Abstract
It is well known that the amplification of the HER2 gene is closely associated with poor prognosis of breast cancer. However, there is controversy about the clinical significance of HER2 according to lymph node status in breast cancer. The aim of this study was to identify the differences in the prognostic significance of HER2 gene amplification according to the stages of breast cancer. We prepared a tissue array for fluorescence in situ hybridization (FISH) with breast cancer specimens from the surgery in 1994 to 1999. Total 338 cases of breast cancer were enrolled and the median follow-up period was 6.3 yr. The detection rates of HER2 gene amplification were as follows: 10.3% in stage I, 22.3% in stage II, and 43.8% in stage III. On survival analyses HER2-positive groups showed worse prognosis in stage III of breast cancer, but not in stage I or II. Multivariate analyses with a Cox-regression model also revealed that HER2 amplification was an independent prognostic factor only in stage III breast cancer. Regarding HER2 gene amplification as a prognostic factor of breast cancer, the clinical significance of the gene was found to be confined to advanced breast cancer.
The prognosis of breast cancer is usually determined by the disease stage (TNM stage) after surgery that assesses the size of tumor (T), the status of metastasis to adjacent lymph nodes (N), and the presence or absence of distant metastasis to other organs (M). The prognosis of patients classified according to TNM stage is different even in the same stage. In other words, in the same stage of breast cancer, the prognosis depends on the expression of estrogen or progesterone receptor (ER or PR) and the over-expression of HER2 protein or the amplification of the gene. Therefore, some investigators have proposed a new staging system for breast cancer including such prognostic factors mentioned above (1).
So far, the over-expression of HER2 protein or the amplification of the gene has been recognized as a prognostic factor of breast cancer and to be associated with poor prognosis (2-7). However, it has been also claimed that the prognostic significance of HER2 is found not in all breast cancer, but only in advanced cases with lymph node metastasis (8). Thus, it is still a controversial issue. Recently, the therapeutic effect of the targeted therapy using trastuzumab for breast cancer has been approved in adjuvant setting (9, 10). So, the clinical significance of HER2 is increased in the determination of indication for targeted therapy as well as of prognosis of breast cancer.
Test methods to assess HER2 status are diverse from gene level to protein level. Immunohistochemistry (IHC) for the detection of HER2 proteins is relatively easy, simple, cheap, and thus performed widely, but has a great shortcoming of the variable interpretation of the same results, i.e., lack of objectivity of results. Therefore, for a vague result obtained by immunohistochemical staining method, it is recommended to assess the accurate status of HER2 gene amplification by performing fluorescence in-situ hybridization (FISH) because its accuracy and reliability are high, even though expensive (11-13). Therefore, the results by FISH are more significant than that of IHC in determination of effects of HER2 on the prognosis of breast cancer.
In this study, we performed FISH for the detection of HER2 gene amplification and investigated the prognostic significance of HER2 according to the stages of breast cancer.
Among the cases of patients underwent mastectomy for breast cancer with invasive ductal carcinoma (NOS) at our institution from January 1994 to December 1999, 338 cases were enrolled in this study who were available for the retrospective examination of medical records and the follow-ups as well as feasible for the amplification of HER2 gene test with good condition of the stored paraffin-embedded tissues. The subjects had never been treated with trastuzumab before this study and had a sufficient follow-up period.
The area representing the histological finding of breast cancer in the paraffin-embedded tissues of each case was assessed by microscope, and from the area, tissues were obtained using a punch 3 mm in diameter, and 30 cases of tissues per array block were aligned.
The paraffin-embedded tissue array blocks were sectioned at 4 µm thickness, attached to slides, and after performing the deparaffinization and hydration process, using a commercialized HER2 FISH kit (Vysis Inc, Downers Grove, Ill), experiments were performed according to the guideline of the manufacturer. First, the samples were treated with diluted wash buffer for 2 min, treated with pre-treatment solution at 95-99℃ for 10 min, and washed with wash buffer for 3 min twice. The samples were treated with pepsin reagent for 10 min, washed with wash buffer for 3 min twice, and dehydrated. Subsequently, the samples were treated with HER2/CEN-17 Probe Mix at 82℃ for 5 min, incubated in a 45℃ humidified hybridization chamber for 14-20 hr, and treated with stringent wash buffer at 65℃ for 10 min. Washed again with wash buffer for 3 min twice, the samples were dehydrated, and a fluorescent mounting solution containing 4'-6-diamidine-2-phenylindole (DAPI) was applied to slides and read. In normal cells, CEN-17 DNA probe bound to the centromere area of chromosome 17 and thus 1-2 green fluorescent signal was shown, and HER2 DNA probe bound to the HER2 gene and thus 1-2 red fluorescent signal was shown, and the cases whose HER2/CEN-17 ratio was higher than 2 were considered to be positive for the amplification of HER2 gene.
Through the examination of the medical records of the subject patients and the records of the visit to our outpatient clinic, the survival status of patients was assessed, and for patients who did not have the record of the visit to hospital for longer than 6 months, the survival survey was performed by telephone. The analysis of the survival of patients was performed by obtaining the Kaplan-Meier survival curve. Comparing and analyzing survival data by Log-rank test. The determination of independent prognostic factors on the survival was performed by multivariate analysis by applying Cox regression model. A p value less than 0.05 was considered to be statistically significant.
The median age of the entire subjects was 48 yr, and the median duration of follow-ups was 6.3 yr (Table 1). With regard to the distribution of the stages of breast cancer, the stage I was 58 cases (17.2%), the stage II was 184 cases (54.4%), and the stage III was 96 cases (28.4%), and concerning surgical treatment, mastectomy was performed on 301 cases (89.0%), and postoperative adjuvant chemotherapy and hormone therapy were performed by considering the status of lymph node metastasis and hormone receptor test. In the status of hormone receptors of breast cancer, of 288 tested cases, 190 cases (66.0%) were found to be positive, and in the HER2 test by FISH of breast cancer, positive results meaning the amplification of the HER2 gene was shown in 89 cases of the total 388 cases (26.3%).
In 89 cases showing the result of the amplification of HER2 gene in breast cancer, the positivity was examined according to the stage (Table 2). The positive result was detected in 6 cases of the stage I (10.3%), 41 cases in the stage II (22.3%), and 42 cases in the stage 3 (43.8%), hence, it was found that the positive rate became higher as the disease stage progressed.
In the survival analysis based on the disease-free period, the 5-yr survival rate according to the amplification of HER2 gene showed different results among the stages of breast cancer (Fig. 1). In the stage I breast cancer, the 5-yr disease-free survival (DFS) rate of the HER2 gene positive group was 100%, the survival rate of the negative group was 85%, and the survival rate of the positive group was higher, but it was not statistically significant (p=0.2053). In the stage II breast cancer, the 5-yr DFS rate of the positive group was 85%, that of the negative group was 87%, and a difference was not significant (p=0.3855). However, in the stage III breast cancer, the DFS rate of positive group was 41%, that of the negative group was 70.5%, and the DFS rate of the HER2 gene-positive group was significantly lower (p=0.0090).
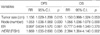
In the survival analysis based on the overall survival period, similarly, the 5-yr survival rate according to the amplification of HER2 gene showed different results depending on the stages of breast cancer (Fig. 2). In the stage I breast cancer, the 5-yr overall survival (OS) rate of the HER2-positive group was 100% and that of the negative group was 94%. In the stage II breast cancer, the OS rate of the positive group was 88% and that of the negative group was 92.5%, and the difference was not significant (p=0.5927 in the stage I, p=0.8566 stage II). However, in the stage III breast cancer, the 5-yr OS rate of the HER2-positive group was 28% and that of the negative group was 60%, and the difference was significant (p=0.0034).
To examine prognostic factors that independently influence the disease-free survival and the overall survival, multivariate analysis was performed by Cox regression model (Table 3). As an important prognostic factor influencing recurrence and death, the statistical significance of the positive finding of HER2 was confirmed. The risk of recurrence of the HER2 gene amplification-positive group was 1.669 times higher than that of the negative group (p=0.036), and the risk of death was 2.394 times higher (p=0.003). On the other hand, in the same analysis performed according to the disease stage, the amplification of HER2 gene did not show any significant effect on recurrence and survival in the disease stage I and II breast cancer, but in the stage III breast cancer, increased the risk of recurrence by 2.678 times (p=0.002) and the risk of death by 2.576 times (p=0.005). Therefore, the significance as a prognostic factor could be confirmed only in the stage III breast cancer (Table 4).
The significance of this study is that the amplification of the HER2 gene, which has been reported to be closely associated with the prognosis of breast cancer, was re-examined and the effect on the prognosis of the same stage breast cancer was assessed by survival analysis based on the long-term follow-ups over than 5 yr. As mentioned already in the introduction, to raise the reliability of HER2 test, in our study, HER2 results were assessed by gene amplification test using FISH, which could be also considered to be greatly meaningful for the understanding of the significance HER2 as a prognostic factor. However, this study was performed retrospectively and the number of patients in stage I was relatively small to that of other stages due to the retrospective selection of appropriate tissues of breast cancer for HER2 FISH test and survival analyses. These would be a limitation of this study.
Generally, the positive rate of HER2 in breast cancer has been reported to be 20-30% (14-17), and in our study, similarly, the positive rate of the amplification of HER2 was found to be 26.3%, and thus it could be confirmed. Nevertheless, HER2-positive rate showed a difference depending on the stage of breast cancer, and the positive result was shown in 10.3% in the stage I, 22.3% in stage II, and 43.8% in the stage III. This result suggests that as the disease stage of breast cancer is advanced, HER2-positive rate increases, and HER2 positivity is closely associated with high stage of breast cancer, that is, poor prognosis (18-20).
According to the summary of HER2 of breast cancer reported until 1998 by Revillion et al. (18), HER2-positive result was a marker representing the aggressiveness of tumors and showed poor prognosis, nonetheless, because of the association with other strong prognostic factors, it did not have a clinically important significance. Slamon et al. (16) and Tandon et al. (21) have reported that the amplification of the HER2 gene in breast cancer assessed by Southern blot had been associated with poor prognosis and these results had been found only in the lymph node positive group, but not in the lymph node negative group. These results are similar to our results in this study. We stratified the patients not by nodal status but by stages of breast cancer to exclude the influence of other prognostic factors such as tumor size, hormonal status as well as nodal status. In this study the pure prognostic effect of HER2 gene amplification was noted only in stage III patients of breast cancer, not in stage I or II. We could suggest an explanation for these results that the advance of breast cancer would be associated with the increased amplification of the HER2 gene and the longer duration of HER2 gene action than in early breast cancer (22), therefore, stage III of breast cancers in this study might have taken sufficient chances to express harmful effects on their survival not only by HER2 signal transduction pathway but also by crosstalks with other signal transduction pathways such as ER pathway.
On the other hand, Borg et al. (23) have reported that, with the result obtained by the same method, the amplification of HER2 gene did not influence prognosis in both lymph node -positive and -negative group. Afterwards, in numerous results applied immunohistochemical staining method, similar results were shown (24, 25), and until now, a clear conclusion could not be reached and it is a controversial issue.
HER2 as a prognostic factor assessed by multivariate analysis, the amplification of the HER2 gene was confirmed to increase the risk of recurrence by 1.669 times (p=0.0036), and the risk of death by 2.394 times (p=0.002) in overall cases of breast cancer. However, our result showed that the effect of the amplification of HER2 gene differs depending on the disease stage. In other words, the prognosis of the HER2 gene amplification group was poor only in the stage III breast cancer, and in the stage I and II breast cancer, a statistically significant difference from the negative group was not detected. In multivariate analysis performed according to the stage of breast cancer, as the disease stage is advanced, the amplification of the HER2 gene was associated with a high risk level of death, however, the statistical significance was noted only in the stage III breast cancer. Therefore, based on the result of our study, it could be confirmed that the amplification of the HER2 gene exerts a poor effect only on the prognosis of advanced breast cancer.
In conclusion, the amplification of the HER2 gene in breast cancer confirmed by FISH was associated with the progression of the disease stage of breast cancer, and the clinical significance as a prognostic factor might be confined only in advanced breast cancer.
Figures and Tables
Fig. 1
Disease-free survival (DFS) curves according to the stages of breast cancer. (A) stage I (B) stage II (C) stage III. Statistical significance between HER2 gene amplification -positive group (solid line) and -negative group (dotted line) was noted only in stage III of breast cancer.
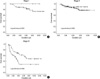
Fig. 2
Overall survival (OS) curves according to the stages of breast cancer. (A) stage I (B) stage II (C) stage III. Statistical significance between HER2 gene amplification -positive group (solid line) and -negative group (dotted line) was noted only in stage III of breast cancer.

References
1. Veronesi U, Viale G, Rotmensz N, Goldhirsch A. Rethinking TNM: Breast cancer TNM classification for treatment decision-making and research. Breast. 2006. 15:3–8.

2. Dykins R, Corbett IP, Henry JA, Wright C, Yuan J, Hennessy C, Lennard TJ, Angus B, Horne CH. Long-term survival in breast cancer related to overexpression of the c-erbB-2 oncoprotein: an immunohistochemical study using monoclonal antibody NCL-CB11. J Pathol. 1991. 163:105–110.

3. Andrulis IL, Bull SB, Blackstein ME, Sutherland D, Mak C, Sidlofsky S, Pritzker KP, Hartwick RW, Hanna W, Lickley L, Wilkinson R, Qizilbash A, Ambus U, Lipa M, Weizel H, Katz A, Baida M, Mariz S, Stoik G, Dacamara P, Strongitharm D, Geddie W, McCready D. neu/erbB-2 amplification identifies a poor-prognosis group of women with node-negative breast cancer. Toronto Breast Cancer Study Group. J Clin Oncol. 1998. 16:1340–1349.

4. Hartmann LC, Ingle JN, Wold LE, Farr GH Jr, Grill JP, Su JQ, Maihle NJ, Krook JE, Witzig TE, Roche PC. Prognostic value of c-erbB2 overexpression in axillary lymph node positive breast cancer. Results from a randomized adjuvant treatment protocol. Cancer. 1994. 74:2956–2963.

5. Press MF, Pike MC, Chazin VR, Hung G, Udove JA, Markowicz M, Danyluk J, Godolphin W, Sliwkowski M, Akita R, Paterson MC, Slammon DJ. Her-2/neu expression in node-negative breast cancer: direct tissue quantitation by computerized image analysis and association of overexpression with increased risk of recurrent disease. Cancer Res. 1993. 53:4960–4970.
6. Seshadri R, Firgaira FA, Horsfall DJ, McCaul K, Setlur V, Kitchen P. Clinical significance of HER-2/neu oncogene amplification in primary breast cancer. The South Australian Breast Cancer Study Group. J Clin Oncol. 1993. 11:1936–1942.

7. Tetu B, Brisson J. Prognostic significance of HER-2/neu oncoprotein expression in node-positive breast cancer. The influence of the pattern of immunostaining and adjuvant therapy. Cancer. 1994. 73:2359–2365.

8. Bianchi S, Paglierani M, Zampi G, Cardona G, Cataliotti L, Bonardi R, Ciatto S. Prognostic significance of c-erbB-2 expression in node negative breast cancer. Br J Cancer. 1993. 67:625–629.

9. Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, Swain SM, Pisansky TM, Fehrenbacher L, Kutteh LA, Vogel VG, Visscher DW, Yothers G, Jenkins RB, Brown AM, Dakhil SR, Mamounas EP, Lingle WL, Klein PM, Ingle JN, Wolmark N. Trastzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005. 353:1673–1684.
10. Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, Cameron D, Dowsett M, Barrios CH, Steger G, Huang CS, Andersson M, Inbar M, Lichinitser M, Láng I, Nitz U, Iwata H, Thomssen C, Lohrisch C, Suter TM, Rüschoff J, Suto T, Greatorex V, Ward C, Straehle C, McFadden E, Dolci MS, Gelber RD; Herceptin Adjuvant (HERA) Trial Study Team. Trastzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005. 353:1659–1672.
11. Ellis CM, Dyson MJ, Stephenson TJ, Maltby EL. HER2 amplification status in breast cancer: a comparison between immunohistochemical staining and fuorescence in situ hybridization using manual and automated quantitative image analysis scoring techniques. J Clin Pathol. 2005. 58:710–714.
12. Press MF, Bernstein L, Thomas PA, Meisner LF, Zhou JY, Ma Y, Hung G, Robinson RA, Harris C, El-Naggar A, Slamon DJ, Phillips RN, Ross JS, Wolman SR, Flom KJ. HER-2/neu gene amplification characterized by fluorescence in situ hybridization: poor prognosis in node-negative breast carcinomas. J Clin Oncol. 1997. 15:2894–2904.

13. Ratcliffe N, Wells W, Wheeler K, Memoli V. The combination of in situ hybridization and immunohistochemical analysis: an evaluation of Her2/neu expression in paraffin-embedded breast carcinomas and adjacent normal-appearing breast epithelium. Mod Pathol. 1997. 10:1247–1252.
14. Kallioniemi OP, Kallioniemi A, Kurisu W, Thor A, Chen LC, Smith HS, Waldman FM, Pinkel D, Gray JW. ERBB2 amplification in breast cancer analyzed by fluorescence in situ hybridization. Proc Natl Acad Sci USA. 1992. 89:5321–5325.

15. Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987. 235:177–182.

16. Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A, Press MF. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989. 244:707–712.

17. Thor AD, Schwartz LH, Koerner FC, Edgerton SM, Skates SJ, Yin S, McKenzie SJ, Panicali DL, Marks PJ, Fingert HJ, Wood WC. Analysis of c-erbB-2 expression in breast carcinomas with clinical follow-up. Cancer Res. 1989. 49:7147–7152.
18. Revillion F, Bonneterre J, Peyrat JP. ERBB2 oncogene in human breast cancer and its clinical significance. Eur J Cancer. 1998. 34:791–808.
19. Ross JS, Fletcher JA. The HER-2/neu oncogene in breast cancer: prognostic factor, predictive factor, and target for therapy. Stem Cells. 1998. 16:413–428.
20. Tagliabue E, Menard S, Robertson JF, Harris L. c-erbB-2 expression in primary breast cancer. Int J Biol Markers. 1999. 14:16–26.

21. Tandon AK, Clark GM, Chamness GC, Ullrich A, McGuire WL. HER-2/neu oncogene protein and prognosis in breast cancer. J Clin Oncol. 1989. 7:1120–1128.

22. Mylonas I, Makovitzky J, Jeschke U, Briese V, Friese K, Gerber B. Expression of Her2/neu, steroid receptors (ER and PR), Ki67 and p53 in invasive mammary ductal carcinoma associated with ductal carcinoma In Situ (DCIS) Versus invasive breast cancer alone. Anticancer Res. 2005. 25:1719–1723.
23. Borg A, Tandon AK, Sigurdsson H, Clark GM, Ferno M, Fuqua SA, Killander D, McGuire WL. HER-2/neu amplification predicts poor survival in node-positive breast cancer. Cancer Res. 1990. 50:4332–4337.
24. Rosen PP, Lesser ML, Arroyo CD, Cranor M, Borgan P, Norton L. Immunohistochemical detection of HER-2/neu in patients with axillary lymph node negative breast carcinoma. A study of epidemiologic risk factors, histologic features, and prognosis. Cancer. 1995. 75:1320–1326.
25. Reed W, Hannisdal E, Boehler PJ, Gundersen S, Host H, Marthin J. The prognostic value of p53 and C-erb-B2 immunostaining is overrated for patients with lymph node-negative breast carcinoma?: a multivariate analysis of prognostic factors in 613 patients with a follow up of 14-30 years. Cancer. 2000. 88:804–813.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download