INTRODUCTION
Embryologically the thyroid gland is derived from 2 anlages: a large median endodermal anlage and two lateral anlages. The median anlage produces most of the thyroid parenchyma, while the lateral anlage is derived from the fourth pharyngeal pouch and contributes 1% to 30% of the thyroid weight (1). Commonly, failure in the descent of the median anlage results in a lingual thyroid gland. In rare cases, failure of the lateral anlage to fuse with the median anlage can result in lateral ectopic thyroid gland (2).
We present a case report of a 54-yr-old woman with presumed metastatic papillary thyroid carcinoma (PTC) of lateral neck nodes, as was expected from clinical and computed tomography (CT) findings. Total thyroidectomy with left modified radical neck dissection (MRND) was performed, but histological examination of the mass at the lateral neck showed ectopic thyroid tissue with a hyperplastic pattern. There was also no malignancy in other lymph nodes.
CASE REPORT
A 54-yr-old female presented with palpable masses in the left lateral neck region. Physical examination revealed two firm, non-tender, mobile masses of 3×3 cm size and 4×4 cm, respectively. The thyroid gland was not palpable in its normal position. A CT scan of the head and neck with contrast was done, which showed a mass (2×2 cm) with calcification on the left lobe of the thyroid, and also revealed that the two palpable masses at the left lateral neck were enhanced with calcification on the left level II (3.5×4.5 cm) and III (3.5×4 cm) (Fig. 1). Fine-needle aspiration biopsy (FNAB) of the mass at left lateral level II resulted in fibroadipose tissues, but suggested lateral neck metastasis of PTC, as evidenced by calcification and cystic change on CT scan, and a FNAB of the calcified nodule at the left lobe of thyroid consisted of intranuclear inclusion, which was indicative of PTC.
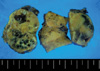
The patient underwent total thyroidectomy with left MRND under the presumptive diagnosis of lateral neck metastasis of PTC. The two masses at level II and III had calcification and cystic change, which is sufficient evidence of neck metastasis. However, unlike nodal metastasis of PTC, which is gray, these masses were homogeneous and pink (Fig. 2). The pathologic diagnosis of the nodule at the left lobe of the thyroid was PTC without capsular invasion, and the mass in the left lateral neck was an ectopic thyroid gland with a hyperplastic pattern (Fig. 3). On pathologic examination, four nodes of the central compartment and five nodes of left level IV and V were not malignant.
DISCUSSION
Ectopic thyroid gland is defined as thyroid tissue not located anterolaterally in the second to fourth tracheal cartilages. The lingual location is most common, accounting for 90% of reported cases (2-4). Bradley et al. (5) reported multifocal papillary thyroid carcinoma occurring very rarely in a lingual thyroid. An ectopic thyroid gland in the region of the submandibular gland and intra-trachea is also very rare (6, 7). Other rare sites of an ectopic thyroid gland include the mediastinum, esophagus, lung, heart, aorta, and abdomen. Evert-Jan et al. (8) reported an accessory thyroid gland at the carotid bifurcation.
Differential diagnosis between lingual thyroid tissue and metastatic thyroid cancer may be difficult. On inspection, the surface of the lingual thyroid may be smooth or irregular. Occasionally, large blood vessels are present on the surface of lingual thyroid tissue, predisposing it to ulceration and hemorrhage (9). Most detailed histological studies have shown that lingual thyroid tissue characteristically has an incomplete or poorly defined capsule. Therefore, benign lingual thyroid tissue may appear malignant due to what appears to be an invasion into the muscle, but this only signifies a defect in the capsule, resulting in intermingling of the glandular and the muscular elements.
Basaria et al. (3) reported ectopic lingual thyroid masquerading as thyroid cancer metastases. They performed a total thyroidectomy and radioiodine therapy due to PTC. One year after the operation, a diagnostic radioiodine scan showed a significant residual uptake at the level of the chin, thought to be consistent with a metastasis at the base of the tongue. The patient received radioactive iodine therapy, but did not improve. Incisional biopsy was done, and histological examination showed numerous follicular structures, and a diagnosis of ectopic thyroid was made. Interestingly, a kinetic analysis of iodine turnover in lingual thyroid tissue showed a biological half-life of 1.3 days compared with 100 days in normal thyroid tissue (10). This phenomenon may explain why the lingual thyroid in the present patient was so resistant to ablation, compared with the remnant tissue in the thyroid bed.
In our case report, we described a patient with PTC who had two ectopic lateral thyroid glands in the neck masquerading as a metastatic focus. In fact, ectopic thyroid glands of the midline, like lingual thyroid, are not easily mistaken for metastatic PTC, because it is almost impossible for metastasis of PTC at level I of the neck to skip over levels II, III, and IV. However, if PTC is combined with lateral neck masses with calcification, why did someone suggest it was an ectopic thyroid at the lateral neck? If preoperatively diagnosed as an ectopic thyroid, selective neck dissection may be enough. However, since it is impossible for suspected calcified masses of the lateral neck to be an ectopic thyroid, MRND must be performed in such cases.
Currently, there are a relatively large number of reports on ectopic thyroid, but there are few articles that present ectopic thyroid coexisting simultaneously with PTC. If a preoperative diagnostic method could be developed that can differentiate between ectopic thyroid tissue and metastatic thyroid cancer, an accurate assessment of the extent of operation would be made.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download