Abstract
A nationwide questionnaire-based survey was performed to evaluate the current clinical practices for the management of neutropenic fever in hematology units and hematopoietic stem cell transplantation (HSCT) centers throughout Korea. A 86.9% response rate was obtained from a total of 46 doctors and practical policies of the 33 sites were analysed. Approximately 42.4% and 84.8% of the sites responded that they used oral fluoroquinolone as prophylaxis for neutropenic patients receiving chemotherapy and HSCT, respectively. Additionally, 42.4% of the sites responded that they used antifungal prophylaxis in the chemotherapy groups whereas 90.9% of the sites responded that they used antifungal prophylaxis in HSCT recipients. Approximately half of the responding sites prescribed combination regimen with 3rd or 4th cephalosporin plus aminoglycoside as a first-line therapy. Most of the sites considered persistent fever for 2-4 days or aggravated clinical symptoms for 1-2 days as failure of the first-line regimen, and they changed antibiotics to second-line regimens that varied widely among the sites. Twenty-seven sites (84.4%) responded that they considered adding an antifungal agent when fever persisted for 5-7 days despite antibacterial therapy. Amphotericin B deoxycholate was preferred as a first-line antifungal, which was probably due to the limitations of the national health insurance system. The role of oral antibiotics in the management of neutropenic fever still accounted for a small portion. To the best of our knowledge, this survey is the first report to examine the practical policies currently in place for the management of neutropenic fever in Korea and the results of this survey may help to establish a Korean guideline in the future.
Due to the development of new anti-cancer drugs and new treatment techniques, as well as many advances in the field of stem cell transplantation and better supportive care, many malignancies can now be treated more effectively. However, neutropenia and infectious complications that inevitably develop following chemotherapy, continue to be a frequent cause of morbidity and mortality. Neutropenic fever is a potentially life-threatening complication that requires prompt medical intervention. Therefore, empirical antimicrobial therapy without waiting for microbiological and/or clinical documentation of an infection is justified in patients with neutropenic fever. Because of this, a practical treatment guideline suitable for the conditions unique to Korea is required. However, it is important to ensure that this guideline takes into account the microbiologic epidemiology, antimicrobial resistance patterns and currently available antimicrobial drugs, while also considering economic issues.
In Korea, there are currently 36 hematopoietic stem cell transplantation (HSCT) centers, in which curative treatments for hematologic diseases have been performed over 20 yr. Nevertheless, a Korean guideline for the treatment of neutropenic fever has not been established yet. And the guideline produced by the Infectious Diseases Society of America (IDSA) has primarily been used. However, this guideline was established on conditions unique to the Unites States. Therefore, its application in Korea, causes many problems. For example, differences are caused by general factors, such as characteristic racial factors and the socio-cultural environmental factors. In addition, the local medical system and insurance coverage criteria are different. In more detail, the types of licensed antimicrobials and approved ranges and dosages are different. For these reasons, countries other than the U.S.A., such as Germany, France, Italy, and Japan, have begun to prepare guidelines specific to their own country (2-5). Therefore, we have performed this nationwide survey to define the current clinical practices in place for the management of neutropenic fever in each HSCT center and hematologic unit in Korea as a first step towards the development of guideline that is suitable for the actual circumstances of our country.
A questionnaire was sent out to selected hematologists and infectious disease specialists in each HSCT center and hematology unit in Korea. The survey was designed to assess the practical policies currently in place with respect to the definition of neutropenic fever, prophylactically and empirically used antimicrobials. In addition, the definition of treatment failure and the indications for colony stimulating factor (CSF) treatment and granulocyte transfusion used for the management of neutropenic fever at each site were also asked. When different guidelines were applied between the chemotherapy group and HSCT group, it was recorded separately to distinguish them. The letter accompanying the questionnaire stressed that the answers should be based on local unit policies and not on personal opinions. This survey was conducted between December 2005 and February 2006. If there were different answers between the hematologist and infectious disease specialist from a center, we verified the data through direct contact by e-mail or telephone to the responsible person in charge. And practical policies were investigated for each of adult and pediatric patients at HSCT centers or hematologic units (from here on, the word 'site' refers to the HSCT center and hematology unit). The results were entered into SPSS 13.0 (SPSS Korea, Seoul, Korea) and analyzed using the accompanying software.
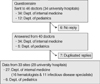
Questionnaire was sent to 46 doctors (34 that belonged to the department of internal medicine and 12 that belonged to the department of pediatrics) at 34 university hospitals, and 40 (86.9%) of the doctors (34 from the department of internal medicine and 6 from the department of pediatrics) responded. Thirty-four replies from the department of internal medicine included duplicated answers from hematologists and infectious disease specialists at 7 HSCT centers. After verification of the data, practical policies of the 33 sites were obtained from 28 university hospitals throughout Korea (Fig. 1).
Twenty-seven (81.8%) of the 33 sites that responded had their own policies regarding the treatment of neutropenic fever, however most of the sites (21/33, 77.8%) based their policies on the IDSA guideline, and only 5 sites (18.5%) used guidelines that they had prepared based on their own microbiologic data. Thirteen of the sites (39.4%) approached the treatment of neutropenic fever by dividing patients into the high risk group and the low risk group; however, only 3 of these sites actually administered oral antibiotics to the low risk group.
The currently used definition of neutropenic fever varied among the sites. Neutropenia was defined as the presence of a neutrophil count of <500 cells/µL or a neutrophil count of <1,000 cells/µL that was predicted to decrease to <500 cells/µL by 31 sites (93.9%). However, fever was defined as a single temperature of ≥38.0℃ or a temperature of ≥38.0℃ for >1 hr by 20 sites (60.6%), whereas 2 separate temperature of ≥38.0℃ or a temperature of ≥38.0℃ for >1 or 2 hr was used to define fever in 6 sites (18.2%), and a single temperature of ≥38.3℃ was used in 4 sites (12.1%). Three sites (9.1%) considered ≥37.8℃ as fever. Another point to be considered was that only 2 sites (6.0%) measured the oral temperature as specified in the IDSA guideline, whereas most sites measured the axillary or tympanic membrane temperature (31/33, 93.9%). Also, definition of the fever was not differently applied according to the measured sites.
Antimicrobial prophylaxis was administered to chemotherapy patients in 19 sites (57.6%). Both antibacterial and antifungal prophylaxis was done in 12 sites (36.4%). Two sites (6.1%) prescribed only an antibacterial agent and another 2 sites administered only antifungal agents to chemotherapy groups. Furthermore, 3 sites (9.1%) provided only anti-pneumocystis prophylaxis and 1 sites provided anti-tuberculous prophylaxis with isoniazid (300 mg/day) to patients who had a past history of tuberculosis and a suspicious lesion on radiography. Oral ciprofloxacin and levofloxacin were used as antibacterial agents in 11 and 3 sites, respectively.
When the HSCT group was considered, it was found that antimicrobial prophylaxis was done in 30 sites (90.9%). Antibacterial agents were prescribed in 28 sites (84.8%). Oral ciprofloxacin was used as the antibacterial agent in 20 of the sites (60.6%), whereas oral levofloxacin was used in 5 of the sites (15.2%). In addition, roxithromycin or a combination of either ciprofloxacin plus metronidazole or ycin plus colimycin (colistimethate sodium) was used orally in 1 site each. Antifungal prophylaxis was done in 30 sites (90.9%), with oral fluconazole or itraconazole being administered in 25 of 28 sites that responded to the question, and amphotericin B deoxycholate or nystatin also being administered in 3 sites (data were not mutually exclusive). Twenty-one sites (63.6%) used oral acyclovir for antiviral prophylaxis, whereas intravenous (IV) acyclovir was used in 5 sites (15.2%), and ganciclovir was used in 2 sites. Co-trimoxazole was prescribed for pneumocystis prophylaxis in 29 sites (87.9%) and it was coupled with pentamidine inhalation in one site. Anti-tuberculous prophylaxis with isoniazid was done in 3 sites; however different doses were used among the sites (dose, 300-400 mg/day, or 10 mg/kg/day).
The most commonly prescribed regimen for empirical antibiotic therapy of neutropenic fever was one cephalosporin (ceftazidime or cefepime) plus one aminoglycoside in 50.0% and 43.7% of the chemotherapy and HSCT group, respectively (Table 1). Overall, combination regimen using an aminoglycoside plus either cephalosporin, carbapenem or an antipseudomonal penicillin was used as empirical therapy in 71.9% and 65.6% of the chemotherapy and HSCT group, respectively. Additionally, carbapenem monotherapy was used as an initial empirical therapy in one site for the HSCT group.
As for glycopeptides, ycin was used at 17 sites (51.5%), whereas teicoplanin was used at 10 sites (30.3%), and both were used at 6 sites (18.2%). A glycopeptide was routinely prescribed as part of an initial empirical therapy in only 2 out of 22 sites that responded to the question, which suggested that most sites do not feel that glycopeptide was a necessary part of the initial regimen. In 19 (86.4%) of the 22 sites that responded to the question, glycopeptide was started for selected patients based on the IDSA guideline. And 21 out of 32 sites (65.6%) that answered the question stated that they stopped glycopeptide when an absolute neutrophil count (ANC) was recovered over 500 cells/µL and any sign of infection by gram positive organisms disappeared. Additionally, in 7 out of 32 sites (21.9%), glycopeptide was discontinued immediately when signs and symptoms of infection induced by gram positive organisms disappeared regardless of ANC.
Table 2 shows the criteria used for changing the initial empirical regimen. Most of sites considered persistent fever for 2-4 days or aggravated clinical symptoms for 1-2 days as failure of the first-line antibiotics. Table 3 shows the antibacterial agents that were prescribed as second-line regimens. The most common approach was to add a glycopeptide regardless of signs of gram positive infection and change to the second-line regimens. The second-line regimens were as follows: carbapenem with or without aminoglycoside was considered for cases in which cephalosporin or piperacillin/tazobactam was used as the first-line regimen, and cefepime, ceftazidime, or piperacillin/tazobactam with or without aminoglycoside was used for cases in which piperacillin was used as the first-line regimen.
Table 4 presents the conditions under which antifungal therapy was started. Twenty-seven sites (84.4%) considered adding an antifungal agent after 5-7 days of persistent fever despite antibacterial therapy. And 14 sites initially prescribed antifungal agents to the patients who had a history of invasive fungal infection during a previous chemotherapy. Table 5 shows the first-line antifungal agents used for treatment of persistent neutropenic fever. In cases receiving antifungal prophylaxis, amphotericin B deoxycholate or IV itraconazole were used as the antifungal agents of choice in 25 of 26 sites that responded. Whereas, in cases without antifungal prophylaxis, they were the agents of choice in 17 of 18 sites that responded. Out of 18 sites that responded the rank of preference, 12 sites used amphotericin B as the first-line antifungals and 6 sites used IV itraconazole as the first-line antifungals. Twenty-two sites responded that they switched to the second-line antifungal agents if persistent fever or deterioration of radiological findings occurred after administration of the first-line antifungal agents for 7-10 days. They responded a great variety of second-line antifungal angents such as caspofungin, voriconazole, itraconazole IV, Amphotericin B deoxycholate, liposomal amphotericin B, and fluconazole (only in cases of candidemia).
Empirical antiviral therapy was conducted at 20 sites (60.6%), 17 of which responded that they administered acyclovir in cases of vesicular skin eruption suspicious herpesvirus infection or intractable oral ulcer. Three sites responded that they prescribed acyclovir in cases of unspecified interstitial pneumonia or encephalitis accompanying a change in mental status.
CSF therapy was routinely administered at 21 sites (63.6%) under the following conditions; 1) when the ANC was <500/µL in 15 sites (71.7%), 2) at a defined time after chemotherapy or HSCT regardless of ANC in 2 sites (9.5%), 3) depending on regimen in 2 sites (9.5%), and 4) other reasons in 2 sites (9.5%).
Granulocyte transfusion was used in 14 sites (42.4%) under the following conditions: 1) when refractory infection occurred despite optimal antimicrobial therapy and neutropenia persisted (10 sites, 71.4%), 2) 1) plus reversibility of neutropenia (2 sites, 14.3%), and 3) 1) plus localized infection (2 sites, 14.3%)
Most sites terminated antimicrobial therapy when recovery of neutropenia was coupled with the disappearance of fever (Table 6). Additionally, six sites (18.1%) reported that antibiotics were terminated regardless of ANC when signs and symptoms of infection disappeared. However, the afebrile period required to stop antibiotics varied from 2 days to 14 days.
In Korea, HSCT has been performed in more than 5,000 patients since it was first conducted in 1983. In 2006, approximately 1,300 patients received HSCT and this number is expected to continue to rise (personal communication with Korean Stem Cell Transplantation Nurses Association). However, there is no nationwide database system currently available for the collection and analysis of data. Therefore, it is difficult to establish a national consensus for the antimicrobial treatment of neutropenic fever following HSCT and chemotherapy. In the late 90s, a survey entitled, 'the appropriateness of the therapeutic use of antibiotics in patients with neutropenic fever' was conducted in Korea (6). That survey, however, only evaluated the antibiotics used empirically for neutropenic fever at 15 hospitals and then simply compared the result with guidelines of other countries. In addition, the survey did not assess the practical policies comprising the overall management of neutropenic fever. In 2003, efforts were made to establish a Korean guideline for the treatment of neutropenic fever by the Korean Society of Chemotherapy. However, an evidence-based guideline could not be established due to insufficient data studied within our country. Therefore, they had suggested a recommendation based on already existing guidelines such as IDSA at that time. So, this study is the first nationwide attempt to survey the overall practical policies regarding the management of neutropenic fever at hematology units or HSCT centers in Korea.
The results of this survey showed that oral fluoroquinolones are now widely used as prophylaxis in neutropenic patients. We found that 57.6% and 90.9% of patients who underwent chemotherapy and HSCT received antimicrobial prophylaxis, respectively. A recent meta-analysis found that fluoroquinolone prophylaxis reduced all-cause mortality in neutropenic patients with hematologic malignancy when compared to patients that did not receive antibiotic prophylaxis (7). However, ciprofloxacin is known to be an independent risk factor for the acquisition of methicillin resistant Staphylococcus aureus (8), and it is also believed that it is contributing to an increase in fluoroquinolone resistance among Escherichia coli that has already been observed in Korea (9, 10). So, it is necessary to define criteria such as to whom give the oral prophylaxic antibiotics-e.g., patients who were suspected to have prolonged neutropenia for more than 7 days.
Although recent meta-analyses have indicated that the use of antibiotic monotherapy (11, 12) or oral antibiotics is effective for patients with neutropenic fever at low risk (13, 14), the most commonly used empirical regimen for neutropenic fever is 3rd or 4th generation cephalosporin (ceftazidime or cefepime) in combination with aminoglycosides. Monotherapy was conducted in only 20% of the sites and oral antibiotics were used in only 9.1% of the sites that responded to this survey. This is probably because prophylactic oral antibiotics had already been administered to most patients, which might lead to the belief that oral antibiotics could not be administered to patients that developed fever. However, the low cost of hospitalization in Korea compared with that of other countries, coupled with the emotional trait of patients and doctors' desire to avoid ambulatory treatments at outpatient clinics may also play a role in the choice of IV antibiotics. Therefore, carefully designed studies are needed to specify the conditions under which outpatient therapy is an acceptable and perhaps preferred choice for neutropenic fever in our country. The results of this survey also showed that only 2 sites (6.2%) routinely used a glycopeptide at the beginning of empirical therapy. These results are similar to those of a multicenter study (15) that failed to demonstrate that the addition of empirical ycin was beneficial, as well as to the results of a recent meta-analysis, which concluded that it is safe to defer the use of glycopeptides until a resistant gram-positive organism is documented (16). As we knew that the criteria to define fever and measuring methods were diverse among the sites and even within a site, a future guideline should include practically applicable criteria which clearly state these points. In addition, it should be kept in mind that empirical antibiotics should be initiated regardless of fever if signs or symptoms of infection are present (1). If the clinical course of patients deteriorates within 1-2 days or fever persists after 2-4 days of first-line empirical antibacterial therapy, most sites considered switching antibiotics to the second-line regimens, which were very diverse as shown in Table 3.
Most of the sites (84.4%) responded that empirical antifungal therapy was considered if fever persisted more than 5-7 days of broad spectrum antibacterial therapy. Liposomal amphotericin B was recommended by several evidence-based guidelines (1-3, 17) and caspofungin was approved for the persistent neutropenic fever by the Food and Drug Administration (FDA) (18). Itraconazole was also approved as a first-line empirical antifungals for the persistent neutropenic fever by Korean FDA. On the other hand, amphotericin B deoxycholate causes many adverse events including infusion related toxicities, nephrotoxicity, other chronic reactions such as nausea, anorexia, vomitin, etc. Nevertheless, amphotericin B deoxycholate has been the drug of choice because its broad spectrum, low cost and coverage by medical insurance were firstly considered when doctors determined a course of antifungal treatment. However, pharmaco-economic studies including cost-effectiveness during the entire treatment period should be conducted. And the selection based not only on the daily cost of drugs, but on the cost-effectiveness data supported by pharmaco-economic study, should be made. Additionally, because of the wide variety of antifungal agents used for the second-line regimen, a more comprehensive and structural survey dealing with antifungal agents should be conducted in the future.
Regarding the administration of CSF and granulocyte transfusion, it appeared to be performed under similar criteria as other countries (19-21). Although the effectiveness of granulocyte transfusion was limited, a favorable response was observed in approximately 60% of cases in whom it is used (22). Because cases requiring granulocyte transfusion are increasing gradually, further studies should be conducted to determine under what conditions it should be used.
It was difficult to arrange the data because there were many differences in the policies between hematologists and infectious disease specialists who even belonged to the same sites. These differences might have occurred because the infectious disease specialists were actively involved in the management of febrile neutropenic patients in some centers, but not in the others. Additionally, the differences in their opinions might have occurred because the doctors looked at the patients from their own special point of view. Because neutropenic fever is an important problem to both hematologists and infectious disease specialists, members of these two fields should always communicate closely with each other when they treated patients as well as they decided upon new treatment strategy.
In conclusion, oral fluoroquinolones were widely used for the prophylaxis of neutropenic fever and combination of a cephalosporin such as ceftazidime or cefepime plus an aminoglycoside was commonly used as a first-line therapy for neutropenic fever in Korea. Although this first-line regimen was common, very diverse protocols were used among the sites. However, it should be noted that this survey did not take into account selection of treatment regimens based on microbiologic data generated at each site, and therefore, additional surveys should be accompanied. As a result of these series of process, an evidence-based guideline specific to our country could be prepared and standardization at a certain level might be possible among the sites. We hope that the results of this survey may help to establish a Korean guideline in the future.
Figures and Tables
Table 3
Second-line antibiotics prescribed to patients who did not respond to the initial empirical regimen

ACKNOWLEDGMENTS
This work was supported in part by The Korean Society of Immunocompromised Host Infections (KSIHI). We thank the hematologists and infectious diseases specialists of the following institutions that participated in this survey for their contributions: Ajou University Hospital, Catholic University St. Mary's Hospital, Chonbuk National University Hospital, Chonnam National University Hospital, Chungnam National University Hospital, Daegu Catholic UNL Medical Center, Daegu Fatima Hospital, Dong-A University Medical Center, Ewha Womans University Mokdong Hospital, Gyeongsang National University Hospital, Hallym University Kangdong Sacred Heart Hospital, Hanyang University Hospital, Inje University Pusan Paik Hospital, Korea University Anam Hospital, Korea University Guro Hospital, KyungHee University Medical Center, Kyungpook National University Hospital, National Cancer Center, Pochon CHA University Bundang CHA General Hospital, Pusan National University Hospital, Seoul Asan Medical Center, Seoul National University Hospital, Soonchunhyang University Hospital, Soonchunhyang University Bucheon Hospital, Sungkyunkwan University Samsung Medical Center, Ulsan University Hospital, Yeungnam University Medical Center, Yonsei University Severance Hospital.
References
1. Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002. 34:730–751.

2. Link H, Bohme A, Cornely OA, Hoffken K, Kellner O, Kern WV, Mahlberg R, Maschmeyer G, Nowrousian MR, Ostermann H, Ruhnke M, Sezer O, Schiel X, Wilhelm M, Auner HW. Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Group Interventional Therapy of Unexplained Fever, Arbeitsgemeinschaft Supportivmassnahmen in der Onkologie (ASO) of the Deutsche Krebsgesellschaft (DKG-German Cancer Society). Antimicrobial therapy of unexplained fever in neutropenic patients. guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO), Study Group Interventional Therapy of Unexplained Fever, Arbeitsgemeinschaft Supportivmassnahmen in der Onkologie (ASO) of the Deutsche Krebsgesellschaft (DKG-German Cancer Society). Ann Hematol. 2003. 82:Suppl 2. S105–S117.
3. Biron P, Fuhrmann C, Escande MC, Blanc-Vincent MP, Crokaert F, Beal J, Bussy V, Lesimple T, Pottecher B, Raveneau J, Senet JM, Viot M. Standards, Options, and Recommendations for the management of brief neutropenias. Fedération Nationale des Centres de Lutte Contre le Cancer. Bull Cancer. 1998. 85:695–711.
4. Viscoli C, Castagnola E, Caniggia M, De Sio L, Garaventa A, Giacchino M, Indolfi P, Izzi GC, Manzoni P, Rossi MR, Santoro N, Zanazzo GA, Masera G. Italian guidelines for the management of infectious complications in pediatric oncology: empirical antimicrobial therapy of febrile neutropenia. Oncology. 1998. 55:489–500.

5. Proceedings of the consensus meeting: evidence-based recommendations on the management of febrile neutropenia in Japan. Honolulu, Hawaii, 8-9 March 2003. Clin Infect Dis. 2004. 39:Suppl 1. S1–S69.
6. Song YG, Chang KH, Kim HY, Hong SK, Park YS, Cho JH, Kim CO, Huh AJ, Park ES, Kim YS, Choi YW, Kim JM. Evaluation for appropriateness of therapeutic use of antibiotics in patients with respiratory tract infections and in patients with febrile neutropenia. J Korean Soc Chemother. 2000. 18:125–140.
7. Gafter-Gvili A, Fraser A, Paul M, Leibovici L. Meta-analysis: antibiotic prophylaxis reduces mortality in neutropenic patients. Ann Intern Med. 2005. 142:979–995.

8. Hori S, Sunley R, Tami A, Grundmann H. The Nottingham Staphylococcus aureus Population Study: prevalence of MRSA among the elderly in a university hospital. J Hosp Infect. 2002. 50:25–29.

9. Yoo JH, Huh DH, Choi JH, Shin WS, Kang MW, Kim CC, Kim DJ. Molecular epidemiological analysis of quinolone-resistant Escherichia coli causing bacteremia in neutropenic patients with leukemia in Korea. Clin Infect Dis. 1997. 25:1385–1391.
10. Lee DG, Choi SM, Choi JH, Yoo JH, Park YH, Kim YJ, Lee S, Min CK, Kim HJ, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Selective bowel decontamination for the prevention of infection in acute myelogenous leukemia: a prospective randomized trial. Korean J Intern Med. 2002. 17:38–44.
11. Furno P, Bucaneve G, Del Favero A. Monotherapy or aminoglycoside containing combinations for empirical antibiotic treatment of febrile neutropenic patients: a meta-analysis. Lancet Infect Dis. 2002. 2:231–242.
12. Paul M, Soares-Weiser K, Leibovici L. Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for fever with neutropenia: systematic review and meta-analysis. BMJ. 2003. 326:1111.

13. Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J. The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol. 2000. 18:3038–3051.

14. Vidal L, Paul M, Ben-Dor I, Pokroy E, Soares-Weiser K, Leibovici L. Oral versus intravenous antibiotic treatment for febrile neutropenia in cancer patients. Cochrane Database Syst Rev. 2004. 4:CD003992.

15. Vancomycin added to empirical combination antibiotic therapy for fever in granulocytopenic cancer patients. European Organization for Research and Treatment of Cancer (EORTC), International Antimicrobial Therapy Cooperative Group and the National Cancer Institute of Canada-Clinical Trials Group. J Infect Dis. 1991. 163:951–958.
16. Paul M, Borok S, Fraser A, Vidal L, Leibovici L. Empirical antibiotics against Gram-positive infections for febrile neutropenia: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2005. 55:436–444.

17. Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz C, Bodensteiner D, Pappas P, Seibel N, Greenberg RN, Dummer S, Schuster M, Holcenberg JS. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med. 1999. 340:764–771.
18. Walsh TJ, Teppler H, Donowitz GR, Maertens JA, Baden LR, Dmoszynska A, Cornely OA, Bourque MR, Lupinacci RJ, Sable CA, dePauw BE. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med. 2004. 351:1391–1402.

19. Kerr JP, Liakopolou E, Brown J, Cornish JM, Fleming D, Massey E, Oakhill A, Pamphilon DH, Robinson SP, Totem A, Valencia AM, Marks DI. The use of stimulated granulocyte transfusions to prevent recurrence of past severe infections after allogeneic stem cell transplantation. Br J Haematol. 2003. 123:114–118.

20. Mousset S, Hermann S, Klein SA, Bialleck H, Duchscherer M, Bomke B, Wassmann B, Bohme A, Hoelzer D, Martin H. Prophylactic and interventional granulocyte transfusions in patients with haematological malignancies and life-threatening infections during neutropenia. Ann Hematol. 2005. 84:734–741.

22. Park SH, Choi SM, Lee DG, Choi JH, Yoo JH, Shin WS, Kang MW. Efficacies and safeties on granulocyte transfusion for severe infections during neutropenic fever. Infect Chemother. 2004. 36(S2):S153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download