Abstract
Brunner's gland hyperplasia is a benign tumor of the duodenum and it is rarely associated with clinical symptoms. We report on a 64-yr-old man with Brunner's gland hyperplasia who had undergone a duodenocephalo-pancreatectomy. The reason is that he presented upper gastrointestinal obstructive symptoms and the esophagogastroduodenoscopic finding revealed the lesion to be an infiltrating type mass on the second portion of the duodenum with luminal narrowing. An abdominal computed tomography showed a 2.5 cm-sized mass in the duodenal second portion with a suspicious pancreatic invasion and 7 mm-sized lymph node around the duodenum. Duodenocephalopancreatectomy was successfully performed. Histological examination revealed a Brunner's gland hyperplasia. The final diagnosis was the coexistence of Brunner's gland hyperplasia and pancreatic heterotopia with a pancreatic head invasion. The literature on Brunner's gland hyperplasia is reviewed.
Brunner's gland, which was accurately described by Brunner in 1688, is a gland in the submucosa of the duodenum (1), which has a main physiological function of secreting an alkaline-based mucus to protect the duodenal lining from the acid secreted in the stomach. Brunner's gland hyperplasia makes up 10.6% of benign tumors in the duodenum and rarely presents any symptoms (2). The first case of Brunner's gland hyperplasia was reported in 1835 in a patient with fatal duodenal intussusceptions (3). It is usually found incidentally because it is small and asymptomatic. However, Brunner's gland hyperplasia can lead to significant symptoms including gastrointestinal bleeding, abdominal pain, and intestinal obstruction. The Brunner's gland hyperplasia is generally polypoid in configuration. We report on an unusual case of a diffuse nodular type of Brunner's gland hyperplasia with symptoms of intermittent upper abdominal pain, nausea, and vomiting, which was difficult to differentiate from malignancy.
A 64-yr-old man visited a private clinic with episodes of epigastric discomfort, dyspepsia, nausea, and vomiting for several days. A duodenal mass was found on esophagogastroduodenoscopy. He was then referred to our hospital. On admission, he had no significant past medical history, but had a weight loss of 7 kg. Laboratory values were as follows: white blood cells 10,950/µL, hemoglobin 12.9 g/dL, platelets 295 K/µL, aspartate aminotransferases (AST) 25 IU/mL, alanine aminotransferases (ALT) 10 IU/mL, alkaline phosphatase (ALP) 72 IU/L, gamma glutamyl transpeptidase (gamma-GT) 102 IU/L, and total bilirubin 0.7 mg/dL. Other laboratory values were within normal limits. An esophagogastroduodenoscopy showed an infiltrating type mass on the second portion of the duodenum with luminal narrowing. So, the scope could not pass through the narrowed lumen (Fig. 1). A 3-D abdominal computer tomography (CT) was then performed, which showed a 2.5 cm-sized mass in the second portion of duodenum and a loss of fat plane between the duodenal mass and pancreas, which gave suspicion of a pancreatic invasion and a 7 mm-sized lymph node around the duodenum. The stage based on the CT finding was stage III (T3, N1, Mx) (Fig. 2). The tissue from the endoscopic biopsy showed moderate and chronically active duodenitis. Since the patient had symptoms of recurrent vomiting and weight loss due to duodenal obstruction and the finding from the abdominal CT was suspicious of duodenal cancer in the second portion with a pancreatic invasion, we decided to perform an operation on the patient. The frozen biopsy from the operation showed a pancreatic heterotopia without evidence of malignancy. However, we performed a duodenocephalopancreatectomy, because we could not completely exclude malignancy due to the CT finding and suspected that the lesion leading to duodenal obstruction in the second portion of duodenum included the ampulla.
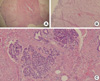
The histological examination of the second portion of the duodenum showed a diffuse nodular type of Brunner's glands hyperplasia with inflammation of the ampulla, and there was reactive lymphadenopathy of regional lymph nodes. Pancreatic heterotopia was found in the subserosa of the duodenum (Fig. 3). Finally, the patient was diagnosed with a diffuse nodular type of Brunner's gland hyperplasia with duodenal obstruction. The patient was discharged 25 days after the operation without any complications.
Patients who have Brunner's gland hyperplasia of the duodenum are frequently affected with chronic pancreatitis (4), duodenal ulcers, and chronic erosive gastritis. The cause of Brunner's gland hyperplasia is thought to be chronic inflammation, chronic stimulus by excessive secretion of gastric acids, or the decrease of the pancreatic exocrine function. However, it is recently thought that the hyperactivity of the exocrine modulating factor (hormone, vagus nerve, and intestinal mucous membrane factor) is the major cause of Brunner's gland hyperplasia (5).
The clinical manifestations of Brunner's gland hyperplasia are nonspecific, such as epigastric discomfort, abdominal distension, or dyspepsia etc. Occasionally, it can lead to hemorrhages, acceleration of peristalsis, diarrhea, transient and partial bowel obstruction and duodenal intussusception due to the mass (3).
Brunner's gland hyperplasia, a submucosal tumor, can be diagnosed by endoscopy, biopsy, abdominal CT, and other radiologic techniques. Only about 0.3-4.6% of the benign tumor originating from the duodenum can be found by the endoscope (6). Brunner's gland hyperplasia is vary rare and represents 10.6% among this amount (7).
Brunner's gland hyperplasia is distributed mainly on the duodenal bulb (57%), the duodenum's second portion (27%), and its third portion (7%). It is rarely on the pylorus (5%), jejunum (2%), or the terminal ileum (2%) (8).
In 1934, Feyrter classified the abnormal glandular proliferation into the following three types: diffuse nodular hyperplasia (type 1), occupying most of the duodenum; circumscript nodular hyperplasia (type 2), the most common type mainly present in the duodenal bulb; and, adenomatous hyperplasia (type 3), which may be sessile or pedunculated (4, 9-12).
This first-mentioned type corresponds with the Brunner's gland hyperplasia found in our patient. This diffuse nodular hyperplasia (type 1) is often mistaken for a malignancy.
The diagnosis of Brunner's gland hyperplasia is supported by endoscopy and radiologic findings. However, sensitivity of the endoscopy is 72-89% and occasionally, the endoscopy is not useful in making the diagnosis (3, 7, 13, 14). Thus, we found that abdominal CT was useful in this case.
There is no consensus on the therapeutic principle for Brunner's gland hyperplasia because follow-up study is insufficient. The medical treatment is to control gastric hyperacidity, which is one cause of Brunner's gland hyperplasia. However, the regression of Brunner's gland hyperplasia is rare (7). Therefore, excision appears to be the treatment of choice. We should completely remove the lesion by endoscopic resection or surgical resection when Brunner's gland hyperplasia leads to symptoms and complications or when definite diagnosis is necessary (7, 15-17).
According to a recent report, other research opinions state that non-symptomatic Brunner's gland hyperplasia should be resected by all means because it undergoes malignant transformations in some cases (7, 18).
There are various methods for the resection of Brunner's gland hyperplasia. For instance, endoscopic polypectomy should be performed if the lesions are less than 1 cm in diameter, if the size is excessively large or if the tumor is the sessile type. Then, surgical polypectomy, duodenal wedge resection, or partial gastrectomy that is extended to the duodenal bulb should be done (7). However, there is one report of a duodenocephalopancreatectomy, in a Brunner's gland hyperplasia case involving the duodenal second portion with a pancreatic invasion (7). Domenico Lusco et al. reported the case of a voluminous Brunner's gland hyperplasia induced stenosis of the duodenal second portion and a pancreatic duct dilatation on an abdominal CT finding. Even though the frozen biopsy showed no evidence of malignancy, they decided to carry on with the operation because they could not exclude the possibility of malignancy (7).
Our case is similar to the case by Domenico Lusco et al. The abdominal CT scans of this case showed the findings of duodenal cancer with a pancreatic head invasion and a regional lymph node enlargement. Also, the patient had symptoms of nausea, vomiting, and epigastric pain due to obstruction. This case helped us to decide on the operation. The histological findings of frozen biopsy from the operation had no evidence of malignancy, but showed pancreatic heterotopia. However, sensitivity of frozen biopsy is 83-92% (19-22) and its diagnostic accuracy is 91-97% (19, 23, 24). So, we could not exclude malignancy even after a frozen biopsy. The excision area should be minimal in Brunner's gland hyperplasia because it is a benign tumor. However, if the tumor involves the second portion of duodenum and invades the pancreatic area just as in this case, then duodenocephalopancreatectomy should be considered.
Another unique aspect of this case is the coexistence of Brunner's gland hyperplasia and pancreatic heterotophia. The relation of ectopic pancreas and Brunner's gland hyperplasia is not clear. Although there is less connection between the cause of Brunner's gland hyperplasia and the pancreatic heterotophia, we need further studies about the relationship of Brunner's gland hyperplasia with pancreatic heterotophia.
In our case, a duodenocephalopancreatectomy was performed due to symptoms of Brunner's gland hyperplasia with a pancreatic invasion, which induced epigastric discomfort, nausea, and vomiting.
Figures and Tables
Fig. 1
Endoscopic finding: the duodenal mass was an irregular and infiltrative type mass on the duodenal bulb area.

References
1. Tan YM, Wong WK. Giant Brunneroma as an unusual cause of upper gastrointestinal hemorrhage: report of a case. Surg Today. 2002. 32:910–912.

2. Peetz ME, Moseley HS. Brunner's gland hyperplasia. Am Surg. 1989. 55:474–477.
3. de Silva S, Chandrasoma P. Giant duodenal hamartoma consisting mainly of Brunner's glands. Am J Surg. 1977. 133:240–243.

4. Bastlein C, Decking R, Voeth C, Ottenjann R. Giant Brunneroma of the duodenum. Endoscopy. 1988. 20:154–155.

5. Franzin G, Musola R, Ghidini O, Manfrini C, Fratton A. Nodular hyperplasia of Brunner's glands. Gastrointest Endosc. 1985. 31:374–378.

6. Perez A, Saltzman JR, Carr-Locke DL, Brooks DC, Osteen RT, Zinner MJ, Ashley SW, Whang EE. Benign nonampullary duodenal neoplasms. J Gastrointest Surg. 2003. 7:536–541.
7. Iusco D, Roncoroni L, Violi V, Donadei E, Sarli L. Brunner's gland hamartoma: 'over-treatment' of a voluminous mass simulating a malignancy of the pancreatic-duodenal area. JOP. 2005. 6:348–353.
8. Walden DT, Marcon NE. Endoscopic injection and polypectomy for bleeding Brunner's gland hamartoma: case report and expanded literature review. Gastrointest Endosc. 1998. 47:403–407.

9. Nakanishi T, Takeuchi T, Hara K, Sugimoto A. A great Brunner's gland adenoma of the duodenal bulb. Dig Dis Sci. 1984. 29:81–85.

11. Buchanan EB. Nodular hyperplasia of Brunner's glands of the duodenum. Am J Surg. 1961. 101:253–257.

13. Gourtsoyiannis NC, Bays D, Papaioannou N, Theotokas J, Barouxis G, Karabelas T. Benign tumors of the small intestine: preoperative evaluation with a barium infusion technique. Eur J Radiol. 1993. 16:115–125.

14. Cwikiel W, Andren-Sandberg A. Diagnostic difficulties with duodenal malignancies revisited: a new strategy. Gastrointest Radiol. 1991. 16:301–304.

15. Adell-Carceller R, Salvador-Sanchis JL, Navarro-Navarro J, Segarra-Soria M, Garcia-Calvo R, Gibert-Gerez J, Colom-Costa J. Laparoscopically treated duodenal hamartoma of Brunner's glands. Surg Laparosc Endosc. 1997. 7:298–300.
16. Bae SW, Lee DK, Baik SG, Kwon SO, Cho MY. A Brunner's Gland Adenoma Removed by Endoscopic Polypectomy. Korean J Gastrointest Endosc. 1993. 13:83–86.
17. De Castella H. Brunner's gland adenoma. An unusual cause of intestinal bleeding. Br J Surg. 1966. 53:153–156.
18. Akino K, Kondo Y, Ueno A, Yamazaki K, Hosokawa M, Shimoji H, Adachi T, Honda S, Ichiyanagi S, Akahonai Y, Fujisawa Y, Takahashi H, Arimura Y, Endo T, Imai K. Carcinoma of duodenum arising from Brunner's gland. J Gastroenterol. 2002. 37:293–296.

19. Skellenger ME, Kinner BM, Jordan PH Jr. Brunner's gland hamartomas can mimic carcinoma of the head of the pancreas. Surg Gynecol Obstet. 1983. 156:774–776.
20. Lightwood R, Reber HA, Way LW. The risk and accuracy of pancreatic biopsy. Am J Surg. 1976. 132:189–194.

21. Ingram DM, Sheiner HJ, Shilkin KB. Operative biopsy of the pancreas using the Trucut needle. Aust N Z J Surg. 1978. 48:203–206.

23. Spjut HJ, Ramos AJ. An evaluation of biopsy-frozen section of the ampullary region and pancreas: a report of 68 consecutive patients. Ann Surg. 1957. 146:923–930.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download