Abstract
The superficial brachial artery (SBA), a branch of the axillary artery, is one of the most common arterial variations in this area. While it is more vulnerable to accidental arterial injection or injury, it could be useful for the nourishment of a medial arm skin free flap. To analyze the relationship between the SBA of axillary origin and segmental variation of the axillary artery, we dissected 304 arms of Korean cadavers. We found an SBA of axillary origin in 12.2% of cadaveric arms. Unilateral occurrence was detected in 16 cadavers and bilateral in 10. SBAs gave rise to radial and ulnar arteries in the cubital fossa (8.9%), continued in the forearm as the radial artery (2.3%), or ended in the upper arm (1.0%). The SBA ended as ulnar artery was not found in any of the cadavers. The bifurcation of the SBA into the radial and ulnar arteries, presence of an SBA that ends in the upper arm, and the lack of continuation as the ulnar artery are characteristics of SBAs in Korean cadavers.
Variations in the arterial pattern of the upper limb are commonly encountered in routine dissections, and the superficial brachial artery (SBA) is one of the major variations (1-11). According to the literature, its frequency and branching pattern vary among ethnic groups.
The SBA originates from the axillary artery and runs superficial to the median nerve (12). The presence of the SBA can be hazardous because it is very vulnerable to injury (5). An accidental intra-arterial injection via the SBA can cause thrombosis or gangrene, leading to amputation of the arm or fingers (7). Conversely, the SBA can be used as a feeding artery to a free flap from medial arm skin (13). Considering these possible complications and benefits, investigations of the arterial pattern in patients' arms before any invasive procedures may be helpful in avoiding iatrogenic injury or in using an SBA for some procedures. Doppler ultrasound imaging or angiography can assist healthcare providers in treating patients with an SBA. Whether those devices are available or not, anatomical knowledge of the SBA is essential.
Since the publication of the study by Adachi et al. (1), data on the SBA in Asian populations have been rare, especially in Korean cadavers. This study was performed to provide the first large series data of the SBA in Korean cadavers.
We observed 304 extremities of 154 adult Korean cadavers (94 males, 60 females). In an anatomy lab for medical students, the upper arm was examined for variations. The upper arms suspected to have variations were further dissected. The course and branches of the SBA of axillary origin were recorded.
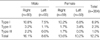
Thirty-seven SBAs emerging from the axillary artery were found in 304 Korean arms (12.2%). Unilateral occurrence was observed in 16 cadavers and bilateral occurrence in 10 cadavers. One SBA was in a cadaver which had only one arm available. The SBA had a tendency to occur more frequently on the right side but the difference had no statistical significance (p=0.22). There was also no difference in gender (p=0.96) (Table 1). In all axillae, the subscapular artery, anterior humeral circumflex artery, and posterior humeral circumflex artery arose from the axillary artery, not from the SBA.
The SBAs were classified into three types. Type I: the SBA bifurcated into the radial and ulnar arteries in the cubital fossa after giving off muscular branches to the biceps brachii and brachialis muscles (Fig. 1). The anterior and posterior interosseous arteries arose either separately or as a common trunk from the ulnar artery. The ulnar artery ran under the flexor carpi ulnaris muscle. The axillary artery became the (definitive) brachial artery to end as a collateral branch around the elbow. This pattern was observed in 27 arms (8.9%).
We further divided Type I SBA into three subtypes (Fig. 2). Type Ia: the SBA emerged proximal to the stem of the subscapular artery, anterior humeral circumflex artery, and posterior humeral circumflex artery (Fig. 2A). Type Ib: the SBA emerged from the axillary artery distal to the stem of the subscapular artery, proximal to the stems of the humeral circumflex arteries. In this type, the subscapular artery arose from the second part of the axillary artery, not third (Fig. 2B). Type Ic: the SBA emerged after the direct appearance of the thoracodorsal artery from the second part of the axillary artery. The circumflex scapular artery appeared from the third part of the axillary artery, distal to the stem of the SBA (Fig. 2C). The proportions of Type Ia, Ib, and Ic were 54.2%, 33.3%, and 12.0% of total Type I, respectively.
Type II SBA (i.e. superficial radial artery) was found on seven sides (2.3%). This artery continued as the radial artery after branching off into muscular branches to the biceps brachii and brachialis muscles (Fig. 3).
In Type III, the slender superficial brachial artery supplied the arm musculature and ended in the arm (Fig. 4). It was found in three cases (1.0%).
In normal morphogenesis, the superficial brachial artery is not an erroneous variation but an essential blood vessel. The SBA is an important vessel in fetal life for replacing or supporting the definitive brachial artery (11). Rodríguez-Baeza et al. (14) suggested that the hemodynamic predominance of certain arterial segments during development determines whether the SBA will remain.
The SBA emerges from the axillary artery during stage IV of upper limb vascular development (5). It is joined to the axillary artery via several deep branches at the level of the axilla, upper arm, and elbow (15).
A surviving SBA will have one of three possible outcomes. The SBA may overtake the territory of the definitive brachial artery, it may form a parallel artery to the deep brachial artery, or it can disappear as it turns into small cutaneous blood vessels (16). The first outcome corresponds with our Type I, the second to Type II, and the third to Type III (Fig. 5).
In our cases, the frequency of Type I SBAs (8.9%) is similar to the highest frequency in the literature. Fuss et al. recorded 17 cases from 200 arms (8.5%, "Type 3" in their report) (4). The corresponding frequency found by Skopakoff et al. (17) was 6.4% and by Keen (3) was 3.6% ("Type A" in his report). In Type I SBAs, all interosseous arteries arose from the ulnar artery. Some groups made comments on the type in which the SBA bifurcates into radial and ulnar arteries while the interosseous arteries are the branches of the definitive brachial artery (5). We did not found any variation of that type.
We grouped the Type I SBAs into Type Ia, Ib, and Ic because they are different in the emerging point. The precise description of differences between them is to state the relationship of the SBA with other arterial stems. In Type Ia, there were no major variations in other arteries. In Type Ib, the subscapular artery emerged higher from the axillary artery than in a normal arterial system. In Type Ic, the subscapular artery did not appear. In this type, thoracodorsal artery appears in the second part of the axillary artery and the SBA appears distally together with the circumflex scapular artery. Fuss et al. (4) divided the SBA into three subtypes, SBA superior, SBA media, and SBA inferior, along the positional relation with the median nerve. The SBA superior rises between the medial cord and lateral cord of the brachial plexus or rises medially to these cords. The SBA media rises between the medial cord and lateral cord of the brachial plexus in which the median nerve forms more distally than normal ones. The SBA inferior rises medially to the median nerve. Adachi (1) grouped the SBA into two subtypes, lateral SBA and medial SBA. The criterion to determine if an SBA is medial or lateral is whether it is medial or lateral to the medial cord of brachial plexus of the ulnar nerve. Compared to the two classifications above, ours is unique because it makes typing possible independently of the brachial plexus.
The Type II SBA continued in the forearm as the radial artery with a frequency of 6% by Keen ("Type B"), 7% by Fuss et al. ("Type 5") and 9% by Skopakoff et al. (3, 4, 17). Type II SBA, a high origin of the radial artery, is the most frequent variation in Western populations. In Korean cadavers, however, the frequency of this type of SBA is less than that of cadavers in other parts of the world (2.3%). In other words, the most frequent SBA in Korean cadavers is Type I.
The Type III SBA in our study is hard to be found in other literatures. As it tapers off in the upper arm, there were no named arterial branches. We are sure, however, that this kind of artery is indeed an SBA because it runs superficial on the deep fascia of the upper arm.
We have not encountered any SBAs that have become only the ulnar artery in the forearm. The absence of the superficial ulnar artery in the Korean population suggests that there is some difference in the hemodynamic dominance in the medial area of the upper arm between Koreans and other ethnicities. Several anatomists detected this type of arterial variation with frequency of 0.5-3.1% (2-4, 14, 17).
In summary, the dissections of the arms of Korean cadavers revealed that the SBA that bifurcates into the radial and ulnar arteries is the most frequent type of SBA in the Korean population and that there is a type of SBA that ends in the upper arm reported only in the Korean population. We could not find any SBAs that became superficial ulnar arteries.
Figures and Tables
Fig. 1
Photograph (A) and illustration (B) of type I SBA. The SBA bifurcated into the radial and the ulnar arteries after giving muscular branches to the biceps brachii and brachialis muscles.
AA, axillary artery; LC, lateral cord; MC, medial cord; M, median nerve; U, ulnar nerve; R, radial nerve; SBA, superficial brachial artery; RA, radial artery; UA, ulnar artery.

Fig. 2
Type Ia, Ib, and Ic superficial brachial arteries. Type Ia (A): the SBA emerged proximal to the stem of the subscapular artery, anterior humeral circumflex artery, and posterior humeral circumflex artery. Type Ib (B): the SBA emerged from the axillary artery distal to the stem of the subscapular artery in the second part, proximal to the stems of the circumflex arteries. Type Ic (C): the SBA emerged distal to the thoracodorsal artery from the second part of the axillary artery, proximal to the circumflex scapular artery appearing from the third part. AA, axillary artery; SBA, superficial brachial artery; SA, subscapular artery; AH, anterior humeral circumflex artery; PH, posterior humeral circumflex artery; TA, thoracodorsal artery; CA, circumflex scapular artery; LC, lateral cord; MC, medial cord; M, median nerve.

Fig. 3
Photograph (A) and illustration (B) of type II SBA. After giving muscular branches to the biceps brachii and brachialis muscles, the SBA continued as the radial artery in the forearm.
AA, axillary artery; BA, brachial artery; LC, lateral cord; MC, medial cord; M, median nerve; SBA, superficial brachial artery; RA, radial artery; UA, ulnar artery.

Fig. 4
Photograph (A) and illustration (B) of type III SBA. The slender SBA supplied the arm musculature and ended in the upper arm. AA, axillary artery; BA, brachial artery; LC, lateral cord; MC, medial cord; M, median nerve; U, ulnar nerve; SBA, superficial brachial artery; RA, radial artery; UA, ulnar artery.

Fig. 5
The development of the brachial artery and the superficial brachial artery in embryonic upper limb. (A) Absent superficial brachial artery. (B) Type I superficial brachial artery. (C) Type II superficial brachial artery. (D) Type III superficial brachial artery. During the limb development, the survival or regression of the arteries are decided by hemodynamic dominance of primitive arterial networks.
BA, brachial artery; SBA, superficial brachial artery; RA, radial artery; UA, ulnar artery.

References
1. Adachi B. Das Arteriensystem der Japaner. 1928. Vol. 1. Kyoto: Maruzen Press;196–290.
2. McCormack LJ, Cauldwell EW, Anson BJ. Brachial and antebrachial arterial patterns; a study of 750 extremities. Surg Gynecol Obstet. 1953. 96:43–54.
3. Keen JA. A study of the arterial variations in the limbs, with special reference to symmetry of vascular patterns. Am J Anat. 1961. 108:245–261.

4. Fuss FK, Matula CW, Tschabitscher M. Die Arteria brachialis superficialis. Anat Anz. 1985. 160:285–294.
5. Anagnostopoulou S, Venieratos D. An unusual branching pattern of the superficial brachial artery accompanied by an ulnar nerve with two roots. J Anat. 1999. 195:471–476.

6. Yoshinaga K, Tanii I, Kodama K. Superficial brachial artery crossing over the ulnar and median nerves from posterior to anterior: embryological significance. Anat Sci Int. 2003. 78:177–180.

7. Bataineh ZM, Al-Hussain SM, Moqattash ST. Complex neurovascular variation in one upper limb. Ital J Anat Embryol. 2007. 112:37–44.
8. D'Costa S, Shenoy BM, Narayana K. The incidence of a superficial arterial pattern in the human upper extremities. Folia Morphol (Warsz). 2004. 63:459–463.
9. Kawashima T, Yoshitomi S, Sasaki H. Anatomical relationship between the superficial brachial arteries and the brachial plexus in humans, and their morphological significance. Folia Morphol (Warsz). 2004. 63:465–471.
10. Coskun N, Sarikcioglu L, Donmez BO, Sindel M. Arterial, neural and muscular variations in the upper limb. Folia Morphol (Warsz). 2005. 64:347–352.
11. Yalcin B, Kocabiyik N, Yazar F, Kirici Y, Ozan H. Arterial variations of the upper extremities. Anat Sci Int. 2006. 81:62–64.

12. Hollinshead WH. Anatomy for surgeons. 1982. vol.3, the back and limbs:3rd ed. Philadelphia: Harper & Row;362.
13. Karamürsel S, Bağdatli D, Demir Z, Tüccar E, Celebioğlu S. Use of medial arm skin as a free flap. Plast Reconstr Surg. 2005. 115:2025–2031.
14. Rodríguez-Baeza A, Nebot J, Ferreira B, Reina F, Pérez J, Sañudo JR, Roig M. An anatomical study and ontogenetic explanation of 23 cases with variations in the main pattern of the human brachio-antebrachial arteries. J Anat. 1995. 187:473–479.
15. Singer E. Human brachial plexus united into a single cord description and interpretation. Anat Rec. 1933. 55:411–419.

16. Melling M, Wilde J, Schnallinger M, Karimian-Teherani D, Behnam M, Firbas W. Rare variant of the brachial artery: superficial lateral inferior type VII EAB. Clin Anat. 2000. 13:216–222.

17. Skopakoff C. Uber die Variabilitat der Ab-und Verzweigung der A. brachialis superficialis. Anat Anz. 1959. 106:356–368.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download