Abstract
The aim of this study was to determine the risk factors for nosocomial infections of imipenem-resistant Pseudomonas aeruginosa (IRPA). A prospective case-control study was performed at a tertiary care hospital in Ankara from January to December 2004. The patients with nosocomial P. aeruginosa infection were included in the study. The features of the patients with IRPA infections were compared to those with imipenem-sensitive P. aeruginosa (ISPA) infections. Only the first isolation of P. aeruginosa was considered. Nosocomial infections were defined according to Center for Disease Control (CDC) criteria. IRPA was isolated from 75 (44.1%) patients, and ISPA was isolated from 95 (55.9%) patients during the study period. IRPA were most frequently isolated from endotracheal aspirate (19%) cultures (p=0.048), whereas ISPA were most frequently isolated from urine (28%) cultures (p=0.023). In multivariate analysis, a longer duration of hospital stay until P. aeruginosa isolation (odds ratio [OR], 1.027; 95% confidence interval [CI], 1.002-1.054, p=0.034), arterial catheter administration (OR, 2.508; 95% CI, 1.062-5.920, p=0.036), vancomycin (OR, 2.882; 95% CI, 1.130-7.349, p=0.027), piperacillin-tazobactam (OR, 6.425; 95% CI, 2.187-18.875, p=0.001), and imipenem (OR, 3.580; 95% CI, 1.252-10.245, p=0.017) treatment within the 14 days before isolation of IRPA were independently associated with imipenem resistance. It was concluded that treatment with imipenem, vancomycin and piperacillin-tazobactam were major risk factors for IRPA infections in hospitalized patients. The nosocomial occurrence of IRPA was also strongly related to the duration of hospital stay, arterial catheter administration.
Pseudomonas aeruginosa is an important nosocomial pathogen with its ability to propagate on medical devices, hospital environment and even in disinfectants. It causes high morbidity and mortality in the services of oncology, hematology, surgery, burn and intensive care units (1). Infections due to this virulent organism are difficult to both control and treat because of intrinsic resistance to many antimicrobial agents (2, 3).
Imipenem, a broad-spectrum β-lactam antibiotic, is one of the most effective drug against P. aeruginosa. The incidence of imipenem-resistance is increasing among gram negative bacilli, particularly P. aeruginosa, often associated with resistance to other antipseudomonal drugs (4). The increasing resistance of P. aeruginosa is a growing threat to the clinical management of such infections (5-7).
P. aeruginosa infections are frequently encountered in Turkish hospitals with resistance to the antimicrobial agents commonly used against such bacterial infections (8). In this study, we investigated the risk factors for nosocomial infections of imipenem-resistant P. aeruginosa (IRPA).
A prospective case-control study was conducted at Ankara Numune Education and Research Hospital (ANERH) in Turkey. ANERH is an 1,100-bed referral and tertiary-care hospital. The hospital contains all major services except pediatric department, including medical and surgical sub-specialties, medical and surgical intensive care units (ICUs). The annual number of discharges was 55,422 in 2004.
An antibiotic restriction policy has been carrying out in ANERH since January 1999. The restriction is on the orders of certain antibiotics; prior consultation with an infection disease (ID) specialist is required for ceftazidime, cefepime, imipenem, meronem, ticarcilin-clavulanate, piperacillin-tazobactam, cephaperazon-sulbactam, intravenous quinolones, intravenous aminoglycosides, linezolid, vancomycin, and teicoplanin.
A prospective surveillance was conducted. All patients, who had nosocomial P. aeruginosa infection at any site, were included in the study from January to December 2004. Patients were excluded from the study if P. aeruginosa had been isolated within 48 hr of admission and younger than 16 yr of age.
Only the first P. aeruginosa isolate from each patient was evaluated. The clinical significance (colonization or infection) of each P. aeruginosa isolate and the type of infection were assessed according to the Center for Disease Control (CDC) criteria by infectious disease specialists (9). Urinary tract infection in a patient with an indwelling bladder catheter was diagnosed with detection of pyuria (≥10 leukocytes/µL), growth of ≥105 CFU/mL bacteria (no more than two species) in urine culture and clinical signs of infection (fever ≥38℃, leukocytosis, abnormal macroscopic appearance of urine, presence of urinary nitrite). In patients assisted by mechanical ventilation, pneumonia was defined when a new or progressive infiltrate or consolidation in chest radiography in the presence of purulent tracheal secretions, supported by a growth of ≥105 CFU/mL bacteria in a quantitative culture of deep endotracheal aspirate. For non-ventilated patients, the diagnosis of nosocomial pneumonia was considered when they had a compatible chest radiography and purulent sputum, with Gram's stain and sputum culture documenting the presence of a pathogen microorganism. Surgical site infection was defined as the presence of purulent drainage, and positive clinical findings (pain, tenderness, localized swelling, redness or heat at the site of incision, spontaneously opening of the incision) supported by the microbiologic analysis of specimens. Sepsis was diagnosed by presence of sepsis criteria and positive blood cultures. Patients colonized with P. aeruginosa were excluded.
Data were extracted to individual forms for each patient. The form included age, sex, diagnosis, date of admission to hospital or ICU, hospitalization before ICU, length of hospital and ICU stay, transfer from another hospital, comorbidity (renal failure, hepatic failure, malignancy, immunosupression, diabetes mellitus, chronic lung disease, malnutrition, or transplantation), elective or emergent surgical operation, Acute Physiological and Chronic Health Evaluation (APACHE II) score, ventilator support, physical examination findings, haematological and biochemical test results, antibiotics given to the patient, culture and antimicrobial susceptibility test results, time interval between hospital admission and isolation of the first positive P. aeruginosa culture.
Exposures to antimicrobial drugs were also explored. Prior antibiotic use was defined as at least 24 hr of therapy during the 14 days prior to isolation of the P. aeruginosa.
The patients were defined as IRPA cases (case patients) if they had IR P. aeruginosa infections and as imipenem-sensitive P. aeruginosa (ISPA) cases (control patients) if they had IS P. aeruginosa infections.
All P. aeruginosa were isolated prospectively in the microbiology laboratory of ANERH. Identification and antimicrobial susceptibility of the isolated strains were done by VITEK automated system (BioMerieux, Marcy I'Etoile, France). GNI+ panel was used for the identification and GN 528 panel for the detection of antimicrobial susceptibility. The isolates with minimum inhibitory concentration (MIC) value ≥8 µg/mL were recorded as IR and MIC value <8 µg/mL as IS. The following antibiotics were tested: amikacin, gentamicin, aztreonam, ceftazidime, cefepim, imipenem, netilmicin, ciprofloxacin, pefloxacin, piperacillin, piperacillin-tazobactam, ticarcillin, ticarcillin clavulanate, and trimethoprim-sulphamethoxazole.
Statistics were run with STATA 7.0 software package (College station, TX, U.S.A.).
Potential risk factors were analyzed by univariate and multivariate analysis. Results are expressed as mean±SD if not indicated otherwise. Student's t-test for independent and paired continuous variables and chi-square test or Fisher's exact test was used when appropriate to compare proportions. Variables with a p value of <0.05 in the univariate analysis were entered in a logistic regression model with backward selection of independent variables for multivariate analysis. A p value of <0.05 was considered significant.
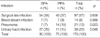
During the study period, P. aeruginosa infections were detected in 170 patients. The mean age was 48.0±20.3 and 117 (69%) were male. The mean age was 49.7±19.9 for ISPA and 45.9±20.3 for IRPA patients. Sixty-three (66.3%) of ISPA patients were male and 54 (72%) of IRPA patients were male. ICU patients accounted for 58 (34%) of the infected patients. Sixty-six percent of all patients were in clinical wards. The most frequent infection was surgical site infection (SSI) (57%), followed by urinary tract infection (22%), pneumonia (13%) and blood stream infection (8%) (Table 1).
Of the 170 patients, 75 (44.1%) had IRPA and 95 (55.9%) had ISPA infections. The frequency of IRPA infections was 1.35 cases/1,000 hospital admissions. In 29 (39%) of IRPA patients, underlying diseases were present (13 [17%] hypertension, 10 [13%] diabetes mellitus, 9 [12%] malignancy, 6 [8%] immunosuppression, 7 [9%] chronic obstructive lung disease, 5 [7%] steroid use, 2 [3%] dialysis, 2 [3%] chemotherapy, 4 [5%] coronary artery disease, 5 [7%] congestive heart disease). In 53 (56%) of ISPA patients, comorbidies were detected (24 [25%] hypertension, 22 [23%] diabetes mellitus, 17 [18%] malignancy, 13 [14%] immunosuppression, 8 [8%] chronic obstructive lung disease, 7 [7%] steroid use, 9 [10%] dialysis, 7 [7%] chemotherapy, 4 [4%] coronary artery disease, 3 [3%] congestive heart disease, 1 [1%] hepatic failure, 1 [1%] chronic alcohol consumption, and 1 [1%] splenectomy). IRPA cases had more frequently pneumonia (19% vs. 7%, p=0.048), whereas ISPA cases had more frequently urinary tract infection (28% vs. 15%, p=0.023).
The mean duration of hospital stay until P. aeruginosa isolation was 22.01±16.6 days in IRPA infections, whereas 14.06±12.7 days in ISPA infections (p<0.001). Forty-one percent of the patients with IRPA infection and 28% of the patients with ISPA infection were followed at ICU.
In ICUs IRPA infections were seen more frequently than wards (53% and 39%, respectively, p=0.078). The services from which patients with IRPA and ISPA infections were receiving care included medical wards (9% and 37%, respectively) and surgical wards (91% and 63%, respectively, p<0.001).
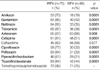
Results of the univariate analysis of risk factors for IRPA are outlined in Table 2. According to the univariate analysis, stay in surgical service (p=0.001), stay in burn unit (p<0.001), transfer from other services (another clinical service, another intensive care unit, another hospital) (p=0.034), longer duration of hospital stay until infection (p<0.001), tracheostomy (p=0.021), arterial line (p=0.012), mean APACHE-II score (p=0.026), APACHE-II score ≥20 (p=0.042) and previous use of amikacin (p=0.025), vancomycin (p=0.001), piperacillin-tazobactam (p=0.007), and imipenem (p=0.002) were significant risk factors for IRPA infections.
In a logistic regression model, a longer duration of hospital stay until P. aeruginosa isolation (odds ratio [OR], 1.027; 95% confidence interval [CI], 1.002-1.054, p=0.034), arterial catheter administration (OR, 2.508; 95% CI, 1.062-5.920, p=0.036), vancomycin (OR, 2.882; 95% CI, 1.130-7.349, p=0.027), piperacillin-tazobactam (OR, 6.425; 95% CI, 2.187-18.875, p=0.001), and imipenem (OR, 3.580; 95% CI, 1.252-10.245, p=0.017) treatment within the 14 days before isolation of IRPA were independently associated with imipenem resistance (Table 3).
Previous use of amikacin, vancomycin, imipenem and piperacillin-tazobactam was present in 15%, 33%, 26%, and 22% of the patients with IRPA and 5%, 10%, 8%, and 7% of the patients with ISPA infection, respectively.
The resistance rates of IRPA isolates to the other antibiotics were frequently higher than those ISPA isolates (Table 4). Eleven (6.4%) of the P. aeruginosa isolates were resistant to all tested antibiotics.
Four patients whose initial isolates were imipenem-susceptible were subsequently recovered to be imipenem-resistant during the same hospital stay. All of these patients had received imipenem between the isolations.
There was no outbreak due to P. aeruginosa during the study period.
P. aeruginosa is one of the most common hospital-acquired gram-negative pathogens (10, 11). Because of increase of imipenem resistance, studies were done to determine the risk factors for IRPA infections (6, 8, 12, 13). Generally, these studies were retrospective and some of them included a limited number of patients (12, 13). Besides, they might have some limitations in the exclusion of colonized patients. In a recent study, a comparative approach of two case-control studies with distinct control groups was used (6). In this study, we have done a prospective case-control study with detailed evaluation of many risk factors including physical examination of cases by an infectious disease specialist.
In this study, the frequency of IRPA infections was 1.35 cases/1,000 hospital admissions and among the P. aeruginosa infections imipenem resistance was observed as 44.1%. Although there was no similar published studies to compare the incidence of patients with IRPA, the overall incidence of IRPA infection/colonisation in Turkey was reported approximately 19% in 1997 and 13% in 1998 (14). This two to three-fold increase reflecting the striking rise in imipenem resistance in our country correlates to other reports notifying this issue (4-7, 15). In ICUs approximately two-fold increase in imipenem resistance of the P. aeruginosa isolates was observed (53.4%), when compared to another study (21% in 1997, 27% in 1998) from our country (14). Some studies found ICU exposure as a risk factor for imipenem resistance in P. aeruginosa (12, 16-18). However, supporting the findings of Troillet et al. and Zavascki et al., ICU stay was not predictive of resistance of P. aeruginosa to imipenem in our study (6, 13). Sex and age were not risk factors for IRPA infections in our study, which was compatible with other studies (6, 8, 13).
Multivariate analysis showed that, a longer duration of hospital stay until P. aeruginosa isolation (OR, 1.027; 95% CI, 1.002-1.054, p=0.034), arterial catheter administration (OR, 2.508; 95% CI, 1.062-5.920, p=0.036), vancomycin (OR, 2.882; 95% CI, 1.130-7.349, p=0.027), piperacillin-tazobactam (OR, 6.425; 95% CI, 2.187-18.875, p=0.001), and imipenem (OR, 3.580; 95% CI, 1.252-10.245, p=0.017) treatment within the 14 days before isolation of IRPA were independently associated with imipenem resistance.
A longer hospital stay identified as a risk factor in this study was similar to the other studies (12, 13, 17, 19). It is a well known risk factor for many antibiotic-resistant microorganisms (16). Antibiotic-susceptible microorganisms in body flora of the hospitalized patients can be replaced with antibiotic resistant strains which are available at hospital environment over time. Due to flora changes, prolonged hospital stay is a risk factor in all units and all types of nosocomial infections (20).
The risk of IRPA infection was 2.5 times higher for arterial catheter administration in this study. Although this has not been reported previously, identification of arterial catheter as a risk factor is not an unexpected finding. As most of the patients with IRPA infections are critically ill, they are subject to invasive procedures such as arterial catheter, endotracheal tube, central venous catheter and urinary catheter.
Antibiotic exposure remains one of the most important risk factor for the acquisition of IRPA infection (19). In this study, prior antibiotic use was defined as at least 24 hr of therapy during the 14 days prior to isolation of the P. aeruginosa. The mean days and range of previous therapy with vancomycin, piperacillin-tazobactam, and imipenem were 10.6 (2-22), 9.3 (2-34), and 11.7 (2-28), respectively. According to our results the previous use of vancomycin, piperacillin-tazobactam and imipenem were associated with imipenem resistance. The risk for imipenem resistance was 6.4 times higher in previous use of piperacillin-tazobactam, 3.5 times higher for imipenem and 2.8 times higher for vancomycin. The high risk of previous use of piperacillin-tazobactam for imipenem resistance was especially striking in our study.
Except a recent study (17), imipenem has been identified as a major risk factor for IRPA in previous studies (6, 12, 16). Using control patients with ISPA, Troillet et al. identified imipenem as the only antibiotic associated with IRPA and reported the highest OR (OR, 23.2; 95% CI, 4.1-132.7) (13). With a similar control group, Zavascki et al. also reported carbapenem as the only antibiotic associated with the risk of IRPA (OR, 12.82; 95% CI, 3.99-41.23) (6). The lower OR for imipenem was found in our study is similar to the study of Harris et al. (OR, 4.96; 95% CI, 2.88-8.57) (12). Despite the strength of this association, imipenem exposure can explain only 26% of the imipenem resistance in initial isolates. In contrast, among the patients who had initially susceptible and subsequent resistant isolates recovered, all were exposed to imipenem.
The association between previous piperacillin-tazobactam use and IRPA in this study has been only identified previously by Harris et al. (12). We noted a higher OR 6.425 (95% CI, 2.187-18.875, p=0.001) for piperacillin-tazobactam than that found in the study of Harris et al. (OR, 2.19; 95% CI, 1.42-4.03). The treatment with other β-lactam antibiotics have been thought to predispose for imipenem resistance by selecting strains with stably depressed β-lactamase production, which could then be more likely to lose their porin OprD2 (21).
Our study showed vancomycin as a significant risk factor. Harris et al. also reported vancomycin as a risk factor for IRPA isolation (12). On the other hand, Zavascki et al. reported that the combination of carbapenem and vancomycin significantly increased the risk of imipenem resistance. However, they did not confirm this finding in their second study model with the control group of ISPA. It has been hypothesized that vancomycin may select for Pseudomonas species by destroying competing gram-positive bacteria that are part of enteric or bronchial flora (6). In this study, previous use of combined treatment of vancomycin plus imipenem was not independently associated with imipenem resistance.
The isolates of IRPA were often multidrug resistant causing a difficulty in the treatment and control of these infections. Eleven (6.4%) of the P. aeruginosa isolates were resistant to all tested antibiotics in this study. Antimicrobial resistance rates of IRPA were high (≥70%) for amikacin, gentamicin, netilmicin, tobramicin, aztreonam, cefepime, ciprofloxacin, pefloxacin, ticarcillin/clavulanate, and trimethoprim/sulphamethoxazole. Imipenem resistance was frequently associated with resistance to other common antipseudomonal agents (Table 4). The lack of association between imipenem and ceftazidime resistance can be explained by rare prescription of ceftazidime in our hospital.
Solid organ transplantation, mechanical ventilation and renal failure have been identified as risk factors in different studies (6, 13, 18, 19). In our study, we did not identify them as risk factors for IRPA. Besides, we could not confirm the results of the National Nosocomial Infections Surveillance system study that found that respiratory tract culture specimens were predictive of resistance of P. aeruginosa to imipenem.
Two limitations were present in this study. Our study was not based on molecular epidemiologic investigation. The other was the limited number of IRPA cases in this study, although 75 cases of IRPA were investigated.
In conclusion, our results suggest that the nosocomial occurrence of IRPA infections is strongly related to longer duration of hospital stay and arterial catheter administration. Prior uses of imipenem, vancomycin and piperacillin-tazobactam were independent risk factors for nosocomial IRPA infections. Considering the high rate of IR in P. aeruginosa infections in this study, we should carefully reconsider the whole prevention and control measures.
Figures and Tables
Table 1
Nosocomial infection sites caused by imipenem-sensitive P. aeruginosa (ISPA) and imipenem-resistant P. aeruginosa (IRPA)
References
1. Fluit AC, Verhoef J, Schmitz FJ. Antimicrobial resistance in European isolates of Pseudomonas aeruginosa. European SENTRY Participants. Eur J Clin Microbiol Infect Dis. 2000. 19:370–374.
2. Quinn JP. Imipenem resistance among gram-negative bacilli. Eur J Clin Microbiol Infect Dis. 1994. 13:203–204.

3. Carmeli Y, Troillet N, Eliopoulos GM, Samore MH. Emergence of antibiotic-resistant Pseudomonas aeruginosa: comparison of risks associated with different antipseudomonal agents. Antimicrob Agents Chemother. 1999. 43:1379–1382.

4. Fridkin SK, Steward CD, Edwards JR, Pryor ER, McGowan JE Jr, Archibald LK, Gaynes RP, Tenover FC. Surveillance of antimicrobial use and antimicrobial resistance in United States hospitals: project ICARE phase 2. Project Intensive Care Antimicrobial Resistance Epidemiology (ICARE) hospitals. Clin Infect Dis. 1999. 29:245–252.
5. Deshpande LM, Fritsche TR, Jones RN. Molecular epidemiology of selected multidrug-resistant bacteria: a global report from the SENTRY Antimicrobial Surveillance Program. Diagn Microbiol Infect Dis. 2004. 49:231–236.

6. Zavascki AP, Cruz RP, Goldani LZ. Risk factors for imipenem-resistant Pseudomonas aeruginosa: a comparative analysis of two case-control studies in hospitalized patients. J Hosp Infect. 2005. 59:96–101.

7. King A, Shannon K, Phillips I. Resistance to imipenem in Pseudomonas aeruginosa. J Antimicrob Chemother. 1995. 36:1037–1041.

8. Akinci E, Colpan A, Bodur H, Balaban N, Erbay A. Risk factors for ICU-acquired imipenem-resistant Gram-negative bacterial infections. J Hosp Infect. 2005. 59:317–323.
9. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988. 16:128–140.

10. Fluit AC, Jones ME, Schmitz FJ, Acar J, Gupta R, Verhoef J. Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY antimicrobial surveillance program, 1997 and 1998. Clin Infect Dis. 2000. 30:454–460.

11. Pfaller MA, Jones RN, Doern GV, Kugler K. Bacterial pathogens isolated from patients with bloodstream infection: frequencies of occurrence and antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob Agents Chemother. 1998. 42:1762–1770.

12. Harris AD, Smith D, Johnson JA, Bradham DD, Roghmann MC. Risk factors for imipenem-resistant Pseudomonas aeruginosa among hospitalized patients. Clin Infect Dis. 2002. 34:340–345.

13. Troillet N, Samore MH, Carmeli Y. Imipenem-resistant Pseudomonas aeruginosa: risk factors and antibiotic susceptibility patterns. Clin Infect Dis. 1997. 25:1094–1098.
14. Yapar N, Erdenizmenli M, Gülay Z, Küçükgüven Biçmen M, Yüce A, Yuluğ N. Pseudomonas aeuroginosa, Acinetobacter ve Staphylococcus Turlerinin Antibiyotik Direnci. Turk J Infect. 2000. 14:507–509.
15. National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004. 32:470–485.
16. Gaynes RP, Culver DH. Resistance to imipenem among selected Gram-negative bacilli in the United States. Infect Control Hosp Epidemiol. 1992. 13:10–14.

17. Lautenbach E, Weiner MG, Nachamkin I, Bilker WB, Sheridan A, Fishman NO. Imipenem resistance among pseudomonas aeruginosa isolates: risk factors for infection and impact of resistance on clinical and economic outcomes. Infect Control Hosp Epidemiol. 2006. 27:893–900.

18. Aloush V, Navon-Venezia S, Seigman-Igra Y, Cabili S, Carmeli Y. Multidrug-resistant Pseudomonas aeruginosa: risk factors and clinical impact. Antimicrob Agents Chemother. 2006. 50:43–48.

19. Fortaleza CM, Freire MP, Filho Dde C, de Carvalho Ramos M. Risk factors for recovery of imipenem- or ceftazidime-resistant Pseudomonas aeruginosa among patients admitted to a teaching hospital in Brazil. Infect Control Hosp Epidemiol. 2006. 27:901–906.

20. Erol S, Altoparlak U, Akcay MN, Celebi F, Parlak M. Changes of microbial flora and wound colonization in burned patients. Burns. 2004. 30:357–361.

21. Satake S, Yoneyama H, Nakae T. Role of OmpD2 and chromosomal beta-lactamase in carbapenem resistance in clinical isolates of Pseudomonas aeruginosa. J Antimicrob Chemother. 1991. 28:199–207.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download