Abstract
A 7-yr-old boy visited our surgical center with Pfeiffer syndrome type 1, presenting with macrocrania, broad big toe and thumb, exophthalmos, tongue protrusion, malocclusion with midfacial retrusion, mild respiratory difficulty due to minor upper airway obstruction, and developmental delay. He also exhibited anthrophobia with a passive character. The patient was treated with internal monoblock distraction osteogenesis to increase the intracranial and intraorbital volumes, and the nasal and pharyngeal airway spaces using two modular mid-facial internal distractors. For distraction, the latency period was 1 week, the daily activation of 1.0 mm was 20 days (total advancement 20 mm at the midline), and the consolidation period was 3 months. The follow-up computed tomography 12 months after surgery showed expansion of the brain and proper ossification in the distracted area. The patient also showed aesthetically good cranial contours, improved tongue and eyeball protrusion, no respiratory difficulty, and improved learning. We suggest that the internal distraction may last longer than an external type, resulting in a better bone fusion rate and successful expansion of craniofacial bones.
After Ilizarov first reported successful distraction osteogenesis of the long bone, there was a report by McCarthy et al. (1) who were the first to perform a distraction osteogenesis of the human craniofacial mandible bone. Thereafter numerous studies reported on craniofacial bone expansion. In order to successfully perform distraction osteogenesis in a craniofacial bone, both external and internal devices developed. External devices were first described by Polley et al. (2), who managed infant patients with craniofacial distraction by the direct application of helmets, which later gradually progressed to distraction techniques (3). Advantages of the external type device are that the direction of distraction can be determined 3 dimensionally even after surgery, and that it is easy to remove (4). Drawbacks of this method include the difficulty in maintaining the stability of the osteotomized segment, difficulty in applying it to a patient of less than 2 yr of age who has a thin calvarium, difficulty in activating, and the most problematic of all is the inability to maintain this device for a sustained period of time due to the bizarre morphological appearance of the patient (5). The internal device was first utilized as a custom-made distractor since its first introduction in the mid-1990s, which was easier to apply as a modular type (6, 7). Recently, a biodegradable or a device with a bendable plate has been introduced (8). Disadvantages of this device are the difficulty in determining the distraction direction, the inability to change the direction after surgical application, and the necessity of a secondary surgery for removal of the device (5, 9).
To solve the problem of the lack of intracranial and intraorbital space during craniofacial dysostosis, fronto-orbital monoblock advancement with LeFort III osteotomy has been developed to simultaneously expand the frontal skull and mid-face bones. The combination of this technique with distraction osteogenesis further enhances the efficacy of the procedure. In our opinion, the application of either an external or internal device will both afford favorable results when combined with fronto-orbital monoblock advancement with LeFort III osteotomy, and although the internal device method is technically more difficult to employ, it may be applied for a longer period of time, and therefore seems to be advantageous in terms of osteogenesis and bone fusion. In Korea, numerous reports have described the utilization of external devices for management of craniofacial dysostosis to date, but studies on the application of internal devices are not yet available (10). We herein report the first case of a 7-yr-old male patient with Pfeiffer syndrome in whom craniofacial monoblock distraction was successfully performed with an internal device.
A 7-yr-old boy presented to our surgical center with a broad big toe and thumb, bulging skull on the anterior fontanelle, underdevelopment of the frontal bone, exophthalmos, small face, tongue protrusion, malocclusion with midfacial retrusion, mild respiratory difficulty due to minor upper airway obstruction, and developmental delay. Physical examination showed that his head circumference was 55 cm (more than 97th percentile) in spite of the low body weight (10th percentile), and short height (3th percentile). He also demonstrated a low intelligence quotient (Korea Wechsler Preschool Primary Scale of Intelligence) of 70, and anthrophobia with passive characteristics. He was diagnosed as having Pfeiffer Syndrome Type 1 (Fig. 1). We planned monoblock distraction osteogenesis to decrease the intracranial and intraorbital pressures, and to increase the nasal and pharyngeal airway spaces.
Using a bicoronal incision, a standard fronto-orbital osteotomy was performed. After separating the frontal bone flap, a forceful forward protrusion of the frontal lobe was noticed suggesting high intracranial pressure from the craniosynostosis. Thereafter, the orbital bandeau was also separated with a pneumatic saw, and a LeFort III-osteotomy was performed. The osteotomy line ran across the zygomatic arch, from the sphenozygomatic suture along the floor of the orbit, behind the nasolacrimal duct, along the lacrimomaxillary suture to the nasal bone. The nasal septum was separated from the perpendicular plate of the ethmoid bone with a straight osteotome. The pterygoid plates were separated with a chisel placed into the pterygomaxillary fissure. The viscerocranium was mobilized. Downward rotation of the facial skeleton was also possible when using Rowe's forceps for disjunction of the mid-face from the cranial base. The frontal bone flap and orbital bandeau were fixed into a fronto-maxillary monoblock bone flap with three micro-plates, and two modular midfacial distractors were fixed posteriorly to the temporal bone and anteriorly to the malar eminence of the zygomatic arch. Bilateral activation cables were brought through a stab wound posterior to the coronal incision and anterior to the ear. The coronal incision was closed with continuous monofilament sutures subcutaneously, and staples in the skin.
The total operating time was 380 min, and 740 mL of packed red cells was infused. The patient was kept on a mechanical ventilator for 10 hr, decannulated on the next morning after surgery, and stayed 1 day in the intensive care unit. Postoperatively, a distance of approximately 1 cm appeared between the skull flap and the parietal skull resulting in increased intracranial volume, which was almost completely filled by expansion of the brain. We distracted the fronto-maxillary monoblock bone flap 1.0 mm everyday for 20 days beginning 1 week after the operation. The patient was discharged from the hospital on the 15th postoperative day. The distractors were kept for 3 months of the consolidation phase to a final 20 mm displacement.
Follow-up 3-dimensional computed tomogram (CT) scans at 2 and 4 months after surgery showed increased intracranial space and sufficient expansion of the underlying brain with only a small free epidural space, and the patient also showed stable forward advancement of the fronto-orbito-maxillary faciocranial monoblock, resulting in improved bilateral eye and mouth closing and occlusion motions (Fig. 2, 3). We removed the two distraction bars 4 months after the initial establishment of the distraction system. At 12 months after surgery, the follow-up 3-dimensional CT scans showed proper ossification in the distracted area (Fig. 4). The patient showed good cranial contours aesthetically, with upward elevation and forward displacement of the preoperatively depressed fronto-facial contour. His parents were also satisfied with this result. He also showed a slightly increased intellectual quotient of 80, and his character changed from passive to active, resulting in improved learning and rehabilitation exercise without any unexpected postoperative complications.
Surgical management by LeFort III osteotomy for children with craniofacial dysostosis syndrome was first reported by Gillies in 1950, after which this procedure was firmly established as the primary mode of treatment by Tessier (11). Later, Ortiz-Monasterio et al. (12) developed the monoblock advancement with LeFort III osteotomy method whereby the fronto-orbital segment and the midface counterpart are advanced simultaneously. In the 1990s, this technique further advanced to distraction osteogenesis (13, 14). Advantages of distraction osteogenesis are that distraction is less invasive since it is performed without a bone graft and therefore less blood loss occurs, the operative time is shorter, bone union is superior leading to longer bone formation or growth, the induced bone growth shows good bone fusion that is comparable to previous methods in terms of bone thickness and strength, and finally, favorable skin and subcutaneous soft tissue expansion allows repeat surgery (15).
The first operation for treatment of craniofacial dysostosis syndrome is usually necessary within months or within one year of birth, and additional surgery may be required at 2-3 yr of age. The age 5-6 yr, at which adenoid infections most commonly occurs and develop to further narrow the passageway leading to obstructive sleep apnea syndrome, is considered to be the optimum age for timing of the primary surgery of the mid-face (16, 17). Additional craniofacial surgery is performed at 15 yr of age according to the status of the skull and facial bones. As our patient did not receive craniosynostosis surgery during the infancy, the increased intracranial pressure resulted in the horn-like central bony elevation of the anterior fontanelle, and the maxilla was underdeveloped leading to eyeball protrusion, malocclusion, and respiratory difficulty. Therefore, the skull and maxilla were simultaneously expanded with distraction.
In cases where the cranium and midface needs to be advanced simultaneously, it is advantageous to perform the monoblock advancement in which the midfacial segment and the fronto-orbital segment are advanced together, thus reducing the number of procedures to a single procedure. However, there exists a major drawback such as possible severe and fatal infection of the opened nasal cavity and frontal skull base (18). In a recent study, it was suggested that since advancement for distraction osteogenesis is performed after nasal mucosal healing, opening the nasal cavity and frontal skull base would significantly decrease the possibility of a severe infection (19).
Common and difficult problems when applying an internal device is the determination of the direction of the device and the inability to change the direction once it has been applied (5, 9). Exceptional advancement employing an internal device during craniofacial monoblock distraction with LeFort III osteotomy frequently results in the soft tissue tension casing caudal rotation of the midfacial segment, which in turn displaces the zygomaticomaxillary complex more anteriorly than the dentoalveolus (20). Furthermore, lateral advancement forces leads to midline advancement, resulting in possible fractures of the zygomaticomaxillary junction, and worsening of the facial concavity (20). To overcome these problems, authors expect that the zygomaticomaxillary complex balance with internal device distraction will prevent rotation, and also that sufficient bone separation during surgery will markedly decrease any lateral distraction of the zygomaticomaxillary complex.
Despite such inherent limitations of the internal device, there are some craniofacial surgeons who prefer the internal device over the external device. The reason for this is that the external type is cosmetically unfavorable and uncomfortable for long-term application (21, 22). For bone formation induction and consolidation to take place after distraction osteogenesis, the distraction device needs to be in place for at least 1-3 months, which is very difficult with a poor patient's compliance. Hence, a shorter consolidation period ensues and the bone fusion rate decreases, and subsequently there is an increased chance of relapse.
A review of previous reports showed that during the postoperative period, a latency period was applied for 0-7 days, the activation rate was 0.5-1.5 mm/day, and the activation period was 14-30 days (5, 7, 14-16, 22-26). Also, the total distance of advancement has been reported to be 14-30 mm for cranial distraction, and 8-23 mm for facial distraction. The recommended consolidation period ranges from 3 weeks to 6 months (5, 7, 14-16, 19, 23-26). As yet, there have been no definite conclusive statistical data in the literature that suggest which method is superior to the others, but it is generally recommended that activation and follow-up radiological studies such as 3-dimensional CT be conducted to assess bone fusion during the consolidation phase.
Figures and Tables
Fig. 1
Upper: preoperative three-dimensional reconstruction images of computed tomography show bulging skull of the anterior fontanelle (red arrows), underdevelopment of frontal bone (yellow arrows), small face, and malocclusion with midfacial retrusion (white arrows). Lower: preoperative photos show exophthalmos (yellow arrows), malocclusion and tongue protrusion (white arrow) due to midfacial retrusion.
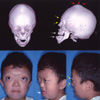
Fig. 2
Upper: postoperative three-dimensional reconstruction images of computed tomography at 2 months after surgery show forward advancement of fronto-facial monoblock (yellow arrows) and improved malocclusion (white arrows) with a distraction rod (blue arrows). Lower: postoperative photos show improved exophthalmos (yellow arrows) and malocclusion, disappearance of tongue protrusion after midfacial advancement with a distraction rod (blue arrows) exposed on the temporal scalp.
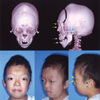
Fig. 3
Conceptual illustration of the preoperative, postoperative and overlapped images of the cranio-facial bony contour in the three-dimensional computed tomography. Left: preoperative image shows small face, malocclusion with midfacial retrusion (blue arrow), and slanted clival angle (blue arrow heads). Middle: postoperative image shows improved malocclusion (yellow arrow) and slanted clival angle (blue arrow heads). Right: the overlapping image based on the clival angle shows forward advancement (white arrows) of cranio-facial monoblock bone flap (red color), compared with preoperative craniofacial contour (blue color).
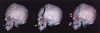
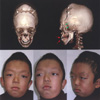
Fig. 4
One year follow-up computed tomography images of three-dimensional reconstruction show bony fusion in the cranial advancement area (white arrows) and in the maxillary bone (green arrows) with improved occlusion of teeth (red arrows). Lower: one-year follow-up photos show nearly normal facial contours.
References
1. McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992. 89:1–8.

2. Polley JW, Figueroa AA, Charbel FT, Berkowitz R, Reisberg D, Cohen M. Monobloc craniomaxillofacial distraction osteogenesis in a newborn with severe craniofacial synostosis: a preliminary report. J Craniofac Surg. 1995. 6:421–423.
3. Polley JW, Figueroa AA. Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg. 1997. 8:181–185.

4. Fearon JA. Halo distraction of the Le Fort III in syndromic craniosynostosis: a long-term assessment. Plast Reconstr Surg. 2005. 115:1524–1536.

5. Riediger D, Poukens JM. Le Fort III osteotomy: a new internal positioned distractor. J Oral Maxillofac Surg. 2003. 61:882–889.

6. Cohen SR, Rutrick RE, Burstein FD. Distraction osteogenesis of the human craniofacial skeleton: initial experience with new distraction system. J Craniofac Surg. 1995. 6:368.
7. Chin M, Toth BA. Le Fort III advancement with gradual distraction using internal devices. Plast Reconstr Surg. 1997. 100:819–830.

8. Cohen SR, Holmes RE. Internal Le Fort III distraction with biodegradable devices. J Craniofac Surg. 2001. 12:264–272.

9. Gosain AK. Plastic Surgery Educational Foundation DATA Committee. Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg. 2001. 107:278–280.

10. Lee YK, Choi JH, Kim SH, Baek SH, Chang YI. Midfacial distraction osteogenesis of Crouzon syndrome with RED (Rigid External Distraction) system. Korean J Orthod. 2002. 32:175–183.
11. Tessier P. The definitive plastic surgical treatment of the severe facial deformities of craniofacial dysostosis: Crouzon's and Apert's diseases. Plast Reconstr Surg. 1971. 48:419–442.

12. Ortiz-Monasterio F, del Campo AF, Carrillo A. Advancements of the orbits and the midface in one piece, combined with frontal repositioning, for the correction of Crouzon's deformities. Plast Reconstr Surg. 1978. 61:507–516.
13. McCarthy JG, Glasberg SB, Cutting CB, Epstein FJ, Grayson BH, Ruff G, Thorne CH, Wisoff J, Zide BM. Twenty-year experience with early surgery for craniosynostosis. II. The craniofacial synostosis syndromes and pansynostosis-Results and unsolved problems. Plast Reconstr Surg. 1995. 96:284–295.
14. Hirabayashi S, Sugawara Y, Sakurai A, Harii K, Park S. Frontoorbital advancement by gradual distraction. Technical note. J Neurosurg. 1998. 89:1058–1061.
15. Uemura T, Hayashi T, Satoh K, Mitsukawa N, Yoshikawa A, Jinnnai T, Hosaka Y. A case of improved obstructive sleep apnea by distraction osteogenesis for midface hypoplasia of an infantile Crouzon's syndrome. J Craniofac Surg. 2001. 12:73–77.

16. Iannetti G, Fadda T, Agrillo A, Poladas G, Iannetti G, Filiaci F. LeFort III advancement with and without osteogenesis distraction. J Craniofac Surg. 2006. 17:536–543.

17. Mitsukawa N, Satoh K, Hayashi T, Furukawa Y, Uemura T, Hosaka Y. A reflectable case of obstructive sleep apnea in an infant with Crouzon syndrome. J Craniofac Surg. 2004. 15:874–878.

18. Fearon JA, Whitaker LA. Complications with facial advancement:a comparison between the Le Fort III and monobloc advancements. Plast Reconstr Surg. 1993. 91:990–995.
19. Kubler AC, Speder B, Zoller JE. Fronto-orbital advancement with simultaneous LeFort III-distraction. J Craniomaxillofac Surg. 2004. 32:291–295.
20. Gosain AK, Santoro TD, Havlik RJ, Cohen SR, Holmes RE. Midface distraction following Le Fort III and monobloc osteotomies: problems and solutions. Plast Reconstr Surg. 2002. 109:1797–1808.

21. Akizuki T, Komuro Y, Ohmori K. Distraction osteogenesis for craniosynostosis. Neurosurg Focus. 2000. 9(3):e1.

22. Chung J, Yoon SH. Rotating distraction osteogenesis in a child with secondary craniosyntostosis. J Craniofac Surg. 2006. 17:557–560.

23. Anderson PJ, Tan E, David DJ. Simultaneous multiple vector distraction for craniosynostosis syndromes. Br J Plast Surg. 2005. 58:626–631.

24. Holmes AD, Wright GW, Meara JG, Heggie AA, Probert TC. LeFort III internal distraction in syndromic craniosynostosis. J Craniofac Surg. 2002. 13:262–272.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download