Abstract
Recurrence after thoracoscopic surgery for primary spontaneous pneumothorax is a lingering problem, and many intraoperative methods to induce pleural symphysis have been introduced. We analyzed the effects of chemical pleurodesis during thoracoscopic procedures. Between August 2003 and July 2005, 141 patients among indicated surgical treatment for primary spontaneous pneumothorax in two hospitals of our institution allowed this prospective study. The patients were randomly assigned to 3 groups: thoracoscopic procedure only (group A, n=50), thoracoscopic procedure and pleurodesis with dextrose solution (group B, n=49), and thoracoscopic procedure and pleurodesis with talc-dextrose mixed solution (group C, n=42). There was no significant difference in demographic data among the three groups. The two groups that underwent intraoperative pleurodesis had significantly longer postoperative hospital stays (A/B/C: 2.50±1.85/4.49±2.10/6.00±2.58 days; p=0.001) and a higher incidence of postoperative fever (A/B/C: 10.0/22.45/52.38%; χ2=21.598, p=0.00). No significant differences were found for recurrence rates or the number of postoperative days until chest tube removal. Therefore, the results of our study indicate that intraoperative chemical pleurodesis gives no additional advantage to surgery alone in deterring recurrence for patients with primary spontaneous pneumothorax. Thus, the use of such scarifying agents in the operating room must be reconsidered.
Treatment options for primary spontaneous pneumothorax range from simple observation to surgery (1-3). Despite all efforts, recurrence has always been a lingering problem, and many intraoperative methods to induce pleural symphysis have been introduced, including mechanical pleural abrasion, ablation with Nd:YAG laser, partial pleurectomy, and instillation of chemical irritants (4). Nowadays, many surgeons perform the bleb resection with mechanical abrasion or pleurectomy. Although these procedures report good long-term results, there were several disadvantages (5).
In this study, we analyzed the effects of chemical pleurodesis after bleb resection, bullectomy or electrocoagulation for recurrences in primary spontaneous pneumothorax as a simple alternative method of pleurectomy or pleural adhesion. We prospectively conducted adjuvant pleurodesis with a 20% dextrose solution or talc -20% dextrose mixed solution during thoracoscopic procedures in patients with primary spontaneous pneumothorax. The effects were evaluated by comparing outcomes of the patients who underwent thoracoscopic procedures alone with those who underwent additional chemical pleurodesis.
We designed the multicenter, prospective, randomized trial under the approval of our center's Institutional Review Board. The allocation of the patients was conducted by the fixed date. Informed consent was obtained from each patient after thorough explanation.
Between August 2003 and July 2005, 141 patients indicated for surgical treatment of primary spontaneous pneumothorax in two hospitals of our institute were included in this study. A total of 141 patients, 134 males and 7 females, ranging in age from 13 to 65 yr old (average 23.16) were treated by video assisted thoracoscopic surgery using a 10 mm or 2 mm scope for primary spontaneous pneumothorax. The 10-mm thoracoscopic surgeries were inclined to the early stage of this study. Primary spontaneous pneumothorax was defined as a spontaneous pneumothorax in a patient without any identifiable underlying lung disease, trauma, or iatrogenic injury. All patients were positively identified to have pleural/subpleural blebs by thoracoscopic examination (with a 2-mm thoracoscope) (6) or by high-resolution computed tomography. In this prospective study, the patients were randomly assigned to 3 different groups by two surgeons: thoracoscopic bleb resection or electrical coagulation (TBR) only (50 patients; group A), TBR and pleurodesis with a 20% dextrose solution (200 cc) (49 patients; group B), and TBR and pleurodesis with a talc (2 g of asbestos free sterilized talc powder) -20% dextrose mixed solution (200 cc) (42 patients; group C).
In the early stage of this study, 31 operations were performed with a 10-mm thoracoscope, but all remaining 110 consecutive operations were performed by needlescopy (2-mm thoracoscopy) (7). According to their assigned groups, the patients received adjuvant pleurodesis after resection of blebs with mechanical suturing devices. The chemicals were instilled into the pleural cavity, mainly at the thoracoscopic procedure sites and apex of the lungs. In group C, talc powder was mixed with the dextrose solution to form a slurry before instillation. The solutions were allowed to drain freely after the patient was transferred to the general ward (average time of pleurodesis, 2 hr). No form of mechanical pleural abrasion was conducted in any of the patients. Postoperative pain was managed by oral nonsteroidal anti-inflammatory drugs (NSAIDs) and intermittent parenteral NSAIDs and meperidine for break-through pain. Patients were discharged 2 days after chest tube removal according to our institutional protocol.
Postoperative data was recorded included recurrence of pneumothorax, postoperative hospital stay, days until chest tube removal, occurrence of postoperative fever, and frequency of parenteral analgesics use. Patients follow-up was conducted by outpatient clinic visits and telephone interviews. Statistical analysis was done using SPSS for Windows (Ver. 10.0.7., Chicago, IL, U.S.A.). Analysis of variance (ANOVA) was used to compare patient characteristics, postoperative hospital stay, days until chest tube removal, and chest tube drainage amount. Chi-square test was used to compare categorical variables. All p values <0.05 were considered statistically significant.
Patient characteristics are summarized in Table 1. The mean ages of patients were 22.26 yr for group A, 24.18 for group B, and 23.02 for group C. There were 46 males and 4 females in group A, 46 males and 3 females in group B, and 42 males and no females in group C. The three groups did not differ significantly in age, sex, or surgical approach. There were no operative deaths, and all procedures were uneventful. No patient underwent conversion to open thoracotomy.
Postoperative data are summarized in Table 2. Days until chest tube removal were 2.96±1.56 days for group A, 2.95 ±2.31 for group B, and 3.60±1.65 for group C (p=0.188) and did not differ significantly. Postoperative hospital stay and frequency of parenteral analgesics use per patient differed significantly among the 3 groups. The durations of postoperative hospital stay (days) were 2.50±1.85 in group A, 4.49 ±2.10 in group B, and 6.00±2.58 in group C (p=0.001), and frequencies of parenteral analgesics use per patient were 2.37±3.51 for group A, 3.42±3.48 for group B, and 5.02 ±2.72 for group C (p=0.001). Post hoc studies (Duncan) showed that group C differed significantly from group A and B in postoperative stay and parenteral analgesics use. Five patients in group A, 11 in group B, and 22 in group C experienced postoperative fever ( χ2=21.598, p=0.00), showing a significant difference.
Mean follow-up durations were 20.22±9.71 months in group A, 23.65±2.51 months in group B, and 17.93± 3.64 months in group C. During follow-up, recurrent ipsilateral pneumothorax was noted in 5 of the 141 patients (3.54 %); 3 in group A (6.0%), 1 in group B (2.04%), and 1 in group C (2.38%). There was no statistically significant difference in recurrence rates among the three groups ( χ2=1.372, p=0.54). Of the 5 patients with ipsilateral recurrence, 2 underwent reoperation by video-assisted thoracoscopic surgery (VATS), 2 were treated by chest tube drainage, and 1 patient received conservative management with inhaled oxygen.
VATS is currently well accepted as a safe and effective procedure for the management of primary spontaneous pneumothorax. After resection or ligation of blebs and elctrocaogulation of subpleural blebs many adjuvant procedures have been used to achieve pleural symphysis in order to further reduce recurrence rates. Partial pleurectomy and pleural abrasion have shown recurrence rates of 2-4.4% (8, 9) and 3-3.6% (10, 11), respectively. Chemical pleurodesis has also been tried with talc, and minocycline and have shown recurrence rates of 1.73-5% (12, 13) and 2.9% (14), respectively. Other reported methods include electrocoagulation of the pleura and ablation with Nd:YAG laser.
At our institution, VATS is conducted for pneumothorax with a 2-mm thoracoscope and instruments from 2003. Surgical staplers are introduced via the 11.5 mm trocar site at the thoracostomy wound, which most of the patients already have before the operation. Although a recent study by Chang (15) showed a higher rate of recurrence by needlescopic VATS (procedure using instruments with an external diameter ≤3 mm [7]) compared to the same procedures performed by conventional VATS, our experience shows that recurrence rates are comparable to conventional VATS (16-19). We hypothesized that additional chemical pleurodesis may further decrease recurrence rates after bleb resection.
The selection of the agents for chemical pleurodesis was based on their low cost, ease of administration, and reported high effectiveness (20-22). Our results show that 20% dextrose solution and talc are effective in reducing recurrence rates, showing comparable recurrence rates with those of previous studies with other agents in the literature. However, there is still much concerns in regards to acute and chronic side effects of talc. During this study, we did not experience any cases of postoperative empyema, arrhythmia, or respiratory failure, all of which have been reported in the literature (23). Although chemical pleurodesis did not increase the duration of postoperative chest drainage, a significantly greater number of patients with fever was noted and due to more frequent chest pain more parenteral analgesics was used in the pleurodesis groups, especially the talc group. There is also the issue of possible oncogenic risk and difficulty in performing future thoracoscopy or thoracotomy caused by the creation of tight adhesions (11).
Our results showed that VATS procedures for primary spontaneous pneumothorax are safe and effective. However, we feel that practice of additional chemical pleurodesis for deterring recurrence should be reconsidered. Chest pain and fever associated with this procedure may cause unnecessary suffering for the patients and extension of postoperative hospital stay.
Figures and Tables
Table 1
Patient characteristics
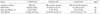
N, number of patients; Signif, statistical significance; NS, not significant.
TBR Only, thoracoscopic procedures without chemical pleurodesis; TBR with 20% dextrose, thoracoscopic procedures and chemical pleurodesis with a 20% dextrose solution; TBR with talc-20% dextrose, thoracoscopic procedures and chemical pleurodesis with a talc-20% dextrose solution.
References
1. Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001. 119:590–602.
2. Cardillo G, Facciolo F, Giunti R, Gasparri R, Lopergolo M, Orsetti R, Martelli M. Videothoracoscopic treatment of primary spontaneous pneumothorax: a 6-year experience. Ann Thorac Surg. 2000. 69:357–361. discussion 61-2.

3. Henry M, Arnold T, Harvey J. BTS guidelines for the management of spontaneous pneumothorax. Thorax. 2003. 58:Suppl 2. ii39–ii52.

5. Chan P, Clarke P, Daniel FJ, Knight SR, Seevanayagam S. Efficacy study of video-assisted thoracoscopic surgery pleurodesis for spontaneous pneumothorax. Ann Thorac Surg. 2001. 71:452–454.

6. Lee SA, Kim KT, Park SM, Jung BG, Sun K, Kim HM, Lee IS. 2 mm video thoracoscopic examination for primary spontaneous peumothorax. Korean J Thorac Cardiovasc Surg. 2000. 33:306–309.
7. Mamazza J, Schlachta CM, Seshadri PA, Cadeddu MO, Poulin EC. Needlescopic surgery. A logical evolution from conventional laparoscopic surgery. Surg Endosc. 2001. 15:1208–1212.
8. Ayed AK. Suction versus water seal after thoracoscopy for primary spontaneous pneumothorax: prospective randomized study. Ann Thorac Surg. 2003. 75:1593–1596.

9. Cardillo G, Facciolo F, Regal M, Carbone L, Corzani F, Ricci A, Martelli M. Recurrences following videothoracoscopic treatment of primary spontaneous pneumothorax: the role of redo-videothoracoscopy. Eur J Cardiothorac Surg. 2001. 19:396–399.

10. Lang-Lazdunski L, Chapuis O, Bonnet PM, Pons F, Jancovici R. Videothoracoscopic bleb excision and pleural abrasion for the treatment of primary spontaneous pneumothorax: long-term results. Ann Thorac Surg. 2003. 75:960–965.

11. Gossot D, Galetta D, Stern JB, Debrosse D, Caliandro R, Girard P, Grunenwald D. Results of thoracoscopic pleural abrasion for primary spontaneous pneumothorax. Surg Endosc. 2004. 18:466–471.
12. Cardillo G, Carleo F, Giunti R, Carbone L, Mariotta S, Salvadori L, Petrella L, Martelli M. Videothoracoscopic talc poudrage in primary spontaneous pneumothorax: a single-institution experience in 861 cases. J Thorac Cardiovasc Surg. 2006. 131:322–328.

13. Tschopp JM, Brutsche M, Frey JG. Treatment of complicated spontaneous pneumothorax by simple talc pleurodesis under thoracoscopy and local anaesthesia. Thorax. 1997. 52:329–332.

14. Chen JS, Hsu HH, Kuo SW, Tsai PR, Chen RJ, Lee JM, Lee YC. Effects of additional minocycline pleurodesis after thoracoscopic procedures for primary spontaneous pneumothorax. Chest. 2004. 125:50–55.

15. Chang YC, Chen CW, Huang SH, Chen JS. Modified needlescopic video-assisted thoracic surgery for primary spontaneous pneumothorax: the long-term effects of apical pleurectomy versus pleural abrasion. Surg Endosc. 2006. 20:757–762.
16. Hatz RA, Kaps MF, Meimarakis G, Loehe F, Muller C, Furst H. Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg. 2000. 70:253–257.

17. Inderbitzi RG, Leiser A, Furrer M, Althaus U. Three years' experience in video-assisted thoracic surgery (VATS) for spontaneous pneumothorax. J Thorac Cardiovasc Surg. 1994. 107:1410–1415.
18. Loubani M, Lynch V. Video assisted thoracoscopic bullectomy and acromycin pleurodesis: an effective treatment for spontaneous pneumothorax. Respir Med. 2000. 94:888–890.

19. Waterworth PD, Kallis P, Townsend ER, Fountain SW. Thoracoscopic bullectomy and tetracycline pleurodesis for the treatment of spontaneous pneumothorax. Respir Med. 1995. 89:563–566.

21. Peng ZM, Wu ES. Clinical value of hypertonic glucose injection in the treatment of recurrent pneumothorax. Hunan Yi Ke Da Xue Xue Bao. 2002. 27:256–258.
22. Frick T, Buchmann P, Largiader F. Experience with thoracoscopic pleurodesis in the treatment of idiopathic spontaneous pneumothorax. Helv Chir Acta. 1990. 57:395–398.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download