Abstract
In the present study, the authors investigated the management of mechanical valve thrombosis (MVT). From January 1981 through March 2006, 2,908 mechanical valve replacements were performed in 2,298 patients at our institution. Twenty (0.87%) patients presented with MVT, 14 (70.0%) were women, and the mean age of the patients was 42.0±14.0 (27-66) yr. Thrombosis involved mitral in 14 (70.0%), aortic in 2 (10.0%), tricuspid/aortic in 1 (5%), and tricuspid in 3 (15%). The interval from first operation to valve thrombosis was 121.8±75.4 (0.9-284.7) months. The most frequent clinical presentation was heart failure (13/20, 65%), and predisposing causes of MVT were: poor compliance with warfarin (7), pregnancy (5), drug interaction (2), and unknown (6). All 20 patients underwent valve replacement: mitral (14, 70.0%), tricuspid (3, 15.0%), aortic (2, 10%) and tricuspid/aortic (1, 5%). One early death occurred due to left ventricular failure, but no late mortality occurred during 63.3±49.9 (0.5-165.1) months of follow-up. MVT was treated successfully, and pregnancy and inadequate anticoagulation were found to influence the occurrence of this rare complication.
Mechanical valve thrombosis (MVT) may cause valve dysfunction, and its onset may be acute or gradual, according to the nature of thrombi (rapid or slow growth) and involvement of hinge point (abrupt or insidious). Edmunds defined mechanical valve thrombosis as a complication attributable to any type of thrombus, without evidence of infection, attached around a mechanical valve, deranging hemodynamics, or interfering with valvular function (1). The risk of valve thrombosis is highest in the tricuspid position, with reported rates as high as 20% (2), while the incidence of left side valve thrombosis varies from 4% to 8.6% within 5 yr of initial valve replacement (3, 4). Eleven-year probability of prosthetic valve thrombosis has been reported to be 0.01% to 0.02% in the mitral or aortic position (5), and tilting disc valves are most commonly reported in association with this complication (6). Detection of valve thrombosis may be easy or difficult, and if valve thrombosis is suspected, transthoracic echocardiographic evaluation can be used to confirm the diagnosis (7). Transesophageal echocardiographic examination is often necessary in the mitral position because of the thrombi involvement along the left atrial side of the sewing ring (8). Several factors such as inadequate anticoagulation, drug interaction, pannus overgrowth, and pregnancy have been suggested to promote valve thrombosis (9). This analysis was undertaken to evaluate the risk factors and outcome of mechanical valve thrombosis in patients who had undergone valve replacement.
Between January 1981 and March 2006, 2,908 mechanical valve replacements were performed in 2,298 patients. Among these, 20 patients underwent surgical intervention due to MVT. We included only surgical cases of MVT. Thrombosis treated by thrombolysis was excluded. Hospital records were reviewed retrospectively, including; preoperative clinical findings, initial valve procedures and etiologies, any type of event during follow-up or anticoagulation, diagnostic methods and characteristics of valve thrombosis, perioperative management, and outcomes. Several factors were evaluated to identify risk factors of MVT development; including sex, valve location, and number of valves replaced.
Twenty patients presented with MVT, 6 (30%) men and 14 (70%) women. Valve replacement involved a single valve in 13 patients (65%), and double valve replacement was done in 7 patients (35%) (Table 1). Implanted prosthetic valves were listed in Table 1. One patient had a history of cerebral embolism and another patient had a history of unilateral lower extremity edema. Left atrial appendage resection was performed in 4 (20%), and the Cox-Maze procedure in 4 (20%). The mean postoperative left ventricular ejection fraction was 57±9.3%, and the mean initial hospital stay was 16.9±6.7 days.
Anticoagulation (heparin and warfarin) was started 24 to 48 hr after all valvular procedures. Patients were discharged with an international normalized ratio (INR) level of 2.0 to 2.5 for mitral and aortic valve replacement cases and of 2.5 to 3.0 for tricuspid valve replacement cases.
The mean age at MVT diagnosis was 42.0±14.0 (27-66) yr. The distribution of MVTs according to the site of valve implantation was as follows: 14 (70%) mitral, 3 (15%) tricuspid, 2 (10%) aortic, and 1 (5%) tricuspid/aortic. Among double-valve prosthesis recipients (7), MVTs were in a mitral prosthesis in 3, an aortic prosthesis in 3, and in a tricuspid prosthesis in 2. Only one case of aortic and tricuspid valve replacement had bivalvular thrombosis.
The mean time from first valve replacement to prosthetic valve thrombosis was 121.8±75.4 (0.9-284.7, median 96.0)months. There was 1 early thrombosis and 19 late thromboses(Table 2). The mean time between the diagnosis ofMVT and surgical treatment was 22.3±42.5 days (range,0-180 days). Eight patients (40%) underwent an emergency or urgent operation.
The most frequent clinical presentation was congestive heart failure (13/20, 65%). Symptoms at presentation were dyspnea in 12 (60%) patients, cardiogenic shock in 1 (5%) patient, and miscellaneous symptoms (myalgia, cough, or fever) in 2 (10%) patients (Table 2). In five patients, MVT was an incidental fortuitous echocardiographic finding (Table 2). The majority of patients (11, 55%) with MVT were of NYHA functional class III or IV at the time of diagnosis. The mean duration between symptom onset and surgical treatment was 87.8±121.7 days (range, 0-365 days). Thromboembolism (stroke, limb or organ ischemia) occurred between initial valve replacement and valve thrombosis in 2 (10%) patients.
MVT was diagnosed by transthoracic echocardiography (TTE) in 13 (65%) patients, and by transesophageal echocardiography (TEE) in 7 (35%) patients. INR profiles when thrombosis was diagnosed were 1.66±0.64 (1.02-2.68) for left-sided valves and 1.42±0.53 (1.07-2.03) for tricuspid valves. Six patients were in target INR when valve thrombosis occurred.
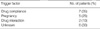
MVT occurred during pregnancy in 7 (35%) patients, and of these, two patients had a history of denying warfarin for fear of possible embryopathy. We classified them as poor compliance category. One patient experienced thrombosis at full term and underwent valve replacement, 2 days later she had a normal full term baby without any adverse event. Poor compliance with anticoagulant treatment leading to a lower INR than recommended was responsible for MVT in another 5 (25%) patients. Adding two patients with pregnancy, poor warfarin compliance was responsible for 7 patients (35%). These patients skipped warfarin for no distinct reason, and their compliances with treatment and medication were poor. In 2 (10%) patients MVT was thought to be related to a drug interaction, i.e., one received medication for a common cold 1 week before thrombosis detection and the other patient had consumed nutritional supplements with or without medication. One patient with a Bjork-Shiley convexo-concave tilting disc valve did not take any warfarin probably due to poor compliance. He did not take medications for 285 months, and we could not follow him up. He presented at out clinic due to cold sweating and dyspnea 3 weeks before a diagnosis of MVT. No specific causes were identified in 6 (30%) patients. Possible factors precipitating MVT are listed in Table 3. We detected valve thrombosis during follow-up echocardiography. Pannus formation was present with thrombus at the time of operation in 45% (9/20) of the patients.
All patients were started on intravenous heparin. Two (10%) of the 20 received streptokinase-based thrombolytic therapy, but it was not successful. One patient had acute mitral valve thrombosis, and due to hemodynamic instability, the patient received thrombolysis. The other patient had acute tricuspid valve thrombosis. Both were treated by surgical intervention and have been in good physical condition until now. All patients underwent surgery under redomedian sternotomy, consisting of mitral valve replacement in 14 patients (70.0%), tricuspid valve replacement in 3 patients (15.0%), aortic valve replacement in 2 (10%), and tricuspid/ aortic valve replacement in one (5%). Thrombi were found around valve hinge points and sewing rings, and all valves concerned were replaced other than thrombectomy. The majority of patients underwent bileaflet mechanical valve replacement. Only one patient received a tissue valve; she was 65 yr at the time of diagnosis, and she was non-compliant to warfarin with a frequent bleeding history.
The aortic cross clamping time averaged 104.9±42.8 min (range, 52-191 min), and the cardiopulmonary bypass time was 164.6±62.7 min (range, 79-286 min). Emergent or urgent operation was done in 8 cases (40%) due to heart failure and hemodynamic compromise. There was one operative death (5%) due to cardiopulmonary weaning failure. Early complications were atrial fibrillation (3), bleeding (1), vocal cord paralysis (1), cerebral infarction (1), atrioventricular conduction block (1), and pneumonia (1).
Oral anticoagulation after surgical treatment consisted of warfarin alone in 16 (16/19, 83%) patients and a combination of warfarin and plavix in 3 (3/19, 17%) patients. The mean hospital stay was 18.5±18.0 (range, 8-89) days, and the mean intensive care unit stay was 3.3±2.4 days (range, 1-9) days. No late mortality or MVT recurrence occurred over 63.3±49.9 (0.5-165.1) months of mean follow-up. A brief summary of clinical characteristics of all patients is provided in Table 4.
Our data show that MVT is a very rare complication after valve replacement and that its clinical manifestations are various. The time between initial valve replacement and diagnosis of MVT was 121.8±75.4 months, and the median was 96.0 months. In most cases, thrombosis occurred insidiously; only one patient presented with acute valve thrombosis one month after valve replacement. Durrleman et al. (10) reported 39 cases of prosthetic valve thrombosis with a 39.0 ±42.0-month mean interval of occurrence from initial operation and an in-hospital mortality of 41%. The difference between our series and Durrleman's data might be due to different patient populations. Some patients might have been lost, and possible unknown sudden death cannot be ruled out. Clinical course might depend on the type of replaced valves; patients with bileaflet mechanical valves might have had stable hemodynamics due to a well-functioning single leaflet or have had unstable vital signs due to bileaflet involvement. The fact is that the clinical manifestations of MVT are various.
During follow-up, we usually suspect valve thrombosis in cases with valve click loss, skipped warfarin, newly appeared symptoms, and so on. In the present study, TTE detected valve thrombosis in 75% of our series, and we found incidental valve thrombosis using this modality in five patients during routine echocardiographic follow-ups. In those cases, none had symptoms, and we could not follow with urgent operations. Detection of valve thrombosis may be difficult, and some series have reported that as many as 50% of cases are diagnosed postmortem (4).
In a recent study, the delay between first onset of symptoms and hospitalization was found (from 1 to 45 days) (11). Previous studies have shown that a delay in diagnosis and a long duration of symptoms result in a higher mortality (12). However, physical examination is an inadequate diagnostic tool and strong clinical suspicion is the most important to detect these complications. Any new or worsening symptoms in a patient with mechanical valve warrant a thorough investigation to exclude valve thrombosis. In the present series, MVT was diagnosed by TTE in 13 (65%) patients and by transesophageal echocardiography in 7 (35%) patients. During follow-up, we suggest a periodical echocardiographic examination. Early detection and diagnosis may often be limited by a progressive or insidious course. The difference of valve thrombosis incidence and the pattern of onset between tilting disc and bileaflet valve is still uncertain.
Another remarkable point of the present study is that pregnancy and inadequate anticoagulation influenced the occurrence of this complication. Buttard and colleagues (11) found inadequate anticoagulation at the time of diagnosis in 45% of their patients: 27% for medical reasons (surgical intervention, neurologic events, or pregnancy) and 17% because of poor drug compliance. A definite relationship has already been established between inadequate anticoagulation and valve thrombosis (11-14).
Anticoagulation during pregnancy is a difficult problem to solve, as pregnancy induces various biophysiologic changes and a hypercoagulable status. The risk of warfarinization during pregnancy is teratogenicity, particularly between the 6th and 12th weeks of gestation (15, 16). Therefore, it is obvious and mandatory to use anticoagulation extremely carefully to prevent valve thrombosis or thromboembolism. Our data also demonstrate difficulties in maintaining adequate anticoagulation during pregnancy; however, no safe and reliable protocol for anticoagulation therapy during pregnancy has been established (17).
Pannus formation, defined as excessive fibrosis around a prosthetic valve, may occur in 25% of patients as early as the first postoperative month (11). It plays an important role in the mechanism of obstruction and could be the sole cause of mechanical valve thrombosis occurrence (9). In the present series, the precise role of pannus in the pathogenesis of valve thrombosis remains unknown. We found pannus in 45% of patients. However, whether it caused valve thrombosis or not was still uncertain, so we did not include it as a cause of valve thrombosis.
Recently, Roudaut et al. (18) conducted a retrospective study of 110 patients treated with fibrinolytic therapy and concluded that this treatment should be reserved for selected patients (those with tricuspid thrombosis, critically ill patients, and patients with contraindications to surgical intervention). We consider that thrombolysis can be tried, especially in the tricuspid valve position. Thrombolysis appears to be useful as a medical bridge to operation and as a major curative modality when a patient's medical condition or hemodynamics is poor. In the present series, thrombolysis was attempted in two patients, but was not successful.
The present study shows that pregnancy and inadequate anticoagulation probably influenced the occurrence of this rare complication. However, our knowledge of MVT is still inadequate, and more efficient ways of eradicating this complication should be suggested.
Figures and Tables
Table 4
Brief summary of clinical characteristics of the patients

*, Right-sided atrioventricular valve in corrected transposition of great arteries.
Dx, diagnosis; Op, operation; AV, aortic valve; AVR, aortic valve replacement; MV, mitral valve; MVR, mitral valve replacement; TV, tricuspid valve; TVR, tricuspid valve replacement; M, male; F, female; CM, Carbomedics; SJ, ST. Jude; DM, Duromedics; BS, Bjork-Shiley; CE, Carpentier Edwards; OX, On-X; ET, Edwards TEKNA; P, pregnancy; P C, poor compliance; U, unknown; D I, drug interaction.
References
1. Edmunds LH Jr, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Guidelines for reporting morbidity and mortality after cardiac valvular operations. Ad hoc liaison committee for standardizing definitions of prosthetic heart valve morbidity of the American association for thoracic surgery and the society of thoracic surgeons. J Thorac Cardiovasc Surg. 1996. 112:708–711.
2. Thorburn CW, Morgan JJ, Shanahan MX, Chang VP. Long-term results of tricuspid valve replacement and the problem of prosthetic valve thrombosis. Am J Cardiol. 1983. 51:1128–1132.

3. Edmunds LH Jr. Thrombotic and bleeding complications of prosthetic heart valves. Ann Thorac Surg. 1987. 44:430–445.

4. Sivasubramanian S, Vijayshankar CS, Krishnamurthy SM, Santhosham R, Dwaraknath V, Rajaram S. Surgical management of prosthetic valve obstruction with the Sorin tilting disc pros. J Heart Valve Dis. 1996. 5:548–552.
5. Hammermeister KE, Sethi GK, Henderson WG, Oprian C, Kim T, Rahimtoola S. A comparison of outcomes in men 11 years after heart valve replacement with a mechanical valve or bioprosthesis. Veterans affairs cooperative study on valvular heart disease. N Engl J Med. 1993. 328:1289–1296.
6. Nunez L, Iglesias A, Sotillo J. Entrapment of leaflet of St. Jude medical cardiac valve prosthesis by minuscule thrombus: report of two cases. Ann Thorac Surg. 1980. 29:566–569.
7. Habib G, Cornen A, Mesana T, Monties JR, Djiane P, Luccioni R. Diagnosis of prosthetic heart valve thrombosis. The respective values of transthoracic and transesophageal Doppler echocardiography. Eur Heart J. 1993. 14:447–455.
8. Gueret P, Vignon P, Fournier P, Chabernaud JM, Gomez M, LaCroix P, Bensaid J. Transesophageal echocardiography for the diagnosis and management of nonobstructive thrombosis of mechanical mitral valve prosthesis. Circulation. 1995. 91:103–110.

9. Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction of mechanical heart valve prostheses: clinical aspects and surgical management. J Am Coll Cardiol. 1991. 17:646–650.

10. Dürrleman N, Pellerin M, Bouchard D, Hébert Y, Cartier R, Perrault LP, Basmadjian A, Carrier M. Prosthetic valve thrombosis: twenty-year experience at the Montreal Heart Institute. J Thorac Cardiovasc Surg. 2004. 127:1388–1392.

11. Buttard P, Bonnefoy E, Chevalier P, Marcaz PB, Robin J, Obadia JF, Kirkorian G, Touboul P. Mechanical cardiac valve thrombosis in patients in critical hemodynamic compromise. Eur J Cardiothorac Surg. 1997. 11:710–713.

12. Tsai KT, Lin PJ, Chang CH, Chu JJ, Chang JP, Kao CL, Hsiehet MJ. Surgical management of thrombotic disc valve. Ann Thorac Surg. 1993. 55:98–101.

13. Massad M, Fahl M, Slim M, Haddad R, Dagher I, Alam S, Najjar F. Thrombosed Bjork-Shiley standard disc mitral valve prosthesis. J Cardiovasc Surg (Torino). 1989. 30:976–980.
14. Venugopal P, Kaul U, Iyer KS, Rao IM, Balram A, Das B, Sampathkumar A, Mukherjee S, Rajani M, Wasir HS. Fate of thrombectomized Bjork-Shiley valves. A long-term cinefluoroscopic, echocardiographic, and hemodynamic evaluation. J Thorac Cardiovasc Surg. 1986. 91:168–173.
15. Hall JG, Pauli RM, Wilson KM. Maternal and fetal sequelae of anticoagulation during pregnancy. Am J Med. 1980. 68:122–140.

16. Iturbe-Alessio I, Fonseca MC, Mutchinik O, Santos MA, Zajarias A, Salazar E. Risks of anticoagulant therapy in pregnant women with artificial heart valves. N Engl J Med. 1986. 315:1390–1393.

17. Soeda M, Shiono M, Inoue T, Hata M, Sezai A, Negishi N, Sezai Y. A successfully operated case of prosthetic valve thrombosis during planned pregnancy. Ann Thorac Cardiovasc Surg. 2006. 1:66–70.
18. Roudaut R, Lafitte S, Roudaut MF, Courtault C, Perron JM, Jais C, Pillos X, Coste P, DeMaria A. Fibrinolysis of mechanical prosthetic valve thrombosis: a single-center study of 127 cases. J Am Coll Cardiol. 2003. 41:653–658.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download