Abstract
Rearrangements of the subtelomeric regions of chromosomes account for a significant proportion of the underlying genetic defects in both idiopathic mental retardation (MR) and multiple congenital anomalies. To detect the rearrangements, a set of subtelomeric fluorescence in situ hybridization (FISH) probes has been developed. The aim of this study was to reveal the frequency of subtelomeric rearrangements in Korean patients with MR or multiple anomalies. We performed a FISH study using a commercially available subtelomeric FISH probes on a series of unrelated Korean pediatric patients with MR or multiple anomalies without identifiable causes. We used a checklist to evaluate the developmental delay and/or MR. Patients who were shown to have chromosome abnormalities, metabolic disorders, or recognizable dysmorphic syndromes by clinical and laboratory findings were excluded. As a result, 100 patients were eligible for the Subtelomeric FISH study, and a total of 29 patients (29%) were suspected to have subtelomeric rearrangements on initial screening by the multiprobe FISH kit. Among theses, confirmatory FISH studies by using single locus-specific FISH probes were performed in 24 patients. One patient (a 10-yr-old girl) was confirmed to have rearrangement, deletion of the telomeric portion of the short arm of chromosome 4 (4p). Her clinical manifestation was compatible with Wolf-Hirschhorn syndrome, which is known to be caused by 4p deletion. The frequency of subtelomeric rearrangements in this study was 1.1% (1/95), lower than those previously reported (0.5-16.3%). We suggest that subtelomeric FISH test is a useful screening tool for patients with idiopathic MR and/or dysmorphism regardless of its false positive value.
It has recently been recognized that subtle rearrangements at the subtelomeric regions of chromosomes may account for a significant proportion of cases with unexplained mental retardation (MR) (1). The subtelomeric regions are gene-rich and are often involved in chromosomal rearrangements (2). Such rearrangements are typically too small to be detected by conventional cytogenetic analysis, a technique that allows detection of rearrangements with a minimum size of 3-5 Mb, if experimental circumstances are optimal and the banding patterns of the rearranged chromosomal material is distinctive. In practice, however, the resolution of conventional cytogenetic analysis may be suboptimal.
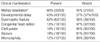
There are several laboratory techniques for the screening of subtelomeric rearrangement, e.g., fluorescent in situ hybridization (FISH) analysis using subtelomeric probes, microsatellite marker analyses (3, 4), and high-resolution comparative genome hybridization (HR-CGH) (5). Recently, the use of multiplex ligation-dependent probe amplification (MLPA) (6), multiplex amplifiable probe hybridization (MAPH) (7-9), real-time quantitative PCR (10), and microarrays (11) have also been described. A recent review showed that the frequency of subtelomeric rearrangements in subjects with MR ranged between 0.5% and 16.3%, according to the definition of study subjects (Table 1) (12). The wide range of the frequency might be attributed to one or more of the followings; the quality of chromosome preparation and banding, different study techniques used (FISH vs. microsatellite analysis vs. CGH), methods to confirm the positive findings from screening (if any), inclusion criteria, patient recruitment strategies, and the initial clinical evaluation of study subjects (13).
Here we report our experience of screening of subtelomeric rearrangements in 100 probands with MR/developmental delay and dysmorphic features by using subtelomeric FISH to assess the usefulness of the technique in identifying the underlying genetic defects in Korean patients.
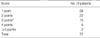
The study subjects were recruited from three institutions, Samsung Medical Center, Seoul Metropolitan Children's Hospital, and Seoul Clinical Laboratories between January 1996 and December 2003. Basically the patients were referred to the clinical laboratories for karyotyping by conventional cytogenetics. The inclusion criteria were 1) the clinical indications of MR or developmental delay for cytogenetic analyses on the test request form, together with dysmorphic features and/or malformations, or two or more malformations in case of neonates, since the mental or physical developmental potential could not be determined at that age and 2) a normal karyotypes on the GTG-banded cytogenetics at the 400- to 550-band resolution. The degree of MR (mild, IQ 50 to 70; moderate, IQ 30 to 50; severe, IQ<30) and scores from the checklist for submicroscopic subtelomeric rearrangements developed by de Vries et al. (Table 2) (14-16) were obtained from medical records.
Metaphase chromosome spreads were obtained from blood lymphocyte cultures using the standard methods. The chromosomes were GTG-banded at 400-band resolution or higher and karyotyped. The subtelomeric FISH was performed by using a commercially available set of probes (Chromoprobe Multiprobe, Cytocell, Banbury, U.K.), according to the manufacturer's instructions. The probes are targeted to the subtelomeric regions mostly at a 100-300 kb distance from the end of each of chromosome arms, excluding the short arms of acrocentric chromosomes.
Two experienced technicians each scored a minimum of five metaphases per probe in a blind manner, focusing on deletions, duplications, and balanced translocations involving the subtelomeric regions of every chromosomes. Metaphases were accepted for analysis if both the p-arm and the q-arm of two chromosome homologues could be scored. The results were considered conclusive if the first five metaphases gave 100% concordant results. If any abnormalities were suspected on screening, the results were confirmed using the single subtelomeric locus-specific probes targeted to the region of interest (Aquarius Subtelomere Specific Probe, Cytocell).
A total of 100 patients were screened for subtelomeric rearrangements (42 from Samsung Medical Center, 23 from the Seoul Metropolitan Children's Hospital, and 35 from the Seoul Clinical Laboratories). The patients' age ranged from 5 months to 27 yr, and the male-to-female ratio was 1.6:1 (62:38). Among them, 16 patients had MR/developmental delay associated with dysmorphic features; 35 patients had isolated MR; and 49 patients had isolated dysmorphic features and/or malformations.
MR could be assessed only in patients who were older than three years (n=53). Among them, 32 patients (32/53; 60%) were recorded as having MR, and the severity of MR ranged from mild (IQ<69) to severe (IQ<20). Family history of MR was documented in five patients. Developmental delay was noted in 43 patients. Dysmorphic features were observed in 62 patients with diverse manifestations with facial dysmorphism being the most frequent. Cleft palate and high-arched palate were observed in 10 and 7 patients, respectively. Seizure and epilepsy were recorded in 19 patients. Microcephaly, short stature, congenital heart defect, and seizure frequently accompanied MR (Table 3).
From the initial screening of 100 patients, subtelomeric rearrangements were suspected in 29 patients. To confirm the rearrangement, we performed single-probe FISH analysis in 24 patients; the confirmation step could not be performed in 5 patients; additional samples were not available in two patients and single FISH probes were not available in three patients.
As a result, cryptic subtelomeric anomalies were found in 1 child out of 95 patients. The submicroscopic deletion of 4pter was detected on the multiprobe FISH and subsequently confirmed by single locus-specific FISH analysis (Fig. 1). The patient was a 3-yr-old girl with mild, non-familial MR. She was born at 37 weeks, weighing 1,700 g, and had a ventricular septal defect, cleft palate, brachycephaly, malocclusion, midfacial hypoplasia, frontal bossing, epilepsy, MR, and developmental delay. Collectively, her clinical manifestation indicated Wolf-Hirschhorn syndrome, compatible with deletion 4pter. A review of the high-resolution karyotypes showed that the deletion was not discernible and thus submicroscopic. The clinical manifestations based on the checklist indicated a median score of 2 points (range, 1-8) in the patients without subtelomeric rearrangement (n=71), and 3 points in the subject with subtelomeric rearrangement (n=1) (Table 4).
Recently, a five-item clinical checklist was suggested by de Vries et al. (15) to improve the rate of detection of subtelomeric defects among mentally retarded individuals (Table 2). In the present study, this checklist was used and clinical information was gathered from the test request form for cytogenetic analyses. In this case, however, the utility of the checklist is highly dependent upon the accuracy of the clinical information given on the request form for cytogenetic analyses. Moreover, the assessment of facial morphology is rather subjective and should take into account the parental phenotypes. We also noted two of the criteria on the checklist related to the family history of MR. In five patients with a family history compatible with Mendelian inheritance, MR in at least one relative was not associated with subtelomeric rearrangement. This does not negate the value of the criterion but rather highlights its limitation when using it to select patients for testing. The checklist was developed to help select cases for subtelomeric testing and consists of five items; the presence of a family history of MR, prenatal onset of growth retardation, postnatal growth abnormalities, two or more facial dysmorphic features, and one or more non-facial dysmorphic features or congenital abnormalities. Testing of patients with a clinical score ≥3 increased the diagnostic yield by fourfold to 4.5% (1/22).
Since subtelomeric deletion was detected only in one patient out of 100 study patients (1%) screened for the cause of MR, we concluded that subtelomeric rearrangements might not be a common cause of MR in Korean pediatric patients. A recent study (17) suggested that the yield of subtelomeric screening in patients with unexplained MR depends foremost on the quality and resolution of the chromosome studies and on the nature and severity of the clinical phenotype. In the present study, the karyotyping analyses were done on high-resolution metaphases in all study subjects. Our findings are in line with those of some studies (5, 18) that showed high-resolution banding can detect most "cryptic" subtelomeric anomalies. This may explain in part the low rate of subtelomeric rearrangements observed in this study. The low frequency of subtelomeric rearrangements in the present study may also be explained by the fact that not all studies excluded the possibility of polymorphisms (19-21). We did not search for subtelomeric microdeletions in patients with a cytogenetic anomaly discernible under light microscopy, and thus possibly missed concurrent microdeletions. However, the chance of the concurrence is very low. Other explanations would include: the retrospective nature and the consecutive enrollment of patients in this study, which might have diminished biases possibly present in earlier studies. Investigations of cases with clinically recognizable microdeletion syndromes (such as 4p-) by separate FISH would have focused on suspected anomalies, and if such anomalies were found, these cases were excluded from the subtelomeric screening. Finally, differences between the present study cohort and those of other telomeric studies in terms of the proportions of cases of familial MR and in the numbers of those with dysmorphic features might have contributed. A positive family history for MR, especially when there are two or more affected members, has been suggested to indicate the presence of a subtelomeric defect (15). However, as only one patient was found to have subtelomeric defect (in a family with a negative history for MR), no correlation studies were possible.
In the previous subtelomeric screening studies, the presence of dysmorphic features has been used as an important selection criterion (18, 20-22). However, the term "dysmorphic features" was not further defined in most cases, and the dysmorphic findings were not subcategorized, which are mandatory when analyzing the phenotypes. The determination of dysmorphism is subjective, and the traits are hard to be quantified. The lack of clear definitions for some of the symptoms, the absence of reference standards for normality, and the absence of reliable incidence figures that take into account the age and ethnic origin of patients, all contribute to make the definition of dysmorphism unclear. Therefore, the phenotypic anomalies observed in the present study were not less frequent than those in other screened groups, and cannot explain the lower rate of subtelomeric deletions. Finally, another possibility would be that the low rate of positive cases has occurred by chance.
Another point to note is that the false positive rate of the screening using multiprobe FISH was considerably high (only one out of 24 patients was confirmed to have subtelomeric deletion) according to our experience. The main reason for this finding might be the different reactivities of 24 square areas, which carry subtelomeric probes for one of the 23 chromosomes, resulting in the different hybridization rate of subtelomere probe. Thus, we suggest that one should not make a conclusion on the presence of rearrangement based solely on the multiprobe FISH but should confirm the rearrangement using a single probe FISH specifically targeted to the subtelomeric region of interest as indicated by multiprobe FISH.
In many patients referred for subtelomeric screening even after a long period of laboratory investigations and follow-up, the identification of subtelomeric rearrangements can be very helpful, especially in parents at childbearing age because prenatal testing and more accurate counseling regarding recurrence risks can be offered. Recently, a new methodology called MLPA has been developed. This method has proven to be accurate and reliable for identifying deletions, duplications, and amplifications in several diseases (23-26) as well as for the screening of subtelomeric rearrangements (6, 12).
We have shown that subtelomeric FISH is helpful in patients with dysmorphic features and MR of unknown etiology with a normal karyotype as a second-line modality in the laboratory investigation. However, subtelomeric FISH has also disadvantages in that it is expensiveness and time-consuming. The pathogenic role of subtelomeric rearrangements is not certain, so prospective studies by other, more efficient techniques, such as MLPA, are needed.
Figures and Tables
Fig. 1
(A) Metaphases fluorescence in situ hybridization (FISH) using subtelomeric multiprobes showed one normal chromosome 4 with red signals from the subtelomeric region of the long arm and green signals from the subtelomeric region of the short arm (arrow) and the other copy of chromosome 4 lacking the green signals (headarrow), indicating the deletion of the subtelomeric region of the short arm of chromosome 4. (B) We confirmed the finding from the multiprobes using a single probe for 4p. Only one chromosome 4 revealed signals from 4p (arrow), indicating deletion of 4p telomere in the other copy of chromosome 4 (headarrow). (C) Partial G-banded karyotype of chromosome 4 of this patient. Chromosomal abnormality was not detected via conventional cytogenetic analysis.

References
2. Shaffer LG, Lupski JR. Molecular mechanisms for constitutional chromosomal rearrangements in humans. Annu Rev Genet. 2000. 34:297–329.

3. Colleaux L, Rio M, Heuertz S, Moindrault S, Turleau C, Ozilou C, Gosset P, Raoult O, Lyonnet S, Cormier-Daire V, Amiel J, Le Merrer M, Picq M, de Blois MC, Prieur M, Romana S, Cornelis F, Vekemans M, Munnich A. A novel automated strategy for screening cryptic telomeric rearrangements in children with idiopathic mental retardation. Eur J Hum Genet. 2001. 9:319–327.

4. Rio M, Molinari F, Heuertz S, Ozilou C, Gosset P, Raoul O, Cormier-Daire V, Amiel J, Lyonnet S, Le Merrer M, Turleau C, de Blois MC, Prieur M, Romana S, Vekemans M, Munnich A, Colleaux L. Automated fluorescent genotyping detects 10% of cryptic subtelomeric rearrangements in idiopathic syndromic mental retardation. J Med Genet. 2002. 39:266–270.
5. van Karnebeek CD, Koevoets C, Sluijter S, Bijlsma EK, Smeets DF, Redeker EJ, Hennekam RC, Hoovers JM. Prospective screening for subtelomeric rearrangements in children with mental retardation of unknown aetiology: the Amsterdam experience. J Med Genet. 2002. 39:546–553.

6. Koolen DA, Nillesen WM, Versteeg MH, Merkx GF, Knoers NV, Kets M, Vermeer S, van Ravenswaaij CM, de Kovel CG, Brunner HG, Smeets D, de Vries BB, Sistermans EA. Screening for subtelomeric rearrangements in 210 patients with unexplained mental retardation using multiplex ligation dependent probe amplification (MLPA). J Med Genet. 2004. 41:892–899.

7. Armour JA, Sismani C, Patsalis PC, Cross G. Measurement of locus copy number by hybridisation with amplifiable probes. Nucleic Acids Res. 2000. 28:605–609.

8. Sismani C, Armour JA, Flint J, Girgalli C, Regan R, Patsalis PC. Screening for subtelomeric chromosome abnormalities in children with idiopathic mental retardation using multiprobe telomeric FISH and the new MAPH telomeric assay. Eur J Hum Genet. 2001. 9:527–532.

9. White SJ, Breuning MH, den Dunnen JT. Detecting copy number changes in genomic DNA: MAPH and MLPA. Methods Cell Biol. 2004. 75:751–768.

10. Boehm D, Herold S, Kuechler A, Liehr T, Laccone F. Rapid detection of subtelomeric deletion/duplication by novel real-time quantitative PCR using SYBR-green dye. Hum Mutat. 2004. 23:368–378.

11. Le Caignec C, Boceno M, Saugier-Veber P, Jacquemont S, Joubert M, David A, Frebourg T, Rival JM. Detection of genomic imbalances by array based comparative genomic hybridisation in fetuses with multiple malformations. J Med Genet. 2005. 42:121–128.

12. Rooms L, Reyniers E, Kooy RF. Subtelomeric rearrangements in the mentally retarded: a comparison of detection methods. Hum Mutat. 2005. 25:513–524.

13. Riegel M, Baumer A, Jamar M, Delbecque K, Herens C, Verloes A, Schinzel A. Submicroscopic terminal deletions and duplications in retarded patients with unclassified malformation syndromes. Hum Genet. 2001. 109:286–294.

14. Baralle D. Chromosomal aberrations, subtelomeric defects, and mental retardation. Lancet. 2001. 358:7–8.

15. de Vries BB, White SM, Knight SJ, Regan R, Homfray T, Young ID, Super M, McKeown C, Splitt M, Quarrell OW, Trainer AH, Niermeijer MF, Malcolm S, Flint J, Hurst JA, Winter RM. Clinical studies on submicroscopic subtelomeric rearrangements: a checklist. J Med Genet. 2001. 38:145–150.

16. Walter S, Sandig K, Hinkel GK, Mitulla B, Ounap K, Sims G, Sitska M, Utermann B, Viertel P, Kalscheuer V, Bartsch O. Subtelomere FISH in 50 children with mental retardation and minor anomalies, identified by a checklist, detects 10 rearrangements including a de novo balanced translocation of chromosomes 17p13.3 and 20q13.33. Am J Med Genet A. 2004. 128:364–373.

18. Joyce CA, Dennis NR, Cooper S, Browne CE. Subtelomeric rearrangements: results from a study of selected and unselected probands with idiopathic mental retardation and control individuals by using high-resolution G-banding and FISH. Hum Genet. 2001. 109:440–451.

19. Kirchhoff M, Rose H, Lundsteen C. High resolution comparative genomic hybridisation in clinical cytogenetics. J Med Genet. 2001. 38:740–744.

20. Anderlid BM, Schoumans J, Anneren G, Sahlen S, Kyllerman M, Vujic M, Hagberg B, Blennow E, Nordenskjold M. Subtelomeric rearrangements detected in patients with idiopathic mental retardation. Am J Med Genet. 2002. 107:275–284.

21. Baker E, Hinton L, Callen DF, Altree M, Dobbie A, Eyre HJ, Sutherland GR, Thompson E, Thompson P, Woollatt E, Haan E. Study of 250 children with idiopathic mental retardation reveals nine cryptic and diverse subtelomeric chromosome anomalies. Am J Med Genet. 2002. 107:285–293.

22. Clarkson B, Pavenski K, Dupuis L, Kennedy S, Meyn S, Nezarati MM, Nie G, Weksberg R, Withers S, Quercia N, Teebi AS, Teshima I. Detecting rearrangements in children using subtelomeric FISH and SKY. Am J Med Genet. 2002. 107:267–274.

23. Hogervorst FB, Nederlof PM, Gille JJ, McElgunn CJ, Grippeling M, Pruntel R, Regnerus R, van Welsem T, van Spaendonk R, Menko FH, Kluijt I, Dommering C, Verhoef S, Schouten JP, van't Veer LJ, Pals G. Large genomic deletions and duplications in the BRCA1 gene identified by a novel quantitative method. Cancer Res. 2003. 63:1449–1453.
24. Janssen B, Hartmann C, Scholz V, Jauch A, Zschocke J. MLPA analysis for the detection of deletions, duplications and complex rearrangements in the dystrophin gene: potential and pitfalls. Neurogenetics. 2005. 6:29–35.

25. Schwartz M, Duno M. Multiplex ligation-dependent probe amplification is superior for detecting deletions/duplications in Duchenne muscular dystrophy. Clin Genet. 2005. 67:189–191.

26. Shao H, Lip V, Wu BL. Effectiveness of multiplex ligation-dependent probe amplification assay used for detecting deletion of Prader-Willi syndrome. Beijing Da Xue Xue Bao. 2005. 37:64–67.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download