Abstract
Pregnancy outcomes in patients with congenital heart disease have not been fully assessed in Korea. Forty-nine pregnancies that occurred in 34 women with congenital heart disease who registered at our hospital between September 1995 and April 2006 were reviewed. Spontaneous abortions occurred in two pregnancies at 6+1 and 7 weeks, and another two underwent elective pregnancy termination. One maternal death in puerperium occurred in a woman with Eisenmenger syndrome. Maternal cardiac complications were noted in 18.4%, pulmonary edema in 16.3%, symptomatic arrhythmia in 6.1%, deterioration of New York Heart Association (NYHA) functional class by ≥2 in 2.0%, and cardiac death in 2.0%. Independent predictors of adverse maternal cardiac events were an NYHA functional class of ≥3 (odds ratio [OR], 20.3), right ventricular dilation (OR, 21.2), and pulmonary hypertension (OR, 21.8). Neonatal complications occurred in 22.4% of pregnancies and included preterm delivery (16.3%), small for gestational age (12.2%), and neonatal death (2.0%). Independent predictors of adverse neonatal events were pulmonary hypertension (OR, 6.8) and NYHA functional class ≥3 (OR, 23.0). Pregnancy in women with congenital heart disease was found to be significantly associated with maternal cardiac and neonatal complications. Pre-pregnancy counseling and multidisciplinary care involving cardiologists and obstetricians are recommended for women with congenital heart disease contemplating pregnancy.
Congenital heart disease occurs in about 0.7% of newborn infants worldwide, and more than 85% of these infants can expect to survive into adulthood due to recent advances in pediatric cardiology and cardiac surgery (1, 2). Consequently, the number of women with congenital heart disease who reach childbearing age is increasing, and many of them contemplate pregnancy. Although some women with congenital heart disease cannot tolerate the hemodynamic changes associated with pregnancy, many have sufficient cardiac reserve to carry pregnancy to term. Recently, a number of studies have evaluated therapeutic and management strategies for pregnancy and delivery in patients with congenital heart disease (3-6). However, a number of problems remain, and such strategies are often based on comprehensive clinical assessments without clear data due to the non-availability of standardized management strategies and limited scientific evidence. Therefore, currently, it is often impossible to provide evidence-based recommendations about the risk of pregnancy or to optimize the management of pregnant patients with congenital heart disease.
Pregnancy in women with congenital heart disease carries a considerable risk to both mothers and neonates, although prognoses continue to improve (7-10). Nevertheless, no report has been issued on the outcomes of pregnant patients with congenital heart disease in Korea, and thus, there is a need to define a risk stratification scheme for women with congenital heart disease to ensure appropriate obstetric counseling and care. The purpose of this study was to assess the outcomes and to identify the risk factors of adverse maternal and neonatal events in pregnant women with congenital heart disease in a tertiary care setting.
The records of all 890 female patients with congenital heart disease registered at the Grown-Up Congenital Heart Disease (GUCH) clinic at our hospital between September 1995 and April 2006 were reviewed. Of these 890 patients, 38 became pregnant, and 4 of these 38 patients with acquired and congenital heart disease were excluded. Finally, the outcomes of 49 pregnancies in 34 patients with congenital heart disease were analyzed.
Initial data were obtained before pregnancy or at first prenatal visit. Variables included maternal age, gestational age, parity status, New York Heart Association (NYHA) functional class, nature of the underlying cardiac lesion, cardiac medications, prior surgery/interventions, comorbid conditions (diabetes, pulmonary disease, systemic and/or pulmonary thromboembolic disease), prior cardiac events (heart failure, infective endocarditis, and arrhythmia), oxygen saturation, laboratory values (blood urea nitrogen, creatinine, and hematocrit), electrocardiography, and a comprehensive echocardiographic assessment.
Follow-up data were collected from outpatient clinics throughout pregnancy and puerperium. Fetal echocardiography was performed in all patients, and pediatric echocardiography was performed on all infants with an abnormal physical examination. Complete data on cardiac, obstetric, and neonatal events were available for all 49 pregnancies.
Cardiac, obstetric, and neonatal events were classified according to previously proposed definitions determined by Siu and colleagues (5). Maternal cardiac events were defined as cardiac death, symptomatic arrhythmia, deterioration of NYHA functional class by ≥2, or pulmonary edema documented by chest radiography. Neonatal events were defined as preterm delivery (<37 weeks of gestation), small birth weight for gestational age (<10th percentile), fetal death (≥20 weeks of gestation), or neonatal death (within the first month after birth). Spontaneous abortion was defined as fetal loss before 20 weeks of gestation. Obstetric events were defined as pregnancy-induced hypertension, postpartum hemorrhage, and noncardiac death.
Left ventricular (LV) systolic dysfunction was defined as an ejection fraction of ≤40% by Simpson's rule, has been widely used to predict pregnancy-related maternal cardiac outcomes (5, 10), and right ventricular (RV) dilation was defined as a mid right ventricular diameter at end diastole of ≥38 mm (11). Pulmonary hypertension was defined as an estimated systolic pulmonary artery pressure (sPAP) of >40 mmHg as determined by echocardiography (12). The identification of a tricuspid regurgitation jet and the quantification of its velocity (v) allow pulmonary artery pressure to be estimated using the equation sPAP=4v2+assumed right atrial pressure (RAP). RAP values were estimated as follows: lack of inferior vena cava (IVC) dilatation and plethora=10 mmHg, either IVC dilatation or plethora=15 mmHg, and IVC dilatation and plethora=20 mmHg.
SAS Version 8 (SAS Institute) software was used for the statistical analysis. Continuous data were expressed as means±standard deviations and categorical data as percentages. Maternal cardiac, neonatal, and obstetric events were analyzed separately, and because some women became pregnant twice or more, collected pregnancy data was regarded as non-independent data. Generalized estimating equations, as proposed by Zeger and Liang (13), were used to construct regression marginal models to produce cluster-sampling data. Univariate and multivariate predictors of maternal cardiac, neonatal, and obstetric events were assessed. p values of <0.05 were considered statistically significant.
A total of 34 women of mean age 29.8±3.6 yr became pregnant 49 times: 21 patients had one pregnancy, 11 had two, and 2 had three. The baseline characteristics of the study population are presented in Table 1. Of these 34 women, 6 had cyanosis defined as an initial oxygen saturation of ≤90% and an NYHA functional class of ≥3 at initial visits. These 6 cyanotic patients had either unrepaired congenital heart disease or a repaired tetralogy of Fallot (TOF) with major aortopulmonary collateral artery syndrome, and their initial oxygen saturations ranged from 70% to 86%. These patients were transferred from local clinics at near term. Cardiovascular medication was taken in 9 patients before pregnancy, and all medications were stopped at diagnosis of pregnancy, except for digoxin in two cases and aspirin in one.
Underlying congenital heart lesions are summarized in Table 2. Congenital cardiac lesions were diagnosed before pregnancy in 40 pregnancies (81.6%), in 28 patients (82.4%). In the remaining 6 patients, diagnoses were made during pregnancy or after delivery. These patients had the following cardiac malformations: atrial septal defect (n=3), patent ductus arteriosus (n=1), double outlet right ventricle with a subaortic ventricular septal defect (n=1), and Ebstein's anomaly (n=1). Surgical or interventional procedures were performed before pregnancy in 25 pregnancies (51.0%) in 17 patients (50.0%). Cardiology counseling before pregnancy was performed in 20 pregnancies (40.8%) in 14 patients (41.2%).
Clinical and echocardiographic data during pregnancies are shown in Table 3. One patient had Eisenmenger syndrome. This patient, who had a double outlet right ventricle with a subaortic ventricular septal defect, did not receive cardiology counseling before pregnancy and refused a recommendation for the therapeutic abortion.
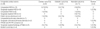
Maternal cardiac events occurred in 9 completed pregnancies (18.4%), and included heart failure with pulmonary edema, cardiac arrhythmia, a decline in NYHA class of ≥2, and cardiac death (Table 4, 5). The most common adverse cardiac event was pulmonary edema, which was documented in 8 pregnancies, and the underlying congenital cardiac anomalies were unoperated atrial septal defect (n=5), unoperated patent ductus arteriosus (n=1), repaired TOF (n=1), and unoperated double outlet right ventricle with subaortic ventricular septal defect (n=1). Symptomatic tachyarrhythmias were documented in 3 patients. Two of them with Ebstein's anomaly were cardioverted for atrial flutter/fibrillation, and one patient with repaired TOF was successfully treated medically for supraventricular tachycardia. One maternal death occurred in puerperium in a woman with Eisenmenger syndrome. There was no association between the mode of delivery and the maternal cardiac event rate: 12.5% for vaginal delivery vs. 24.0% for cesarean section (p=0.46).
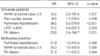
Univariate and multivariate predictors of maternal cardiac events are summarized in Table 6. An NYHA functional class of ≥3, pulmonary hypertension, and RV dilation were identified as independent predictors of an adverse maternal cardiac event.
Four pregnancies (8.2%) were aborted; 2 (4.1%) spontaneously and 2 (4.1%) electively. The two spontaneous abortions occurred during the first trimester; after 6+1 and 7 weeks of gestation. Cesarean section was performed in 25 pregnancies (51.0%), and 20 (40.8%) pregnancies resulted in successful vaginal deliveries. The 24 cesarean sections (96.0%) were performed due to obstetric indications. Pregnancy-induced hypertension complicated 3 pregnancies (6.1%), and postpartum hemorrhage complicated 3 (6.1%). All ongoing 45 pregnancies were singletons.
Obstetric and neonatal events are shown in Table 4, and stratified by congenital cardiac lesions in Table 5. Neonatal events occurred in 11 pregnancies (22.4%), and preterm delivery and small for gestational age were the most common. The mean gestation period at delivery was 38.3±2.2 weeks. Of the 45 live births, 5 neonates (11.1%) had an Apgar score of ≤5/10 at 1 min, but no adverse neonatal event occurred among these 5. The only neonatal death occurred in a patient with an unoperated ventricular septal defect. This pregnancy was complicated by infective endocarditis requiring hospitalization and antibiotics. The neonate expired 10 days after delivery due to complications arising from prematurity. Univariate and multivariate predictors of neonatal events are summarized in Table 7. Pulmonary hypertension and an NYHA functional class of ≥3 were found to be independent predictors of an adverse neonatal event.
Among the 45 live births, the rate of congenital heart disease was 8.9%. The following cardiac malformations were diagnosed: atrial septal defect (n=1), ventricular septal defect (n=1), coarctation of aorta with ventricular septal defect (n=1), and pulmonary stenosis with a hypoplastic right ventricle (n=1). All cases were detected by fetal echocardiography before birth.
The problems posed by congenital heart disease in adults are growing rapidly, in terms of both the numbers affected and disease complexity, due to the remarkable diagnostic and therapeutic advances made over the recent years (6). Thus, pregnancy outcomes and related risks in this heterogeneous patient population require comprehensive assessment to facilitate adequate patient counseling regarding safety issues and antenatal care planning. In the current study, we report the experience of a single center in terms of pregnancy outcomes in women with congenital heart disease.
The maternal cardiac event rate determined in the present study (18.4%) is comparable to that reported in a recent cohort study (19.4%) of pregnant women with congenital heart disease only (10). In a large cohort of pregnant women with heart disease, Avila et al. reported a maternal cardiac event rate of 23.5% (14). Its higher event rate may be explained by difference of study population, where only 19% of their patients had congenital heart disease.
In accordance with previous studies (5, 14), the most common maternal cardiac event in our study was pulmonary edema with congestive heart failure, which was followed by symptomatic tachyarrhythmia. All pulmonary edema and symptomatic tachyarrhythmia events responded to medical treatment. In 25 pregnancies (51.0%), patients underwent a surgical or interventional procedure before pregnancy, and a trend toward a favorable cardiac outcome was observed in this group, although there was no statistical significance (8.0% vs. 29.2%, p=0.07). Cardiology counseling before pregnancy was performed in 20 pregnancies (40.8%), and this too showed a tendency toward a lower adverse maternal cardiac event rate (5.0% vs. 27.6%, p=0.06). Postulated reasons for the lower incidence of pre-pregnancy cardiologic counseling include unplanned pregnancy and lack of education for risk of pregnancy.
In the present study, an NYHA functional class of ≥3, pulmonary hypertension, and RV dilatation were identified as independent predictors of an adverse maternal cardiac event, which concurs with previous reports on the topic (15, 16). In a recent cohort study, Khairy et al. found that women with a low subpulmonary ventricular ejection fraction and/or severe pulmonary regurgitation are 9 times more likely to develop adverse maternal cardiac events during pregnancy (10).
The adverse neonatal event rate of 22.4% observed in this study is comparable to the 27.8% found in a large cohort of pregnant women with congenital heart disease, and as was found in our study, the most common neonatal complications were premature birth followed by small for gestational age (5, 10).
Our study showed that pulmonary hypertension and an NYHA functional class of ≥3 were found to be independent predictors of an adverse neonatal event. A poor NYHA functional class has been previously reported to be a risk factor of neonatal events (5, 17). However, our study failed to substantiate the previously reported predictive role of maternal left heart obstruction on neonatal outcome (5, 17), due to the lack of patients with a left-sided obstructive lesion.
The congenital heart disease rate (8.9%) among 45 live births found in the present study, is consistent with those previously reported in women with a congenital cardiac anomaly (5, 10), and is approximately 10-fold higher than that found in the general population (18).
This study had several limitations that require consideration. First, the number of patients enrolled was relatively small, and therefore, its statistical power in terms of identifying predictors of cardiac and neonatal events is limited. Second, due to its retrospective nature, some echocardiographic data was unavailable, and treatment strategies and outcomes assessment were not standardized. Finally, because this study was performed at a tertiary care center, the study cohort might show selection bias. However, pregnant patients with congenital heart disease are usually transferred to tertiary care centers, and thus, we believe that our findings reflect the real world.
Based on our findings, maternal cardiac and neonatal complications are considerable among women with congenital heart disease. Therefore, we recommend that pre-pregnancy counseling and multidisciplinary care involving cardiologists, pediatricians, and obstetricians should be adopted when women with congenital heart disease are considering pregnancy. Furthermore, prospective, multicenter studies are needed to confirm our findings and to establish evidence-based guidelines concerning the management of pregnant patients with congenital heart disease in Korea.
Figures and Tables
Table 3
Clinical and echocardiographic data during pregnancies
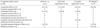
*Left ventricular systolic dysfunction was defined as an ejection fraction of ≤40% by Simpson's rule; †Right ventricular dilatation was defined as a mid right ventricular diameter ≥38 mm at end diastole.
NYHA Fc, New York Heart Association functional class; LV, left ventricle; RV, right ventricle; ASD, atrial septal defect; VSD, ventricular septal defect; PAVSD, partial atrioventricular septal defect; RV-PA, right ventricle to pulmonary artery.
References
1. Perloff JK. Congenital heart disease in adults. A new cardiovascular subspecialty. Circulation. 1991. 84:1881–1890.

2. Nieminen HP, Jokinen EV, Sairanen HI. Late results of pediatric cardiac surgery in Finland: a population-based study with 96% follow-up. Circulation. 2001. 104:570–575.

3. Connelly MS, Webb GD, Somerville J, Warnes CA, Perloff JK, Liberthson RR, Puga FJ, Collins-Nakai RL, Williams WG, Mercier LA, Huckell VF, Finley JP, McKay R. Canadian consensus conference on adult congenital heart disease 1996. Can J Cardiol. 1998. 14:395–452.
4. Iserin L. Management of pregnancy in women with congenital heart disease. Heart. 2001. 85:493–494.

5. Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC, Kells CM, Bergin ML, Kiess MC, Marcotte F, Taylor DA, Gordon EP, Spears JC, Tam JW, Amankwah KS, Smallhorn JF, Farine D, Sorensen S. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001. 104:515–521.

6. Deanfield J, Thaulow E, Warnes C, Webb G, Kolbel F, Hoffman A, Sorenson K, Kaemmer H, Thilen U, Bink-Boelkens M, Iserin L, Daliento L, Silove E, Redington A, Vouhe P, Priori S, Alonso MA, Blanc JJ, Budaj A, Cowie M, Deckers J, Fernandez Burgos E, Lekakis J, Lindahl B, Mazzotta G, Morais J, Oto A, Smiseth O, Trappe HJ, Klein W, Blomstrom-Lundqvist C, de Backer G, Hradec J, Mazzotta G, Parkhomenko A, Presbitero P, Torbicki A. Management of grown up congenital heart disease. Eur Heart J. 2003. 24:1035–1084.

7. Pitkin RM, Perloff JK, Koos BJ, Beall MH. Pregnancy and congenital heart disease. Ann Intern Med. 1990. 112:445–454.

8. Perloff JK. Pregnancy and congenital heart disease. J Am Coll Cardiol. 1991. 18:340–342.
9. Wooley CF, Sparks EH. Congenital heart disease, heritable cardiovascular disease, and pregnancy. Prog Cardiovasc Dis. 1992. 35:41–60.

10. Khairy P, Ouyang DW, Fernandes SM, Lee-Parritz A, Economy KE, Landzberg MJ. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006. 113:517–524.

11. Foale R, Nihoyannopoulos P, McKenna W, Kleinebenne A, Nadazdin A, Rowland E, Smith G. Echocardiographic measurement of the normal adult right ventricle. Br Heart J. 1986. 56:33–44.

12. Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984. 70:657–662.

13. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986. 42:121–130.

14. Avila WS, Rossi EG, Ramires JA, Grinberg M, Bortolotto MR, Zugaib M, da Luz PL. Pregnancy in patients with heart disease: experience with 1,000 cases. Clin Cardiol. 2003. 26:135–142.

15. Weiss BM, Zemp L, Seifert B, Hess OM. Outcome of pulmonary vascular disease in pregnancy: a systematic overview from 1978 through 1996. J Am Coll Cardiol. 1998. 31:1650–1657.

16. Yentis SM, Steer PJ, Plaat F. Eisenmenger's syndrome in pregnancy: maternal and fetal mortality in the 1990s. Br J Obstet Gynaecol. 1998. 105:921–922.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download