Abstract
The origin of methicillin-resistant Staphylococcus aureus (MRSA) strains from otolaryngology outpatients has not been evaluated yet in Korea. We analyzed epidemiologic and genetic characteristics of MRSA isolates from the ear discharge of 64 outpatients with chronic otitis media in a Korean University Hospital during 2004. MRSA strains were grouped as either from the initial visit (n=33) or the follow-up visit (n=31) based on the timing of isolation. Healthcare-associated risk factors were frequently present among patients of the initial visit group, especially prior visit to primary clinic (79%) and antibiotic use (73%). SCCmec typing and multilocus sequence typing results showed that two genotypes, ST5-MRSA-II and ST239-MRSA-III, were prevalent in both the initial visit (73% vs. 24%) and the follow-up visit (55% vs. 42%). Pulsed-field gel electrophoresis identified eight types, including two major types shared by both groups. We conclude that majority of MRSA strains from ear discharge of chronic otitis media belonged to nosocomial clones that might be circulating in the community. This is the first report of the genetic analysis of MRSA strains from otolaryngology practices in Korea.
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital pathogen found worldwide. According to the Korean Nationwide Surveillance of Antimicrobial Resistance study, the prevalence of MRSA has been reported as 68% of S. aureus isolates in Korean hospitals (1). Meanwhile, the rate of MRSA isolates among non-tertiary hospitals has increased to 46% in 2005 (http://karms.nih.go.kr).
The emergence of a novel type of S. aureus, community-acquired (CA) MRSA, has been reported in other parts of the world. Since it was reported first in the United States in 1995 (2), CA-MRSA has been recognized as another substantial public health threat caused by S. aureus. CA-MRSA has not been established yet in Korea, but the recent increasing prevalence of MRSA in outpatient populations has led to confusion over whether these cases originate from the community or from the healthcare setting. A substantial proportion of outpatient strains of MRSA come from ear discharge found in otolaryngology practices. However, there is no published data on the origin of MRSA strains in these patients in terms of genotypic analysis.
The genetic basis of the methicillin resistance of MRSA is the presence of the mecA gene, which encodes the low-affinity penicillin binding protein 2a. This protein is carried by a mobile genetic element staphylococcal cassette chromosome mec (SCCmec). Currently, six types of SCCmec (types I to VI) have been discovered. SCCmec types I, II, and III are associated with hospital-acquired MRSA, whereas types IV, V, and VI are associated with CA-MRSA.
In the outpatient setting, it is difficult to distinguish community-acquired MRSA from nosocomial MRSA. Based on epidemiology and past history related to healthcare-associated risk factors, MRSA could be designated as either community-acquired, healthcare-associated, or nosocomial in origin (3). However, the definite designation of MRSA strains as community-acquired or healthcare-associated requires both rigorous epidemiological and molecular analyses.
The aim of this study was to use epidemiological and genetic analyses to identify the origins of MRSA isolates from ear discharge in otolaryngology outpatients with chronic otitis media.
A total of 64 clinical isolates of MRSA were collected between January and September 2004 from ear discharge of otolaryngology outpatients with chronic otitis media in the 750-bed Korea University Anam Hospital. Only the first isolate per patient was included in the study. Oxacillin resistance was determined by the standard disk diffusion method, using the guidelines of the Clinical Laboratory Standards Institutue (CLSI) (4), and confirmed by polymerase chain reaction (PCR) amplification of the mecA gene (5).
Antimicrobial susceptibility tests were performed by disk diffusion for penicillin, clindamycin, tetracycline, oxacillin, erythromycin, cephalothin, ciprofloxacin, and vancomycin, as recommended by the CLSI (4).
The following data were collected from patients' medical charts and from hospital electronic databases: age, sex, underlying disease, dates of initial and follow-up visits, and timing of the first MRSA isolation. A survey was performed by a trained nurse on the telephone to determine whether there was direct or indirect exposure to the healthcare setting within one year, such as hospitalization, an outpatient visit, antibiotic exposure, surgical operations, or close contact with people having these risk factors.
SCCmec types were determined by rapid PCR-restriction fragment length polymorphism (RFLP) analysis of the ccrB gene, as described earlier (5). Chromosomal DNA was extracted with a Wizard genomic DNA preparation kit (Promega, Madison, WI, U.S.A.) using lysostaphin (0.5 mg/mL) and RNase (0.3 mg/mL). The 643-bp ccrB gene fragment was amplified using a pair of primers: CRB-1 (5'-GGC TAT TAT CAA GGC AAT TTA CC -3'), and CRB-2 (5'-ACT TTA TCA CTT TTG ACT ATT TCG 3'). Thermal cycling was set at 30 cycles (30 sec for denaturation at 94℃, 1 min for annealing at 50℃, and 2 min for elongation at 72℃). PCR products were purified by the QIAquick-spin PCR purification kit (Qiagen Inc., Valencia, CA, U.S.A.) and followed by digestion with HinfI and BsmI (New England Biolabs Inc., Ipswich, MA, U.S.A.). The RFLP patterns were analyzed using 2% agarose gel electrophoresis.
MLST was performed using the method described by Enright et al. (6). PCR was performed using chromosomal DNA and the identical primer sets to amplify fragments of the following seven housekeeping genes: arcC, aroE, glp, gmk, pta, tpi, and yqiL. The process was carried out with an initial denaturation at 95℃ for 5 min, followed by 30 cycles of 95℃ for 30 sec, 54℃ for 30 sec, and 72℃ for 1 min. The reaction was then maintained at 72℃ for an additional 5 min. The amplified fragments were purified using the PCR purification kit and then sequenced by Bioneer (Bioneer Co., Daejeon, Korea). The allelic profiles (STs) were determined using MLST data-base (http://saureus.mlst.net).
Chromosomal DNA from S. aureus was prepared in agarose blocks and was cleaved with SmaI (New England Biolabs Inc.). Electrophoresis was performed with the GeneNavigator System (Amersham Pharmacia Biotech, Uppsala, Sweden) using 130 V at 16℃; There were a 5 sec pulse time for 4 hr, a 25-sec pulse time for 6 hr, a 45-sec pulse time for 20 hr, and a 75-sec pulse time for 6 hr. The Lambda Ladder Standard (New England Biolabs) was used as a size marker. Band images were captured and analysis of banding patterns was performed using the Molecular Imager Gel Doc XR system (Bio Rad Laboratories, Hercules, CA, U.S.A.) and Quantity One analysis software version 4.6.1 (Bio Rad Laboratories). The similarity among all pairs was assessed using the Dice coefficient correlation; unweighted pair group method (UPGMA) clustering was used to construct a dendrogram. Band patterns of the isolates were compared using criteria for bacterial strain typing (7).
During the study period from January 2004 to September 2004, 126 isolates of MRSA were isolated from the outpatient population in this hospital. Seventy-one of these isolates (57%) were collected from the ear discharge of patients with chronic otitis media. Sixty-four patients (90%) were queried for study enrolment and the remaining 7 patients were unavailable or had an unknown timing of MRSA isolation. Based on the timing of isolation, 34 (52%) subjects had a positive culture during the initial visit and 31 patients (49%) had a positive culture during the follow-up visit. It was unknown whether the MRSA came from colonization or infection. Routinely screening cultures for MRSA from all outpatients attending the clinic was impractical due to financial and other constraints. Therefore, the screening of cultures for MRSA was performed only in patients with ear discharge on the initial visit or during the follow-up visit.
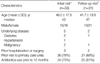
The median age of the study population was 47 yr (ranging from 1 to 79 yr), and 61% of participants (39/64) were female. Risk factors associated with MRSA acquisition were identified in both subject groups with MRSA isolates on the initial visit and the follow-up visit (Table 1). Prior visits to primary care units, including otolaryngology clinics, and antibiotic exposure in the previous 12 months were frequently present in both groups. No subjects had close contact with people having these risk factors.
All 64 S. aureus strains analyzed were confirmed as MRSA by the oxacillin disk diffusion method and the presence of a 400-bp mecA gene fragment amplified by PCR.
All 64 MRSA isolates were resistant to penicillin and erythromycin. The majority of the isolates tested were resistant to gentamicin (95.6%), tetracycline (94.1%), cephalothin (92.6%), clindamycin (91.2%), and ciprofloxacin (91.2%), while all isolates were susceptible to vancomycin. There was no difference between the initial and the follow-up isolates in resistance rates to non-β-lactam antibiotics.
Genotyping of 64 MRSA isolates showed four sequence types by MLST and three SCCmec types (II, III, and IV) by PCR-RFLP-SCCmec typing. The prevalent STs were ST5 (41 strains, 64%) and ST239 (21 strains, 33%), which carried SCCmec types II and III, respectively (Table 2). There was not a distinct demarcation of distribution of SCCmec types II and III between the initial visit and follow-up visit. The only one isolate from the follow-up visit carried SCCmec type IV.
Our data identified ST5-MRSA-II and ST239-MRSA-III as two major genotypes of MRSA isolates from ear discharge, based on the proposal by Robinson and Enright (8). The other two genotypes, ST1-MRSA-III and ST72-MRSA-IV, each were found in one isolate.
The PFGE analysis of 64 MRSA isolates showed eight genotypes (A, B, C, D, E, F, G, and H) with subtypes. There were 7 subtypes in both genotypes A and B, and 3 subtypes in genotype C. Fifty-three isolates (83%) belonged to the major genotypes, A (28 isolates) and B (25 isolates). The distribution and banding patterns of genotypes, according to the timing of MRSA isolation, are shown in Fig. 1. Genotype A was predominant in the initial visit, accounting for 56%, while genotype B was predominant in the follow-up visit, accounting for 48%. One isolate each of genotype E and F were found in the initial visit while one isolate each of genotype G and H were found in the follow-up visit. The majority of the PFGE types and subtypes in the initial visit were identified as ST5-MRSA-II and ST239-MRSA-type III, and there were similar findings in the follow-up visit as shown in Table 2.
In this study, we investigated the genetic and epidemiologic characteristics of the MRSA isolates from ear discharge of otolaryngology outpatients with chronic otitis media in order to determine whether these isolates originated from the community or the hospital. Many patients with MRSA-positive cultures during the initial visit had healthcare-associated risk factors for MRSA acquisition. Additionally, MRSA isolates from these individuals had a multi-drug resistance phenotype and were identified as major gentotypes of hospital-acquired strains (ST5-MRSA-II and ST239-MRSA-III). These characteristics of the MRSA isolates on the initial visit did not differ from those of MRSA isolates from the follow-up visit. The resistance patterns to multiple antibiotics are similar to those of MRSA strains from tertiary-care hospitals, as previously reported in a nationwide survey in Korea (9). Genotype ST5-MRSA-II has been reported as a prototype clone in Korea (10), and ST239-MRSA-III has also been prevalent in Korea since 2001 (11).
In this study, based on the timing of MRSA isolation, these risk factors were very limited in their ability to distinguish whether the MRSA was community-acquired or hospital-acquired. However, these data suggest that MRSA ear carriage on the initial visit could be acquired during the visit to primary care units. In previous studies, it had been reported that non-disposable aurioscope ear pieces were colonized with pathogenic bacteria, including MRSA, and could be a potential source of cross-colonization of MRSA among pediatric patients in an ambulatory setting (12). In addition, empirical antibiotic use and prolonged duration of antibiotic therapy were often cited for increasing bacterial resistance in primary and secondary otolaryngology care (13).
Patients with MRSA ear carriage pose unique problems in terms of treatment. Most of these individuals are asymptomatic from the bacteria but can become infected with the organisms over time. Moreover, they silently pass the organisms to other uninfected people and can transfer the organisms to other hospitals. Previous studies on MRSA isolates in the otolaryngology field showed a prevalence of MRSA only among the isolates from patients with suppurative otitis media in Japan (14) and from patients with chronic rhinosinusitis in the United States (15). Although MRSA isolation has increased among otolaryngology outpatients in recent years, there is a lack of data to explain how and where the acquisition of MRSA strains occurs.
While the data from our study were from a limited number of MRSA isolates of a Korean University Hospital, the findings support the theory that MRSA strains spread from tertiary care hospitals to primary or secondary care units in the community and then are reintroduced into tertiary care hospitals. Further studies remain to clarify the spread of nosocomial MRSA clones into primary or secondary care facilities.
In conclusion, our study indicates that the majority of MRSA isolates from otolaryngology outpatients with chronic otitis media could be healthcare-associated or hospital-acquired. This finding suggests that MRSA ear carriage is one of potential sources of intra- and inter-hospital spread in Korea. Therefore, we recommend infection control precautions and the judicious use of antibiotics in the practice of otolaryngology. This is the first report of genetic analysis of MRSA strains from otolaryngology practices in Korea.
Figures and Tables
 | Fig. 1Dendrogram and SmaI-PFGE banding patterns generated from 8 different PFGE types (A to H) with subtypes of 64 MRSA isolates. The numbers in the right indicate distribution of PFGE types based on timing of isolation (the initial visit vs. the follow-up visit). The scale in the upper left indicates the coefficient of similarity. |
Table 1
Epidemiologic characteristics of 64 outpatients with chronic otitis media according to time of MRSA isolation from ear discharge
References
1. Lee K, Kim YA, Park YJ, Lee HS, Kim MY, Kim EC, Yong D, Chong Y. Korean Nationwide Surveillance of Antimicrobial Resistance Group. Increasing prevalence of vancomycin-resistant enterococci, and cefoxitin-, imipenem- and fluoroquinolone-resistant gram-negative bacilli: a KONSAR study in 2002. Yonsei Med J. 2004. 45:598–608.
2. Moreno F, Crisp C, Jorgensen JH, Patterson JE. Methicillin-resistant Staphylococcus aureus as a community organism. Clin Infect Dis. 1995. 21:1308–1312.

3. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ. Health care--associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002. 137:791–797.

4. Clinical Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. CLSI approved standard M100-S17. 2007. Wayne, PA: Clinical and Laboratory Standards Institute.
5. Yang JA, Park DW, Sohn JW, Kim MJ. Novel PCR-restriction fragment length polymorphism analysis for rapid typing of staphylococcal cassette chromosome mec elements. J Clin Microbiol. 2006. 44:236–238.

6. Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000. 38:1008–1015.
7. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995. 33:2233–2239.

8. Enright MC, Robinson DA, Randle G, Feil EJ, Grundmann H, Spratt BG. The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA). Proc Natl Acad Sci USA. 2002. 99:7687–7692.

9. Kim HB, Jang HC, Nam HJ, Lee YS, Kim BS, Park WB, Lee KD, Choi YJ, Park SW, Oh MD, Kim EC, Choe KW. In vitro activities of 28 antimicrobial agents against Staphylococcus aureus isolates from tertiary-care hospitals in Korea: a nationwide survey. Antimicrob Agents Chemother. 2004. 48:1124–1127.

10. Ko KS, Lee JY, Suh JY, Oh WS, Peck KR, Lee NY, Song JH. Distribution of major genotypes among methicillin-resistant Staphylococcus aureus clones in Asian countries. J Clin Microbiol. 2005. 43:421–426.

11. Cha HY, Moon DC, Choi CH, Oh JY, Jeong YS, Lee YC, Seol SY, Cho DT, Chang HH, Kim SW, Lee JC. Prevalence of the ST239 clone of methicillin-resistant Staphylococcus aureus and differences in antimicrobial susceptibilities of ST239 and ST5 clones identified in a Korean hospital. J Clin Microbiol. 2005. 43:3610–3614.

12. Cohen HA, Liora H, Paret G, Lahat E, Kennet G, Barzilai A. Aurioscope earpieces--a potential vector of infection? Int J Pediatr Otorhinolaryngol. 1998. 45:47–50.
13. Raghavan U, Jones NS. Combating bacterial resistance in otorhinolaryngology. Clin Otolaryngol Allied Sci. 2002. 27:446–452.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download