Abstract
This study was performed to estimate the rate of boosted reaction in the two-step tuberculin skin test (TST) and to evaluate the associated factors among military personnel of South Korea, which has an intermediate burden of tuberculosis (TB) and a routine bacille Calmette-Guérin (BCG) vaccination policy. Two-step TST was performed on 264 military personnel who did not have a history of close contact to TB. Subjects with a negative reaction to the first test of <10 mm had a second TST applied 1 week later on the other forearm. A positive result (≥10 mm) on the initial TST was observed in 126 (48%) of the subjects. A boosted reaction on the second TST developed in 32 (23%) of the 124 subjects with a negative initial TST. In multiple logistic regression analysis, the size of the initial TST reaction was the only factor associated with a boosted reaction on the second TST. The high rate of boosted reaction among healthy adults in South Korea suggests that two-step TST should be performed to assess the baseline TST reactivity in settings with an intermediate burden of TB and routine BCG vaccination policy, especially among subjects with an initial TST reaction that is ≥5 mm.
Although several novel diagnostic tests for tuberculosis infection have been developed and commercially licensed in recent years, the tuberculin skin test (TST) is still widely used for identifying latent tuberculosis infection (LTBI). Several difficulties exist, however, in the application and interpretation of the TST. For example, the reaction may be accentuated on repeated test, which can cause the test to be misinterpreted as a skin test conversion (1). The prevalence of boosted reaction is generally correlated with the prevalence of initial tuberculin reactions and is particularly common in individuals who have been vaccinated with bacille Calmette-Guérin (BCG) (1-4). Therefore, an evaluation of the prevalence of boosted reaction and the associated factors would be important for the assessment of TST reactivity in countries that have a high prevalence of tuberculosis (TB) and a routine BCG vaccination policy (3, 5-7). However, no published data exist on the boosted reaction in an adult South Korean population, which has an intermediate incidence of TB (96 cases per 100,000 population per year) (8) and a national policy of mass BCG vaccination.
The objectives of this study were to estimate the rate of boosted reaction and to evaluate the associated factors among military personnel in a setting with an intermediate burden of TB and routine BCG vaccination policy.
Some South Korean troops, mostly engineers, have been operating in Afghanistan on a 6-month rotation since 2002 to help with the reconstruction effort in that war-torn country. As part of the TB control program of the Armed Forces Medical Command, Republic of Korea, the troops dispatched to Afghanistan, which have shown a high incidence of TB (168 cases per 100,000 population per year) (8), have undergone screening tests for TB in addition to a medical examination before and after deployment at the Armed Forces Capital Hospital since 2006.
We performed two-step TSTs on the troops that were to be dispatched to Afghanistan for 6-month missions as described above in August 2006 with the approval of the ethics committee of the Armed Forces Medical Command and after obtaining informed consent from each subject. Before the skin tests were performed, the troops completed questionnaires about previous TSTs, potential exposure to TB, treatment for TB, and other demographic data. Subjects were excluded from this study if they had a documented history of TB or a history of close contact to TB. Because the records of previous BCG vaccination were not available for most subjects, the presence of a typical BCG scar was accepted to indicate previous BCG vaccination (9).
TSTs were administered by injecting 0.1 mL of 2 tuberculin units of purified protein derivative (RT 23; Statens Serum Institute, Copenhagen, Denmark) into the anterior surface of the forearm with disposable syringes and 27-gauge needles using the intradermal Mantoux method. Reactions were read 48-72 hr after the injection by a trained nurse, and the largest transverse diameter of palpable induration was recorded in millimeters. At the time of reading, the nurse was unaware of each subject's BCG vaccination status. A positive TST result was defined as an induration of 10 mm or more in diameter. Subjects with a reaction of <10 mm to the first test had a second TST applied 1 week later on the other forearm. The techniques for testing and reading were the same as for the initial TST. A boosted reaction was defined as a reaction of ≥10 mm on the second TST with a ≥6 mm increase than on the first TST result (4).
Data were analyzed using SPSS 12.0 (SPSS Inc, Chicago, IL, U.S.A.). To evaluate possible association between boosting reaction and variables, odds ratio with 95% confidence intervals (95% CI) were calculated. The likelihood ratio test was used to assess the significance of this association. Then, multiple logistic regression analysis was used to determine the independent factors associated with boosting reaction.
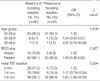
In total, 264 troops were recruited to have a medical examination during the study period. Of these troops, 126 (48%) had a positive result on the initial TST and were excluded from further testing. Of the remaining 138 subjects with a negative initial TST (≤9 mm), 14 subjects refused the second TST and were excluded. The characteristics of the remaining 124 (47%) subjects are presented in Table 1. The subjects ranged in age from 20 to 47 yr, with a median age of 22 yr, and all of the subjects were male. None of the subjects had a previous history of TST. Abnormal findings were not observed on chest radiography or in the other laboratory tests performed for the medical examination. A BCG scar was present in 112 subjects (90%), and boosted reaction was observed in 32 (23%) subjects. As shown in Table 2, boosted reaction was not associated with increasing age or the presence of a BCG scar (p=0.618 and 0.427, respectively). The size of the initial TST reaction was significantly associated with boosted reaction (p=0.004). In multiple logistic regression analysis, the size of the initial TST reaction was the only factor associated with boosted reaction on the second TST (Table 3).
In the present study of the TST reactivity in Korean military personnel, boosted reaction on the second TST developed in 23% of the subjects with a negative reaction on the initial TST and was associated with the size of the initial TST reaction.
The definitions of a boosted reaction have differed in previous studies, and the rates of boosted reactions for two-step TSTs have ranged from 0 to 59% (5-7, 10-19). The variation in the rates of boosted reactions among the different studies reflects differences in the populations studied regarding age, BCG vaccination status, and previous exposure to TB or nontuberculous mycobacteria. Therefore, our finding was expected to be similar to a study performed in Turkey, which is characterized by an intermediate incidence of TB and a routine BCG vaccination program as in South Korea; that study found high positive rates of boosted reactions (21%) (6). Even though the majority of our subjects were younger than 30 yr (89%), our rate of boosted reactions was 11-17% higher than the rates reported by two other studies performed in countries with a high prevalence of TB and routine BCG vaccination (5, 7). This difference might be attributable to the different proportions of males, who are reportedly more likely to be positive of boosted reaction (11, 20).
Previous BCG vaccination has been reported to be one of the most influential factors for boosted reaction (10, 12, 13, 16, 19, 20). In the present study, however, the presence of a BCG scar was not associated with an increased rate of boosted reaction. The lack of a BCG effect in our subjects could have occurred because most BCG vaccinations in Korea are performed during infancy; the prevalence of a BCG scar in infants was approximately 88% during the seventh nationwide TB prevalence survey in Korea (21). Menzies et al. (12) reported that BCG vaccination received in infancy has little effect on the boosted reaction. In addition, previous studies have documented a relationship between increasing age and boosted reaction (5, 11-13); therefore, it is likely that we did not observe a statistically significant relationship because of the small number of older subjects in our study population.
The prevalence of an initial TST reaction has been correlated with the prevalence of the boosted reaction (12, 22, 23). We found that the rate of positive boosted reaction as the size of the initial TST reaction increased. Menzies et al. (12) reported a frequency of boosted reactions of 3.7, 17.1, and 28.4% in subjects whose initial TST reactions measured 0, 1-4, and 5-9 mm, respectively. Alvarez et al. (22) found that the rate of boosted reactions was 12.7 and 35.5% in subjects with an initial reaction measuring 0-4 and 5-9 mm, respectively. In the present study, the rates of boosted reactions were 10, 25, and 38% in subjects with an initial TST reaction measuring 0, 1-4, and 5-9 mm, respectively (p=0.004), and the size of the initial TST reaction was the only factor associated with boosted reaction on the second TST in multiple logistic regression analysis.
Health care workers are at high risk for TB, and screening of health care workers for TB is an important component of infection control programs (1). However, little is known about the TST reactivity in an adult South Korean population. This is the first study to report the boosted reaction in an adult South Korean population. Therefore, our results suggest that the boosted reaction on repeated test should be considered when TB screening of health care workers, who are likely to receive periodic retesting, would be performed hereafter in South Korea.
In conclusion, the prevalence of boosted reaction on repeated TST was high among adults in a setting with an intermediate burden of TB and routine BCG vaccination policy, and the size of the initial TST reaction was the only associated factor on multiple logistic regression analysis. Therefore, to avoid misinterpreting the boosted reaction on subsequent TST as a conversion, the use of a two-step TST would be necessary to assess the baseline TST reactivity among subjects with a negative reaction on initial TST, especially when the size of the initial TST is >5 mm.
Figures and Tables
References
1. American Thoracic Society. Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med. 2000. 161:S221–S247.
2. Farhat M, Greenaway C, Pai M, Menzies D. False-positive tuberculin skin tests: what is the absolute effect of BCG and non-tuberculous mycobacteria? Int J Tuberc Lung Dis. 2006. 10:1192–1204.
3. Joos TJ, Miller WC, Murdoch DM. Tuberculin reactivity in bacille Calmette-Guerin vaccinated populations: a compilation of international data. Int J Tuberc Lung Dis. 2006. 10:883–891.
4. Menzies D. Interpretation of repeated tuberculin tests. Boosting, conversion, and reversion. Am J Respir Crit Care Med. 1999. 159:15–21.
5. Al Mazrou AM. Booster effect of two-step tuberculin skin testing among hospital employees from areas with a high prevalence of tuberculosis. Infect Control Hosp Epidemiol. 2004. 25:1117–1120.

6. Hizel K, Maral I, Karakus R, Aktas F. The influence of BCG immunisation on tuberculin reactivity and booster effect in adults in a country with a high prevalence of tuberculosis. Clin Microbiol Infect. 2004. 10:980–983.

7. Salles CG, Ruffino-Netto A, Lapa-e-Silva JR, Kritski AL, Cailleaux-Cesar M, Queiroz-Mello FC, Conde MB. The presence of a booster phenomenon among contacts of active pulmonary tuberculosis cases: a retrospective cohort. BMC Public Health. 2007. 7:38.

8. World Health Organization. Global tuberculosis control: surveillance, planning, financing. WHO report 2007. 2007. Geneva, Switzerland:
9. Choi CM, Kang CI, Kim DH, Kim CH, Kim HJ, Lee CH, Yim JJ. The role of TST in the diagnosis of latent tuberculosis infection among military personnel in South Korea. Int J Tuberc Lung Dis. 2006. 10:1342–1346.
10. Cauthen GM, Snider DE Jr, Onorato IM. Boosting of tuberculin sensitivity among Southeast Asian refugees. Am J Respir Crit Care Med. 1994. 149:1597–1600.

11. Frenzel EC, Thomas GA, Hanna HA. The importance of two-step tuberculin skin testing for newly employed healthcare workers. Infect Control Hosp Epidemiol. 2006. 27:512–514.

12. Menzies R, Vissandjee B, Rocher I, St Germain Y. The booster effect in two-step tuberculin testing among young adults in Montreal. Ann Intern Med. 1994. 120:190–198.

13. Moreno S, Blazquez R, Novoa A, Carpena I, Menasalvas A, Ramírez C, Guerrero C. The effect of BCG vaccination on tuberculin reactivity and the booster effect among hospital employees. Arch Intern Med. 2001. 161:1760–1765.

14. Morse DL, Hansen RE, Grabau JC, Cauthen G, Redmond SR, Hyde RW. Tuberculin conversions in Indochinese refugees. An assessment of boosting and anergy. Am Rev Respir Dis. 1985. 132:516–519.
15. Morse DL, Hansen RE, Swalbach WG, Redmond SR, Grabau JC. High rate of tuberculin conversion in Indochinese refugees. JAMA. 1982. 248:2983–2986.

16. Sepulveda RL, Ferrer X, Latrach C, Sorensen RU. The influence of Calmette-Guerin bacillus immunization on the booster effect of tuberculin testing in healthy young adults. Am Rev Respir Dis. 1990. 142:24–28.
17. Sherman RA, Shimoda KJ. Tuberculosis tracking: determining the frequency of the booster effect in patients and staff. Am J Infect Control. 2001. 29:7–12.

18. Srour-Fihmi S, Weiler-Ravell D, Kitzes R, Chemtob D. Routine two-step skin testing for tuberculosis in the staff of a geriatric hospital in Israel: booster and conversion rates. J Hosp Infect. 2000. 46:141–146.

19. Wang PD. Two-step tuberculin testing of passengers and crew on a commercial airplane. Am J Infect Control. 2000. 28:233–238.

20. Sepkowitz KA, Feldman J, Louther J, Rivera P, Villa N, DeHovitz J. Benefit of two-step PPD testing of new employees at a New York City hospital. Am J Infect Control. 1997. 25:283–286.

21. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998. 2:27–36.
22. Alvarez S, Kasprzyk DR, Freundl M. Two-stage skin testing for tuberculosis in a domiciliary population. Am Rev Respir Dis. 1987. 136:1193–1196.

23. Welty C, Burstin S, Muspratt S, Tager IB. Epidemiology of tuberculous infection in a chronic care population. Am Rev Respir Dis. 1985. 132:133–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download