Abstract
Quantitative measurement of BK virus DNA (Q-BKDNA) has been used for the early diagnosis and monitoring of BK virus-associated nephropathy (BKVAN). This study was designed to determine the BKDNA cutoff for the diagnosis of BKVAN. Between June 2005 and February 2007, 64 renal transplant recipients taken renal biopsies due to renal impairment submitted plasma and urine for Q-BKDNA. Eight BKVAN patients (12.5%) had median viral loads of 6.0 log10 copies/mL in plasma and 7.3 log10 copies/mL in urine. Among 56 non-BKVAN patients, 45 were negative for Q-BKDNA; 4 were positive in plasma with a median viral load of 4.8 log10 copies/mL, and 10 were positive in urine with a median viral load of 4.8 log10 copies/mL. Receiver operating characteristic curve analysis showed that a cutoff of 4.5 log10 copies/mL in plasma and a cutoff of 5.9 log10 copies/mL in urine had a sensitivity of 100% and a specificity of 96.4%, respectively. A combined cutoffs of 4 log10 copies/mL in plasma and 6 log10 copies/mL in urine had better performance with a sensitivity of 100% and a specificity of 98.2% than each cutoff of urine or plasma. Q-BKDNA with the combined cutoffs could reliably diagnose BKVAN in renal transplant recipients.
BK virus-associated nephropathy (BKVAN) is an important cause of allograft loss in kidney transplant recipients (1-3). The prevalence of BKVAN has increased from 1% to 10% in the past decade (4). Although reasons for this increase have not been determined, it may be associated with the introduction of more-potent immunosuppressive agents, the increasing awareness of this disease by clinicians, and advances in diagnostic techniques (5). Because BKVAN patients show progressive allograft dysfunction without specific symptoms, it is difficult to differentiate BKVAN from acute graft rejection (6). The definitive diagnosis of BKVAN requires renal biopsy to prove viral cytopathic effects in renal tubular epithelium (7). BKVAN, however, can be coincident with acute cellular rejection, and early infiltrations frequently involve only the medulla, which is usually not included in renal biopsy (8, 9). Consequently, additional diagnostic modalities are required to diagnose BKVAN (10). Urine cytology has been used as a noninvasive screening test, but the presence of decoy cells containing viral inclusions is not a specific marker of BKVAN (11). Although quantitative polymerase chain reaction (PCR) of BK virus DNA (BKDNA) may be a more sensitive and specific test (7, 12, 13), quantitative assays of BKDNA have not been standardized, and individual laboratories need to establish and validate their own cutoffs. Several clinical laboratories in Korea have quantitatively measured BKDNA, but cutoff values for BKVAN have not been determined yet. We have therefore utilized real-time PCR to establish BKDNA cutoff values for the diagnosis of BKVAN.
All renal transplant recipients who underwent renal biopsy and quantitative measurement of BKDNA in both plasma and urine between June 2005 and February 2007 to diagnose the cause of renal impairment were retrospectively enrolled. Patients' medical records were reviewed for demographic findings and pathologic and clinical diagnoses. BKVAN was diagnosed by the presence of intranuclear viral inclusion bodies in epithelial cells and the immunohistochemical detection of SV40 antigen in renal biopsy specimens. DNA was extracted from 200 µL aliquots of urine and plasma using QIAamp MinElute Virus Spin Kits (Qiagen, Valencia, CA, U.S.A.) and eluted into 40 µL.
As the standard, the plasmid pBKV 34-2, containing the entire linearized genome of the BKV Dunlop strain inserted into the BamHI restriction site of pBR322, obtained from the American Type Culture Collection (ATCC 45025; Manassas, VA, U.S.A.), was grown in TOPO TA Cloning TOP10 cells (Invitrogen Corporation, Carlsbad, CA, U.S.A.) and purified with QIAprep Spin Miniprep kit (Qiagen). Plasmid concentration was measured by optical density using an Ultrospec 3000 spectrophotometer (Amersham Pharmacia Biotech, Piscataway, NJ, U.S.A.) and the number of viral genome equivalent copies was calculated using the equation: amount of DNA (pg)/1012×6.023×1023/(660×9,363 bp) (14). A standard curve was plotted at estimated concentrations of 0.3, 1.3, 2.3, 3.3, 5.3, and 7.3 log10 copies/µL.
Quantitative real-time PCR assays were performed using the LightCycler (Roche Diagnostics, Palo Alto, CA, U.S.A.), with BKDNA measured by the hybridization probe method. The sequences of the primers for the large T antigen gene (GenBank accession number V01108) were 5'-ACAGCAAAGCAGGCAAGG-3'and 5'-GGAGTCCTGGTGGAGTTCC-3', and the probe sequences were 5'-LC Red640-AAGCAACAGCAGATTCTCAACACTCAACA-phosphate and 5'-TTTTGCCATGAAGAAATGTTTGCCAGTGATGA-fluorescein-3', all designed by TIB MOLBIOL (Berlin, Germany). PCR amplifications were run in a reaction volume of 20 µL containing 2 µL of DNA sample, 10× LightCycler-FastStart DNA Master Hybridization Probes (Roche Molecular Biochemicals, Mannheim, Germany), 3 mM magnesium chloride, 500 nM of each primer, and 200 nM of each probe. The amplification protocol was consisted of an initial denaturation at 95℃ for 10 min, followed by 45 cycles of denaturation at 95℃ for 10 sec, annealing at 57℃ for 10 sec, and extension at 72℃ for 20 sec. Postamplification melting curve analysis was performed to distinguish BKV-specific amplicon melted at 66℃ from nonspecific melting.
Data were expressed as median values and ranges. Statistical significance was estimated by Student's two-tailed t test or Fisher's exact test, and Mann-Whitney test, with α=0.05 (SPSS package version 12.0). Receiver operating characteristic (ROC) curve analysis was used to determine the BKDNA cutoffs for diagnosis of BKVAN; ROC curves were obtained using a statistical package program from MedCalc (MedCalc, Mariakerke, Belgium).
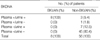
Between June 2005 and February 2007, 64 renal transplant recipients underwent renal biopsy, along with quantitative measurement of BKDNA (Q-BKDNA) in both plasma and urine, to diagnose the cause of renal impairment. The characteristics of the patients are listed in Table 1.
Eight patients (12.5%) were diagnosed with BKVAN based on pathologic findings; their median age was 40.5 yr (range, 22-60 yr) and 6 (75.0%) were male. BKVAN was diagnosed at 2.5-28 months post-transplantation (median, 5.8 months); 5 BKVAN patients (62.5%) were diagnosed within 6.5 months, but the other 3 were diagnosed after 16.5 months. Renal biopsy revealed concurrent acute cellular rejection in 6 (75.0%) of these patients. The median level of serum creatinine was 2.3 mg/dL (range, 1.9 to 3.2 mg/dL; reference 0.7-1.4 mg/dL) (Table 1).
Fifty-six (87.5%) of the 64 patients had no pathologic evidence of nephropathy. Their median age was 45.0 yr (range, 13 to 64 yr) and 37 (66.1%) were male. Renal biopsies obtained at 0.3 to 176 months post-transplantation (median, 8.5 months) showed acute cellular rejection in 32 patients (57.1%). The median level of serum creatinine was 2.4 mg/dL (range, 1.4-12.4 mg/dL) (Table 1).
There were no significant differences between BKVAN and non-BKVAN patients in age, sex, duration after kidney transplantation, acute cellular rejection, and creatinine level at renal biopsy (p>0.05 for all comparisons).
Calibration with standard DNA showed a wide linear range, from 0.6 to 7.6 log10 copy equivalents of viral DNA, with a sensitivity of as little as 2.2 copy equivalents. This corresponds to a linear range of 2.6 to 9.6 log10 copies/mL with a detection limit of 2.3 log10 copies/mL.
The overall prevalence of BKV DNAemia and DNAuria were 18.8% (12/64) and 28.1% (18/64), respectively. The median BKV loads in plasma and urine from BKVAN patients were 6.0 log10 copies/mL (range, 5.0-6.9 log10 copies/mL) and 7.3 log10 copies/mL (6.3-9.3 log10 copies/mL), respectively (Fig. 1). Forty-five (80.4%) of the 56 non-BKVAN patients were negative for BKDNA in both urine and plasma. Four (7.1%) non-BKVAN patients were positive for BKDNA in plasma, with a median viral load of 4.8 log10 copies/mL (range, 3.9-5.6 log10 copies/mL), whereas 10 (17.9%) non-BKVAN patients were positive for BKDNA in urine, with a median viral load of 4.8 log10 copies/mL (range, 3.6-7.8 log10 copies/mL) (Fig. 1). BKV DNA loads both in plasma and urine were higher in the BKVAN patients than in the non-BKVAN patients (p<0.001). All BKVAN patients were positive for BKDNA in both plasma and urine. In contrast, only 3 (5.4%) non-BKVAN patients showed both BKV DNAemia and DNAuria (Table 2).
ROC curve analysis showed that a cutoff of 4.5 log10 copies/mL BKDNA in plasma and a cutoff of 5.9 log10 copies/mL in urine had a sensitivity of 100% and a specificity of 96.4%, respectively (Fig. 2). Using each cutoff, 2 non-BKVAN patients were misclassified as having BKVAN. As a result, a total of 3 patients were falsely positive by at least one of the two criteria: one patient with a plasma viral load of 5.6 log10 copies/mL and a urine viral load of 6.5 log10 copies/mL; one patient with a plasma viral load of 5.2 log10 copies/mL, and one patient with a urine viral load of 7.8 log10 copies/mL. With the combined cutoffs of 4 log10 copies/mL in plasma and 6 log10 copies/mL in urine, two of three false positive patients were excluded, and the specificity was 98.2%.
We found that the overall prevalence of BKV DNAemia, DNAuria, and BKVAN were 18.8%, 28.1%, and 12.5%, respectively. The prevalence of BKV DNAemia, DNAuria, and BKVAN have been reported as 5-29%, 10-57%, and 1-10%, respectively (2, 4, 15-19). These wide ranges may be due to differences in post-transplantation period when samples were obtained, in immunosuppressive regimens, and in the percentages of seronegative recipients (17). We found that the prevalence of BKVAN was higher than previous studies (2, 4, 15-19). This was not surprising, since the patients in this study were confined to those with renal impairment, whereas most previous studies were based on prospective monitoring of renal transplant recipients. While most studies have found that the prevalence of BKV DNAuria was twice as high as the prevalence of DNAemia (2, 4, 15-19), we found that this ratio was only 1.5:1. Because we did not include an internal control in our assays, the possibility of residual PCR inhibitors in DNA extracts from urine specimens could not be ruled out. Urine specimens tend to have more residual inhibitors (20). To estimate the effects of these inhibitory substances on cutoff values and positivity rates, internal controls should be included in real-time PCR-based assays.
We found that 5 of the 8 BKVAN cases were diagnosed within 6.5 months after transplantation, whereas the other 3 were diagnosed from 16.5 months to 28 months. BKVAN has been reported to occur from 2 to 60 months post-transplantation (5). One early report described a bimodal distribution of BKVAN, with 50% occurring 4-8 weeks after transplantation and the remainder developing months to years later (21). More recently, the majority of BKVAN cases were found to occur within the first year after transplantation, with approximately 25% diagnosed later (3, 22). Although the number of included patients was small, our results are consistent with this bimodal distribution. Therefore, regular monitoring of BKDNA for more than 2 yr after transplantation is required for the timely diagnosis of BKVAN. It has been recommended that renal transplant recipients be monitored for BKDNA at least every 3 months during the first 2 yr post-transplantation and thereafter annually until 5 yr after transplantation (23).
We found that a cutoff of 4.5 log10 copies/mL BKDNA in plasma and a cutoff of 5.9 log10 copies/mL in urine had a sensitivity of 100% and a specificity of 96.4% in identifying patients with BKVAN. Previous studies have found that plasma BKDNA >3.7 log10 copies/mL or >4 log10 copies/mL and/or urine BKDNA of >7 log10 copies/mL can be used to diagnose BKVAN (1, 3, 22, 24). Compared to those criteria, our urine cutoff value was 1 log10 copies/mL lower, while our plasma cutoff value was similar. Because there has been no external quality control survey program for BKV quantification to date, it is difficult to determine the accuracy of this assay (7). Our finding, the lower cutoff level for urine, may be associated with partial inhibition of quantitative measurement of BKDNA in urine. We found that the use of a combined cutoffs of 4 log10 copies/mL in plasma and 6 log10 copies/mL in urine improved the specificity up to 98.2%. Since renal biopsy is highly invasive, the diagnostic specificity of Q-BKDNA is important. Thus, simultaneous measurement of BKDNA in both plasma and urine may be used to monitor renal transplant recipients for BKVAN.
In conclusion, BKVAN was significant cause of renal impairment in renal transplant recipients. Q-BKDNA could reliably diagnose BKVAN in renal transplant recipients using a combined cutoffs of 4 log10 copies/mL in plasma and 6 log10 copies/mL in urine.
Figures and Tables
Fig. 1
Distribution of BK virus DNA loads in BK virus-associated nephropathy (BKVAN) and non-BKVAN patients. Data are expressed as log10 viral copies/mL. Dashed lines indicate the suggested viral load cutoffs for diagnosis of BKVAN.

Fig. 2
Receiver operating characteristics curve for diagnosis of BKVAN and (A) plasma BKV DNA levels, and (B) urine BKV DNA levels, respectively. A cutoff of 4.5 log10 copies/mL in plasma and a cutoff of 5.9 log10 copies/mL in urine showed the best performance, respectively.

References
1. Randhawa P, Ho A, Shapiro R, Vats A, Swalsky P, Finkelstein S, Uhrmacher J, Weck K. Correlates of quantitative measurement of BK polyomavirus (BKV) DNA with clinical course of BKV infection in renal transplant patients. J Clin Microbiol. 2004. 42:1176–1180.

2. Lin PL, Vats AN, Green M. BK virus infection in renal transplant recipients. Pediatr Transplant. 2001. 5:398–405.

3. Hirsch HH, Knowles W, Dickenmann M, Passweg J, Klimkait T, Mihatsch MJ, Steiger J. Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. N Engl J Med. 2002. 347:488–496.

5. Trofe J, Gordon J, Roy-Chaudhury P, Koralnik I, Atwood W, Eash S, Alloway RR, Khalili K, Alexander JW, Woodle ES. Basic and clinical research in polyomavirus nephropathy. Exp Clin Transplant. 2004. 2:162–173.
6. Randhawa PS, Finkelstein S, Scantlebury V, Shapiro R, Vivas C, Jordan M, Picken MM, Demetris AJ. Human polyoma virus-associated interstitial nephritis in the allograft kidney. Transplantation. 1999. 67:103–109.
7. Major EO, Ryschkewitsch C, Valsamakis A, Hou J. Murray PR, Baron EJ, Jorgensen JH, Landry ML, Pfaller MA, editors. Human polyomaviruses. Manual of clinical microbiology. 2007. 9th ed. Washington DC: ASM Press;1612–1621.
8. Hirsch HH. Polyomavirus BK nephropathy: a (re-)emerging complication in renal transplantation. Am J Transplant. 2002. 2:25–30.

9. Nickeleit V, Hirsch HH, Binet IF, Gudat F, Prince O, Dalquen P, Thiel G, Mihatsch MJ. Polyomavirus infection of renal allograft recipients: from latent infection to manifest disease. J Am Soc Nephrol. 1999. 10:1080–1089.
10. Mannon RB. Polyomavirus nephropathy: what have we learned? Transplantation. 2004. 77:1313–1318.
11. Binet I, Nickeleit V, Hirsch HH, Prince O, Dalquen P, Gudat F, Mihatsch MJ, Thiel G. Polyomavirus disease under new immunosuppressive drugs: a cause of renal graft dysfunction and graft loss. Transplantation. 1999. 67:918–922.
12. Lee WH, Kim BS, Jeong HJ, Kim YS, Kim HS. BK virus detection by polymerase chain reaction in renal transplant recipients and healthy donors. Korean J Lab Med. 2003. 23:263–267.
13. Limaye AP, Jerome KR, Kuhr CS, Ferrenberg J, Huang ML, Davis CL, Corey L, Marsh CL. Quantitation of BK virus load in serum for the diagnosis of BK virus-associated nephropathy in renal transplant recipients. J Infect Dis. 2001. 183:1669–1672.

14. Leung AY, Suen CK, Lie AK, Liang RH, Yuen KY, Kwong YL. Quantification of polyoma BK viruria in hemorrhagic cystitis complicating bone marrow transplantation. Blood. 2001. 98:1971–1978.

15. Basse G, Mengelle C, Kamar N, Guitard J, Ribes D, Esposito L, Rostaing L. Prospective evaluation of BK virus DNAemia in renal transplant patients and their transplant outcome. Transplant Proc. 2007. 39:84–87.

16. Ahuja M, Cohen EP, Dayer AM, Kampalath B, Chang CC, Bresnahan BA, Hariharan S. Polyoma virus infection after renal transplantation. Use of immunostaining as a guide to diagnosis. Transplantation. 2001. 71:896–899.
17. Fogeda M, Munoz P, Luque A, Morales MD, Bouza E; BKV Study Group. Cross-sectional study of BK virus infection in pediatric kidney transplant recipients. Pediatr Transplant. 2007. 11:394–401.

18. Bressollette-Bodin C, Coste-Burel M, Hourmant M, Sebille V, Andre-Garnier E, Imbert-Marcille BM. A prospective longitudinal study of BK virus infection in 104 renal transplant recipients. Am J Transplant. 2005. 5:1926–1933.

19. Benavides CA, Pollard VB, Mauiyyedi S, Podder H, Knight R, Kahan BD. BK virus-associated nephropathy in sirolimus-treated renal transplant patients: incidence, course, and clinical outcomes. Transplantation. 2007. 84:83–88.

20. Tang YW, Sefers SE, Li H, Kohn DJ, Procop GW. Comparative evaluation of three commercial systems for nucleic acid extraction from urine specimens. J Clin Microbiol. 2005. 43:4830–4833.

21. Gardner SD, MacKenzie EF, Smith C, Porter AA. Prospective study of the human polyomaviruses BK and JC and cytomegalovirus in renal transplant recipients. J Clin Pathol. 1984. 37:578–586.

23. Hirsch HH, Brennan DC, Drachenberg CB, Ginevri F, Gordon J, Limaye AP, Mihatsch MJ, Nickeleit V, Ramos E, Randhawa P, Shapiro R, Steiger J, Suthanthiran M, Trofe J. Polyomavirus-associated nephropathy in renal transplantation: interdisciplinary analyses and recommendations. Transplantation. 2005. 79:1277–1286.

24. Ramos E, Drachenberg CB, Portocarrero M, Wali R, Klassen DK, Fink JC, Farney A, Hirsch H, Papadimitriou JC, Cangro CB, Weir MR, Bartlett ST. BK virus nephropathy diagnosis and treatment: experience at the University of Maryland Renal Transplant Program. Clin Transpl. 2002. 143–153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download