to the proportion of obese people in the general Korean population. Both the low proportion of obesity and the rarity of severe obesity in Korea may also have affected the results. The fact that the subjects were prepubertal (younger than 10 yr) may also have influenced the results by excluding the effects of sex hormones. Although the possibility that obesity might increase the risk of asthma remains controversial, their correlation is still a matter of concern. It is well documented that obesity is an inflammatory state that leads to increased levels of hormones such as leptin, cytokines such as interleukin-6 and tumor necrosis factor-α, chemokines and other inflammatory mediators that could potentially influence airway smooth muscle (6). RBP4 is a newly discovered fat-derived peptide that modulates glucose metabolism and consequently induces insulin resistance (23). A recent report suggests that RBP4 is a central mediator of obesity-induced insulin resistance in mice and humans (24). Mean serum RBP4 levels were elevated in both nondiabetic and diabetic obese subjects, and serum RBP4 levels were positively correlated with BMI (25). Previous studies have shown that RBP4 levels are elevated in obese patients (12, 24, 25). On the other hand, another report showed no association between plasma RBP4 levels and BMI (13). Our results show that serum RBP4 is not related to BMI. RBP4 level was not different between the asthmatics and normal control groups, and there were no differences in BMI between the asthmatics and controls in our study. The relatively narrow BMI distribution of our study subjects might explain the lack of a relationship.
Simple linear regression analysis revealed that both FEV1/FVC and FEF25-75% are predictive factors of RBP4 for male asthmatics in our study. The FEV1 to FVC ratio is a useful assessment of airflow limitation (26). Recently, FEV1/FVC was reported to be a predictive factor for basement membrane thickness, which is a known early airway remodeling marker (27). Among the respiratory indices derived from the forced vital capacity maneuver, maximal midexpiratory flow rate (MMEF) namely FEF25-75%, which measures the average flow of gas through the middle lung volumes, was originally considered a more sensitive and earlier marker of obstruction in the small airways than FEV1 (28, 29). Our findings show that these two parameters contribute to serum RBP4 levels. The relationship between serum RBP4 and pulmonary function might be indirectly associated with lung inflammation, changes in small airways, and airflow obstruction, all part of asthma pathogenesis. It is known that asthma is more prevalent in boys younger than 10 yr or the mid-teens, at which point asthma is more prevalent in girls until sexual maturity (30). A current study shows that high serum leptin levels in asthmatic boys may partly explain the higher prevalence of childhood asthma in males (8). Our results support this phenomenon. No explanation for the phenomenon has been given. The often hypothesized role of sexual hormones still remains to be demonstrated (30).
Our research establishes the first causal relationship between serum RBP4 and asthma. We excluded the effects of sex hormones by recruiting prepubertal children as study subjects. The small number of participants and the relatively small obese group are limitations of this study. Relatively small number of female asthmatics may also have affected the results.
In conclusion, our findings suggest an association between RBP4 and pulmonary function in prepubertal male asthmatics. This relationship may indirectly affect the high prevalence of childhood asthma in males.
Figures and Tables
Fig. 1
Serum RBP4 levels do not show any difference between the asthmatics and the controls in all, male and female participants (P>0.05). Data represent median values.

Table 3
Simple linear regression analysis between RBP4 and variables in asthmatics

In all analyses, the dependent variable was RBP4. All analyses are adjusted for age.
B, unstandardized regression coefficient; SE, standard error; Beta, standardized; regression coefficient; BMI, body mass index; TEC, total eosinophil count; ECP, eosinophil cationic proteinl; FEV1, forced exporatory volume in 1 second, FVC, forced vital capacity; FEF25-75%, forced expiratory flow between 25% and 75% of forced vital capacity.
References
1. Yawn BP, Brenneman SK, Allen-Ramey FC, Cabana MD, Markson LE. Assessment of asthma severity and asthma control in children. Pediatrics. 2006. 118:322–329.

2. Shore SA, Fredberg JJ. Obesity, smooth muscle, and airway hyperresponsiveness. J Allergy Clin Immunol. 2005. 115:925–927.

4. Leung TF, Li CY, Lam CW, Au CS, Yung E, Chan IH, Wong GW, Fok TF. The relation between obesity and asthmatic airway inflammation. Pediatr Allergy Immunol. 2004. 15:344–350.

5. Matsuda K, Nishi Y, Okamatsu Y, Kojima M, Matsuishi T. Ghrelin and leptin: a link between obesity and allergy? J Allergy Clin Immunol. 2006. 117:705–706.

6. Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005. 115:911–919.

7. Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma. From bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000. 161:1720–1745.
8. Guler N, Kirerleri E, Ones U, Tamay Z, Salmayenli N, Darendeliler F. Leptin: does it have any role in childhood asthma? J Allergy Clin Immunol. 2004. 114:254–259.

10. Janke J, Engeli S, Boschmann M, Adams F, Bohnke J, Luft FC, Sharma AM, Jordan J. Retinol-binding protein 4 in human obesity. Diabetes. 2006. 55:2805–2810.

11. Aeberli I, Biebinger R, Lehmann R, L'Allemand D, Spinas GA, Zimmermann MB. Serum retinol-binding protein 4 concentration and its ratio to serum retinol are associated with obesity and metabolic syndrome components in children. J Clin Endocrinol Metab. 2007. 92:4359–4365.

12. Lee DC, Lee JW, Im JA. Association of serum retinol binding protein 4 and insulin resistance in apparently healthy adolescents. Metabolism. 2007. 56:327–331.

13. Cho YM, Youn BS, Lee H, Lee N, Min SS, Kwak SH, Lee HK, Park KS. Plasma retinol-binding protein-4 concentrations are elevated in human subjects with impaired glucose tolerance and type 2 diabetes. Diabetes Care. 2006. 29:2457–2461.

14. Takebayashi K, Suetsugu M, Wakabayashi S, Aso Y, Inukai T. Retinol binding protein-4 levels and clinical features of type 2 diabetes patients. J Clin Endocrinol Metab. 2007. 92:2712–2719.

15. Balagopal P, Graham TE, Kahn BB, Altomare A, Funanage V, George D. Reduction of elevated serum retinol binding protein in obese children by lifestyle intervention: association with subclinical inflammation. J Clin Endocrinol Metab. 2007. 92:1971–1974.

16. Yao-Borengasser A, Varma V, Bodles AM, Rasouli N, Phanavanh B, Lee MJ, Starks T, Kern LM, Spencer HJ 3rd, Rashidi AA, McGehee RE Jr, Fried SK, Kern PA. Retinol binding protein 4 expression in humans: relationship to insulin resistance, inflammation, and response to pioglitazone. J Clin Endocrinol Metab. 2007. 92:2590–2597.

17. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, MacIntyre NR, McKay RT, Wanger JS, Anderson SD, Cockcroft DW, Fish JE, Sterk PJ. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000. 161:309–329.
18. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000. 320:1240–1243.

19. Hong YM, Moon KR, Seo JW, Sim JG, Yoo KW, Jeong BJ, Choe YH. Nationalwide study on body mass index, skinfold thickness, and arm circumference in Korean children. J Korean Pediatr Soc. 1999. 42:1186–1200.
20. Yoon KA, Lim HS, Koh YY, Kim H. Normal predicted values of pulmonary function test in Korean school-aged children. J Korean Pediatr Soc. 1993. 36:25–37.
22. Sood A. Does obesity weigh heavily on the health of the human airway? J Allergy Clin Immunol. 2005. 115:921–924.

23. Muoio DM, Newgard CB. Metabolism: a is for adipokine. Nature. 2005. 436:337–338.
24. Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, Kotani K, Quadro L, Kahn BB. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature. 2005. 436:356–362.

25. Graham TE, Yang Q, Bluher M, Hammarstedt A, Ciaraldi TP, Henry RR, Wason CJ, Oberbach A, Jansson PA, Smith U, Kahn BB. Retinol-binding protein 4 and insulin resistance in lean, obese, and diabetic subjects. N Engl J Med. 2006. 354:2552–2563.

26. Global Initiative for Asthma. No. 95-3659. Global strategy for asthma management and prevention. Revised 2006. 1995. National Institutes of Health Publication.
27. Kim ES, Kim SH, Kim KW, Park JW, Kim YS, Sohn MH, Kim KE. Basement membrane thickening and clinical features of children with asthma. Allergy. 2007. 62:635–640.

28. Ferguson AC. Persisting airway obstruction in asymptomatic children with asthma with normal peak expiratory flow rates. J Allergy Clin Immunol. 1988. 82:19–22.

29. McFadden ER Jr, Linden DA. A reduction in maximum mid-expiratory flow rate. A spirographic manifestation of small airway disease. Am J Med. 1972. 52:725–737.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download