Abstract
An economic evaluation of Haemophilus influenzae type b (Hib) immunization was conducted to examine whether Hib immunization should be included in the Korea's national immunization program. The costs and benefits included direct and indirect values and an estimation of the economic efficiency. We determined that a universal Hib immunization program in Korea would prevent 17 deaths and 280 invasive Hib cases. When we assumed the one Hib immunization cost as 26,000 won, the national Hib immunization would cost 34.6 billion won. Costs for various Hib diseases were estimated at 26.8 billion won (11.8 billion won from direct costs and 14.9 billion won from indirect costs). A benefit-cost ratio of 0.77 showed that the economic efficiency of the integration of Hib immunization in Korea is low because of the low incidence rate of Hib disease and high price of vaccine. However, if the Hib immunization cost decrease to less than 20,000 won, a benefit-cost ratio increase to 1.0 and above, integrating Hib immunization into the national immunization program with economic efficiency can be considered.
Haemophilus influenzae type b (Hib) is an important cause of meningitis, pneumonia, and other invasive infections in infants (1-3). Hib meningitis, specifically, may result in serious neurological sequelae. Invasive diseases caused by Hib can now be prevented by immunization with polysaccharide-protein conjugate vaccines that were developed in the 1980s and are proven safe, immunogenic, and highly effective when given to infants (3). Until now, the Hib vaccines have not been added to the routine immunization schedules of developing countries because of the high cost of the vaccine and low economic efficiency (4). Among 37 Western Pacific region countries, only 16 countries have introduced the Hib vaccine into their routine childhood immunization program in 2005 (5). Mongolia introduced and supported the conjugate Hib vaccine with the support of the Global Alliance for Vaccines and Immunization (GAVI) in 2005. Indonesia included Hib vaccine into their national immunization program after the research on cost-benefit analysis of Hib immunization (6).
In Korea, the conjugate Hib vaccine was introduced in 1993 but has not yet been integrated into the national immunization program. The cost of Hib immunization is not supported by the Korean government, because it is not included in the national immunization program, meaning that the total cost of Hib immunization has to be paid by parents. The total direct cost of Hib immunization for a full series of 3 doses is 120,000 won, imposing a heavy burden on parents. Despite this fact, the Hib immunization rate has risen from 16% in 2002 (7) to 50% in 2005 (8).
Since 1998, the World Health Organization (WHO) has recommended that the Hib conjugate vaccine be included in national immunization schedule in all countries where resources permit its use and the burden of disease has been established (1, 3).
To examine whether Hib immunization should be included in a universal immunization program in Korea, an economic evaluation of Hib immunization was conducted with societal perspective. All future costs associated with long-term health effect from Hib disease were considered.
The epidemiological data on Hib for Korea were obtained from the results of a previously published paper. Results from other Asian countries and Western countries were also used in our analysis. A decision tree of the cost-benefit analysis is presented in Fig. 1.
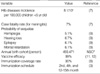
The economic effect of the Hib immunization program on a birth cohort of 493,471 infants, the estimated number of births in 2003, was evaluated from birth through to 5 yr of age. The most important epidemiologic data used in this cost-benefit analysis were based on the results of Kim and his colleagues' survey in 2004 (7). This was the first population-based study and the only report of annual incidence of Hib meningitis in Korea; it was conducted between 1999 and 2001 in Jeonbuk province. The annual incidence of Hib disease was estimated at 6.8 per 100,000 in children under the age of 5. This study assumed that 16% (7) of children on the study population were completely immunized with the Hib vaccine. Therefore, they estimated the Hib incidence based on an adjusted population denominator that did not include children with the Hib vaccination since they would not be at risk for the Hib disease. We used the adjusted annual incidence of Hib invasive disease in the analysis, which was 8.1 per 100,000 in children under 5 yr of age (7). Among Hib invasive disease, 87% showed meningitis (the incidence of Hib meningitis was 7.1 per 100,000), and 13% caused other invasive disease including pneumonia, epiglottitis, and other manifestations (7). We could not find data on the incidence rates of Hib pneumonia and other Hib invasive diseases except Hib meningitis in Korea, so we assumed the same ratios for pneumonia over meningitis as those gathered from the United States (9) because the US data were very comprehensive than the other countries data. The case fatality rate of Hib meningitis was 7% (7). Hib meningitis is a dangerous disease associated with a high rate of neurological sequelae; possible long-term consequences for children with meningitis included in our model were mental retardation, severe hearing loss, epilepsy, and hemiplegia. The probabilities of these outcomes were 6.1%, 6.7%, 6.1%, and 5.1%, respectively (9, 10). Current Hib vaccine is highly effective (3). Therefore, in this study, we assumed Hib vaccine efficacy after completing the immunization schedule set at 99% (11, 12) and 100% compliance for cost-benefit analysis. The epidemiological data used in the economic evaluation are listed in Table 1.
Costs were expressed in Korean won (1 USD=1,200 won [exchange rate in 2003]). All costs were inflated to the value of the Korean won in 2003, and discounted at a 5% annual rate for the base case analysis by Center for Disease Control and Prevention (CDC)'s recommendation (13).
An economic evaluation was conducted to evaluate the introduction of a prevention program by universal immunization against Hib in infants less than 1 yr of age in Korea.
A sensitivity analysis was also performed to evaluate the robustness of the conclusion to changes in the assumptions about the main determinants of costs and benefits to preventing the Hib invasive disease. We changed price of Hib vaccination, discount rate, and the incidence of Hib disease. For the discount rate, we used a 3% discounted rate, according to Korean pharmacoeconomics guidelines (K-PEG) developed by the Health Insurance Review and Assessment service (HIRA) in 2005.
Given the limited information on Hib disease incidence in Korea, to evaluate the extent to which underestimation of Hib incidence rate in the pre-immunization era could potentially have an impact in our analysis, a 95% confidence interval (4.1/100,000-16.1/100,000) of the 8.1/100,000 incidence rate was used in our model (7).
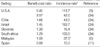
In this study, direct costs included those associated with the medical cost of Hib diseases, additional costs due to sequelae of Hib meningitis and transportation. Indirect costs included the economic value of the lives of children and parents due to Hib diseases and sequelae. The benefit of the immunization program is conceptualized as those costs that would be avoided with Hib immunization. Benefit included not only the averted medical costs associated with acute Hib disease and sequale, but also the reduced economic productivity that results from a disability or premature death. Table 2 shows the value of economic parameters used for cost-benefit analysis.
The National Health Insurance (NHI) program in Korea covers the whole population as a compulsory social system; the total number of people covered by the NHI reached over 47 million or about 96.6% of the total population. Medical costs including inpatient and outpatient cases of Hib meningitis, Hib pneumonia, and other Hib diseases were calculated using the HIRA claim data from 2003. Because these data included only insurance covered costs, we also include non-reimbursed costs (14) in the medical calculation (non-reimbursed costs in total health care expenditure was 15.4% for inpatient and 30.1% for outpatient) (14). The average medical costs were estimated to be 3,040,399 won for meningitis, 1,228,269 won for pneumonia, and 1,284,995 won for all other types of Hib invasive diseases including epiglottitis, bacteremia, and cellulitis.
Hib meningitis can cause neurological disabilities such as mental retardation, hearing loss, and epilepsy, and we included the cost of associated rehabilitation services in this study. Concretely, it was assumed that the annual costs for hemiplegia, which accounted for 5.1% of Hib meningitis cases, were 3,600,000 won based on National Rehabilitation Center (NRC) data, and that the average lifespan is 50 yr for these individuals (9). For children with hearing impairments, the cost of a hearing-aid was included. The cost of a standard hearing-aid used was the benefit paid by the Ministry of Health and Welfare (MOHW) health security program, which was paid at 250,000 won. This study assumed that the patient would need a hearing-aid for 50 yr of life and it would have to be replaced every 5 yr. For long-term epilepsy care, the annual treatment cost was 1,343,000 won based on HIRA data, and it was calculated for 50 yr. The average monthly special education cost for mentally handicapped children until 19 yr old was 700,000 won based on data from the Research Institute for Differently Abled Person's Right in Korea (RIDRIK). We assumed that this kind of special education would be needed for 15 yr, from age 5 to 19. The cost associated with rehabilitation for sequelae was inflated at 3.6%, discounted at a 5% annual rate and was expressed at the 2003 rate for the won. Other direct costs for treatment include the caregiver's travel cost to clinics during the treatment period (a round- trip in Seoul). We calculated the average cost of transportation using 2001 Korea Health and Nutrition Examination Survey (KNHANES) data, and then we converted it to the 2003 won rate, applying the Consumer Price Index (CPI) for transportation.
Our model estimated the economic value of life lost prematurely, indirect costs from permanent disability, and indirect costs associated with parents who missed work and stayed at home to care for sick children. Although difficulty to estimate, the economic value of life was estimated using the human capital approach that assumes that the monetary value of lost productivity equals the wage rate (15).
The indirect costs associated with parents' absence from work to take care of their sick children with Hib were included in the analysis. The economic costs for parents taking time off work were estimated on the basis of individual inpatient and outpatient days and an average daily wage of 101,895 won in 2003. The average wage data were taken from the Survey Report on Wage Structure of the Ministry of Labor (16). The average treatment periods of Hib invasive disease inpatients and outpatients, respectively, were 23.6 days and 14.6 days for meningitis, 16 days and 3.1 days for pneumonia, and 13.7 days and 2.2 days for other Hib diseases. The period of treatment was based HIRA claim data. Additionally, costs incurred by parents whose child had Hib meningitis sequelae were calculated as follows: it was assumed that full-time care would have to be provided by a parent at an average annual earning of 24.4 million won (16) for 37 yr from the age of 30 (17) - average age of parent at the birth of their first child - up to the age of 67, with a 10% increase every 5 yr. This information was used to calculate the future earning of an individual. The average age of retirement was assumed to be 67 yr of age in Korea based on the 2003 Organization for Economic Cooperation and Development (OECD) report.
For cases where the child has sequelae, the loss of income under the assumption from the age of 20 (the average age of people when they get their first job), up to the age of 67 was estimated. To adjust the severity of disability due to Hib, the Health Utility Index (HUI) (18) was applied to the calculation: 0.840 for hemiplgia, epilepsy, and mental retardation and 0.977 for severe hearing loss (19). The HUI is a value assigned to the quality of life, calculating a weighted coefficient for each health state and adopted in relation to the age of patient. The cost related to a loss of productivity resulting from premature death was also estimated for 47 yr. Since not everyone will be employed, the economically active population rate of 74.7% (20) from the National Statistical Office (NSO) was weighted in the calculation of productivity loss (Table 2).
Hib immunization could be safely administrated with other vaccines such as vaccine for diphtheria, tetanus and pertussis (DTP), and polio immunizations, so the establishment of a Hib immunization program would share infrastructure and organizational costs with the existing immunization program. Therefore, the marginal cost for extending the existing program for DTP and polio immunizations was estimated as an indirect costs of the immunization (6, 9, 11, 21, 22). That is to say, there would be no added cost for an extra visit to the clinic for the Hib vaccine injection.
There are many different combination vaccines that contain the Hib conjugate vaccine; Hib combined with DTP, hepatitis B, and polio. However, combination vaccines were not considered in this study because of the price of vaccine, the schedule and number of immunization, and the efficacy of combination vaccines vary by vaccine.
The number of immunizations needed with the Hib conjugate vaccine is 3 to 4 as stated by the manufacturer. We assumed 3 shots for the Hib immunization in this study.
The following items were considered in estimating the cost of the immunization program: costs for immunization and treatment of adverse reactions produced by the vaccine for direct costs; and the indirect costs included missed work on the part of the parent in the case of an adverse reaction.
Hib vaccine is more expensive than the traditional expanded program on immunization (EPI) vaccine, and prices are changing and differ among countries (3). Hib vaccines are only administered by private clinics in Korea. The price of the Hib immunization is 40,000 won which includes the vaccine and administrative cost; the vaccine cost is around 27,000-30,000 won (whole-sale price) and the administrative and other cost is around 10,000 won in 2003. However, if Hib immunization is adopted as one of the routine immunization and administrated in public clinics, the price would decrease. Hib immunization schedule is same as DTP immunization schedule; they can get Hib and DTP together at one visit which can decrease the administrative cost. When the vaccine purchased by public health sector, the cost of vaccine also can be decreased. It was assumed that there would be a 50% reduction of administrative costs and 20% reduction of the cost of the vaccine. Therefore, we estimated 26,000 won per dose with a 35% reduction of the current price in 2003 for a universal immunization program in the base analysis. The coverage rate of universal immunization was assumed at 90% in this study.
Conjugate Hib vaccines have been found to be generally well-tolerated. They are probably the least reactogenic vaccines in current use, since data from vaccine trials and several large post-marketing surveillance studies have indicated that serious reactions attributable to Hib vaccines are rare (23, 24). Therefore, no medication costs or indirect costs of a patient's time due to adverse vaccine reactions were assumed.
In the base analysis, the universal immunization program would prevent 280 cases of invasive disease, 17 deaths, and 59 sequelae from Hib meningitis. The cost per death averted would be 2 billion won, 123 million won per Hib case averted, and 587 million won per case of Hib meningitis sequelae averted (Table 3).
When we assumed the cost for one shot of Hib immunization as 26,000 won, the immunization program would result in a cost of about 34.6 billion won. The cost for Hib disease, which is regarded as benefits by Hib immunization, was estimated 23.8 billion won (11.8 billion won from direct benefit and 12.0 billion won from indirect benefit). Therefore, a net cost was 7.9 billion won (34,641,664,000 won-26,708,274,000 won=7,933,390,000 won) and a benefit-cost ratio was 0.77 (26,708,274/34,641,664=0.77). This means that the benefits incurred by Hib immunization would be less than its costs. It was shown that integrating the Hib immunization into our national immunization program with the present price of vaccine and incidence of Hib disease has a low economic efficiency (Table 3).
The sensitivity analysis showed that the results are closely related to the incidence of Hib; the benefit-cost ratio was less than 1 (0.39) in the low limit of incidence rate, and the benefit-cost ratio was higher than 1 (1.53) in the case of a high limit of incidence rate (Table 4). In the reference incidence of Hib disease, we found the maximum price that would make it cost-beneficial was 20,000 won. The benefit-cost ratios of Hib immunization varied from 0.25 to 1.99 using a 5% discounted rate and from 0.31 to 2.46 using a 3% discounted rate.
Even though WHO has recommended that the Hib conjugate vaccine be included in national immunization schedules in all countries, the MOHW of Korea did not include Hib immunization as a national routine immunization program, because there were no data on cost-benefit analysis and the cost of immunization is very expensive. All Hib vaccines used in Korea are imported and the cost of the Hib vaccine in 2003 was more than 7,136,989 USD for one year (25), and the voluntary coverage rate of Hib immunization reached 50% (8). Thus, Korea's vaccine policy for Hib should be reconsidered and a reasonable guideline should be prepared by the Korean government.
The results of the economic evaluation of Hib immunization in this study showed Hib immunization would be beneficial with a cost less than 20,000 won for one shot of immunization. However, the price in 2003 (26,000 won for one shot) showed a low economic efficiency. The relatively a lower economic efficiency of Hib immunization in Korea resulted mainly from the low incidence rate. Most economic evaluations of Hib immunization showed that the results were very sensitive to the incidence of Hib disease (6, 11, 21, 22). This result differs from those of most other countries (Table 5). Most economic evaluations of Hib immunization have shown that the benefit exceeds the cost of Hib immunization, except in Spain (11).
Some aspects must be considered in the interpretation of these results. The incidence rate used in this study, which was firstly reported and unique in Korea, was the lowest among the countries studied. Additionally, incidence rates of Hib pneumonia and other Hib diseases have not yet been reported, and we had to assume them using Hib epidemiology data from the United States. The US data was more comprehensive and detail than data from other countries; however, the epidemiological condition could be different from that in Korea. Although we used an adjusted incidence rate, there is a possibility that the incidence was underestimated due to the introduction of the Hib vaccine in private sectors. Incidence rates in this study were lower than those reported in the US, Northern Europe, and Australia in the pre Hib conjugate vaccine era (26), but are comparable to rates observed elsewhere in Asia. The low incidence rate of Hib diseases as found in Korea were also observed in other Asian countries, such as China (27-29) and Japan (30, 31). The variation in Hib diseases incidence rates in different countries and in regions of the same country may be due to the substantial heterogeneity in healthcare systems, completeness of surveillance, methods for clinical evaluation, treatment practices, and socioeconomic determinants. At any rate, it seems true that Hib meningitis rates in Asia are much lower than those in the Western countries such as US and Europe. As for the possible reasons for the low rate of Hib disease among Asian children, inadequate case ascertainment and poor microbiology have been suggested (32). Other invasive diseases caused by Hib, in addition to bacterial meningitis, include bacterial pneumonia, cellulites, septic arthritis, and epiglottis. It was difficult to find the incidence rate of these syndromes in Asian countries (5). Additional studies examining the incidence rate of Hib disease and why some Asian countries show a lower incidence rate of Hib are needed.
Another reason for the lower benefit-cost ratio result was due to the high price of Hib immunization. In Korea, the Hib vaccine is administered in private clinics, so it was difficult to accurately account for the cost of Hib immunization. Consequently, the immunization costs in this study were based on the price of Hib immunization in the private sector in 2003. If the Hib vaccine is adopted as part of a routine immunization, the cost for both the vaccine and its administration would decrease. We assumed 65% of the current price for Hib immunization in 2003; a 20% reduction of vaccine cost and 50% reduction of administration cost. The Hib vaccine could be purchased for around USD 20.00 in Korea, and it is still higher than other countries' immunization costs. However, if the Hib immunization was adopted in a national immunization schedule, the cost of the vaccine would probably be lower due to the economy of scale. If the cost of immunization per dose could be decreased from 40,000 won to 20,000 won with the integration of Hib immunization into the universal immunization program in Korea, we could expect the economic efficiency to increase significantly. Korea experienced a reduction in cost of the varicella vaccination after it was included in the national immunization schedule in 2005; the cost decreased by 57% in private clinics (from 35,000 won to 20,000 won) and the cost of immunization in public health institutions was 10,000 won in 2005. Therefore, the Hib vaccine cost per dose also is expected to decrease significantly - more than assessed in this analysis. If the Hib vaccination cost is under 20,000 won, the result will mean economic efficiency. Hib immunization coverage rates have risen from 16% in 2002 to 50% in 2005. The vaccine volunteer coverage rate is high in proportion to the low incidence because pediatricians in private clinics encourage Hib vaccination. Even though public health center provide national immunization program free of charge, half of all vaccinations in Korea are administered in private clinics. The reasons for the high coverage rate in private clinics are due to the accessibility and mistrusts for public health institutions.
The costs of morbidity and mortality of meningitis are lower than in other countries due to the NHI program. The government strongly regulates the charge of medical treatment offered through NHI, so the medical and rehabilitation costs are quite low; even the medical charge is lower than prime cost in some cases. The cost in Korea is presumed to be much lower than it that in the US: the medical cost of Hib meningitis per patient was 2,533 USD in Korea compared to 9,756 (9) in the US.
The HIRA data used in this analysis do not include data of non-reimbursed cost of insurance and the other costs such as dietary supplements and over-the-counter pharmacy medicines paid by patients. The validity of data is also debatable. Despite these limitations, the NHI program that covered the whole population as a compulsory social system is the most representative data to calculate the medical cost.
In this study, we used human capital approach to estimate productivity loss. However, it is quite controversial that human capital approach could overestimate productivity loss. In this context, the friction cost method that have been made for Netherlands was proposed, and it give estimates of lost production much lower than those obtained from traditional methods, such as the human capital approach (15). Also, Goeree et al. (33) compared the human capital and friction cost approaches in estimating the productivity costs due to premature mortality from schizophrenia in Canada; the estimates using the human capital approach were 69 times higher those obtained using the friction cost approach. According to these results, the productivity loss using the human capital approach could be higher than when using the friction cost approach, and then the results of this cost-benefit analysis would change to less cost beneficial; the benefit-cost ratio would decrease to about 0.51. Despite this limitation, this analysis in Korea is comparable with the Hib vaccination cost-benefit analysis using the human capital approach in other countries (34), and it was used almost the same methodology and assumption.
Hib disease is very serious and the Hib vaccine efficacy was reported to be 99% (12). The most effective method to decrease the Hib disease burden is Hib immunization. To decrease Hib disease burden with increased vaccination coverage, Hib immunization should be integrated into the national immunization program. The Hib vaccine price, however, is too high to get more benefit than the cost. If the Hib immunization cost decrease to less than 20,000 won, a benefit-cost ratio increase to 1.0 and above, integrating Hib immunization into the national immunization program with economic efficiency can be considered.
Figures and Tables
Table 1
Summary of the variables used to estimate the outcomes of Haemophilus influenzae type b (Hib) immunization in Korea
References
1. WHO. Global Programme for Vaccines and Immunizations (GPV). The WHO position paper on Haemophilus influenzae type b conjugate vaccines. Wkly Epidemiol Rec. 1998. 73:64–68.
2. Schillinger J, Schwartz B, Perkins B, Wenger J. Murray CJL, Lopez A, editors. Global burden of bacterial meningitis. The global burden of diseases. 1996. Boston: Harvard School of Public Health (on behalf of the World Health Organization and the World Bank).
3. WHO. Introduction of Haemophilus influenzae type b vaccine into immunization programmes: Department of Vaccines and Biologicals. 2000. WHO.
4. Levine OS, Schwartz B, Pierce N, Kane M. Development, evaluation and implementation of Haemophilus influenzae type b vaccines for young children in developing countries: current status and priority actions. Pediatr Infect Dis J. 1998. 17:9 Suppl. S95–S113.

5. Immunization. cited 2007. May 20. WHO Regional Office for the Western Pacific;Available from:URL: http://www.wpro.who.int/health_topics/immunization/general_info.htm.
6. Hussain I, Syed A, Sofiah A, Ong L, Choo K, Musa M, Teh K, Ng H. Cost-Benefit analysis of Haemophilus influenzae vaccination programme in Malaysia. Buletin Kasiharan Masyakat Jilid. 1999. 5:79–89.
7. Kim JS, Jang YT, Kim JD, Park TH, Park JM, Kilgore PE, Kennedy WA, Park E, Nyambat B, Kim DR, Hwang PH, Kim SJ, Eun SH, Lee HS, Cho JH, Kim YS, Chang SJ, Huang HF, Clemens JD, Ward JI. Incidence of Haemophilus influenzae type b and other invasive diseases in South Korean children. Vaccine. 2004. 22:3952–3962.

8. Shin E, Lee M, Kwon S, Ki M, Kim K, Na B, Nam H, Lee S. Development of vaccination coverage estimation methods and evaluation indicators of national immunization program in Korea (in Korean). 2005. SEOUL: Korea Center for Disease Control and Prevention.
9. Zhou F, Bisgard K, Yusuf H, Deuson R, Bath S, Murphy T. Impact of universal Haemophilus influenzae type b vaccination starting at 2 months of age in the United States: an economic analysis. Pediatrics. 2002. 110:653–661.

10. Baraff L, Lee SI, Schriger DL. Outcomes of bacterial meningitis in children: a meta-analysis. Pediatr Infect Dis J. 1993. 12:389–394.
11. Jiménez FJ, Guallar-Castillón P, Rubio Terrés C, Guallar E. Cost-benefit analysis of Haemophilus influenzae type b vaccination in children in Spain. Pharmacoeconomics. 1999. 15:75–83.

12. Dagan R, Fraser D, Roitman M, Slater P, Anis E, Ashkenazi S, Kassis I, Miron D, Leventhal A. Effectiveness of a nationwide infant immunization program against Haemophilus influenzae b. The Israeli Pediatric Bacteremia and Meningitis Group. Vaccine. 1999. 17:134–141.
13. CDC. U.S. Public Health Service. A practical guide to prevention effectiveness: decision and economic analysis. 1994. Atlanta(GA):
14. Jeong H. Public financing in total health expenditure and coverage by National Health Insurance in Korea: Including comparison with other OECD countries (in Korean). Korean J Health Economics Policy. 2003. 10:95–112.
15. Drummond M, Sculpher M, Torrance G, O'Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. 2005. 3rd ed. New York: Oxford University Press.
16. Ministry of Labor. Survey Report on Wage Structure (in Korean). 2005. Korea National Statistical Office.
17. Korea Institute for Health & Social Affairs. Average age of parents at their first child birth(in Korean). 2005. Korea National Statistical Office.
18. Zepp F, Schuind A, Meyer C, Sanger R, Kaufhold A, Willems P. Safety and reactogenicity of a novel DTPa-HBV-IPV combined vaccine given along with commercial Hib vaccines in comparison with separate concomitant administration of DTPa, Hib, and OPV vaccines in infants. Pediatrics. 2002. 109:e58.
19. Livartowski A, Boucher J, Detournay B, Reinert P. Cost-effectiveness evaluation of vaccination against Haemophilus influenzae invasive diseases in France. Vaccine. 1996. 14:495–500.

20. Korea National Statistical Office. Annual report on the economically active population survey (in Korean). 2003. Korea National Statistical Office.
21. Limcangco MR, Armour CL, Salole EG, Taylor SJ. Cost-benefit analysis of a Haemophilus influenzae type b meningitis prevention programme in The Philippines. Pharmacoeconomics. 2001. 19:391–400.

22. Trollfors B. Cost-benefit analysis of general vaccination against Haemophilus influenzae type b in Sweden. Scand J Infect Dis. 1994. 26:611–614.

23. Chen RT, Rastogi SC, Mullen JR, Hayes SW, Cochi SL, Donlon JA, Wassilak SG. The Vaccine Adverse Event Reporting System (VAERS). Vaccine. 1994. 12:542–550.

24. Choung E, Kim Y, Kim Y, Kim D, Seo J, Lee H. Immunogenicity and safety of a Haemophilus influenzae type b polysaccharide-tetanus toxiod conjugate vaccine(PRP-T; Hiberix) in Korean infants (in Korean). Korean J Pediat Infect Dis. 2003. 10:71–80.
25. Korean Phamaceutical Traders Association. Import record situation of an integrative medicine item by item(in Korean). 2003. SEOUL: Korean Phamaceutical Traders Association.
26. Peltola H. Haemophilus influenzae type b disease and vaccination in Europe: lessons learned. Pediatr Infect Dis J. 1998. 17:9 Suppl. S126–S132.

27. Lau YL, Yung R, Low L, Sung R, Leung CW, Lee WH. Haemophilus influenzae type b infections in Hong Kong. Pediatr Infect Dis J. 1998. 17:9 Suppl. S165–S169.

28. Yang Y, Shen X, Jiang Z, Liu X, Leng Z, Lu D, Rao J, Liu J, Chang L. Study on Haemophilus influenzae type b diseases in China: the past, present and future. Pediatr Infect Dis J. 1998. 17:9 Suppl. S159–S165.

29. Lee YS, Kumarasinghe G, Chow C, Khor E, Lee BW. Invasive Haemophilus influenzae type b infections in Singapore children: a hospital-based study. J Paediatr Child Health. 2000. 36:125–127.
30. Kamiya H, Uehara S, Kato T, Shiraki K, Togashi T, Morishima T, Goto Y, Satoh O, Standaert SM. Childhood bacterial meningitis in Japan. Pediatr Infect Dis J. 1998. 17:9 Suppl. S183–S185.

31. Nakano T, Ihara T, Kamiya H, Yabu Y, Kuwabara H, Iwade Y, Sugiyama A. Incidence of Haemophilus influenzae type b meningitis in Mie prefecture, Japan. Pediatr Int. 2001. 43:323–324.

32. WHO. Report of a meeting on priorities for pneumococcal and Haemophilus influenzae type b(Hib) vaccine development and introduction. 2001. Geneva: Department of Vaccines and Biologicals, WHO.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download