Abstract
We report two cases of papillary thyroid carcinoma occurring after the successful treatment of osteosarcoma. One of the patients was administered with several alkylating agents and topoisomerase II inhibitor as part of the primary treatment of osteosarcoma. The onset of thyroid carcinoma occurred after 5 and 12 yr after cessation of the osteosarcoma therapy. All the patients involved in this study are alive and free of their malignancies. There have been eight case reports of these two malignancies occurring in the same patient. Thyroid carcinoma rarely occurs in patients with osteosarcoma; however, vigilant surveillance and long-term follow-up should be emphasized for all survivors.
The survival of children with osteosarcoma has improved substantially over the last 30 yr. However, as the number of long-term survivors has increased, there have been increasing concerns about the potential of late sequelae, especially in the development of second malignant neoplasms (SMN's). In previous reports with long follow-up durations, 2-5% of osteosarcoma patients developed an SMN at a median interval of 5-8 yr after osteosarcoma treatment (1-4). The pathogenic mechanisms for SMN's mainly consist of genetic predisposition and therapy-related factors including chemotherapy and especially radiation therapy. The most commonly encountered SMN in osteosarcoma are hematologic malignancy and breast cancer. Thyroid carcinomas have been described as an SMN in survivors of leukemia and Hodgkin lymphoma, occurring after craniospinal irradiation that includes the thyroid gland (5, 6). However, few studies have reported thyroid carcinoma as an SMN in osteosarcoma. Here, we report the occurrence of thyroid papillary carcinoma after the treatment of osteosarcoma in two patients who had neither a family history of cancer nor history of radiation therapy.
A 13-yr-old girl visited a local clinic for painful swelling of right arm after a minor trauma in 1988 (Fig. 1A). A pathologic fracture was suspected upon initial radiographs, and as a result, an incisional biopsy was performed, which revealed a fibroblastic osteosarcoma. She was transferred to our institution after the biopsy and was diagnosed as having in clinical stage IIB according to the Enneking's classification. She had received preoperative chemotherapy consisting of cisplatin (100 mg/m2, every 3-4 weeks, total 780 mg/m2) and doxorubicin (60 mg/m2, every 4 weeks for a total of 293 mg/m2). Despite the treatment, the patient's poor clinical response and her parents' refusal to definite surgery led us to change the chemotherapy regimen. After seven courses of bleomycin, cyclophosphosphamide and actinomycin D, the tumor was resected with a wide margin, and reconstructed with a tumor prosthesis-bone cement composite. The changed chemotherapy regimen was considered to be effective based on the clinical and histologic response, and the patient had received 4 more courses of chemotherapy with the same agents. The patient complained of dyspnea during the last course of postoperative chemotherapy and was brought in for a cardiac consultation. The echocardiogram and endomyocardial biopsy revealed the patient to be afflicted with dilated cardiomyopathy, which was consideraed to have been caused by doxorubicin. Her cardiac symptoms were mild and well-controlled with diuretics, and she had been doing well for 12 yr until a mass in her neck was discovered.
Fine-needle aspiration cytology revealed papillary carcinoma in the right lobe of thyroid. She underwent total thyroidectomy without neck dissection and a pathologic evaluation of the tissue revealed the papillary carcinoma of conventional type (Fig. 1B). The mass had a 1.2 cm diameter, and the tumor did not invade the thyroid capsule. She has not undergone radioactive iodine therapy and has been treated on thyroid replacement therapy. She showed no evidence of either malignancy at 18 yr after the diagnosis of her osteosarcoma and at 4 yr after the diagnosis of her thyroid carcinoma.
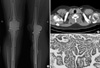
An 18-yr-old boy was diagnosed with a chondroblastic type osteosarcoma of the right proximal tibia in 2001. According to the Enneking's criteria, the osteosarcoma was in clinical stage IIB. After completing two cycles of chemotherapy that included a high-dose methotrexate, adriamycin, and cisplatin, he was treated with a limb salvage operation (Fig. 2A). Postoperative chemotherapy was performed with the same agents used in preoperative chemotherapy. In 2006 (5 yr after the diagnosis of osteosarcoma), a thyroid nodule was incidentally found on a follow-up chest CT image (Fig. 2B). The cytologic findings of a fine-needle aspiration were consistent with papillary thyroid carcinoma, and he underwent a total thyroidectomy with modified radical neck dissection shortly thereafter. The pathologic evaluation revealed a conventional type papillary carcinoma in the left thyroid lobe (Fig. 2C). The tumor showed some infiltration into perithyroidal soft tissue. A total of 15 lymph nodes were dissected, 10 of which were found to be positive for tumor cells. After the surgery, he was treated with radioactive 131I and maintained on thyroid hormone replacement therapy. Six years after the diagnosis of osteosarcoma and 1 yr after the diagnosis of thyroid carcinoma, he has been and remains free of malignancies.
Thyroid cancer accounted for 7.5% of the SMN's reported in a series of childhood survivors of malignancy (7). Most second thyroid cancers have been reported to develop after radiation therapy in survivors of leukemia and Hodgkin lymphoma. A genetic predisposition to thyroid malignancy has been observed in familial syndromes such as Pendred, hamartoma, and Gardner's syndromes (8), while familial retinoblastoma, Li-Fraumeni, Rothmund-Thomson, and Bloom syndromes were associated with osteosarcoma. In our series, none of the patients exhibited clinical features consistent with the aforementioned genetic disease. Moreover, there was no family history of genetic disease or malignancy on either of the maternal and paternal sides. However, there still remains a possibility that our patients may have a genetic syndrome such as Rothmund-Thomson syndrome, especially since the clinical features of this syndrome could be subtle. Genotype analysis of the RECQL genes including RECQL4 (for Rothmund-Thomson syndrome), RECQL2 (for Bloom syndrome), and RECQL3 (for Werner syndrome) are mandatory to rule out these syndromes.
Although most second thyroid malignancies develop after exposure to radiotherapy, none of our patients underwent radiation therapy. Some of the thyroid malignancies may have been unrelated to the primary tumors, and ocurred as it would in the general population rather than being related to either the primary cancer or the therapy. Several etiologic factors for the second thyroid cancer aside for radiation therapy have been proposed, such as the sequelae of immune suppression, the oncogenic potential of systemic chemotherapy, or some combinations of these factors.
Chemotherapy can have numerous long-term effects including, most importantly, the leukemogenic effect. There are several reports on secondary leukemias and myelodysplastic syndromes in patients treated with multi-agent chemotherapies for osteosarcoma. Recent reports have emphasized the concern of treatment-related myelodysplasia/myeloid leukemia for regimens that use high cumulative doses of alkylating agents in addition to combination therapy with topoisomerase II inhibitors. Smith et al. reported 3 cases of thyroid cancer arising in patients treated with alkylating agents without radiation (9). They proposed that alkylating agents affected DNA synthesis by binding directly to DNA. This binding resulted in damage to the normal and neoplastic cells. In the current series, the first case was administered with several alkylating agents and topoisomerase II inhibitor (including cisplatin, cyclophosphamide, ifosfamide, and adriamycin), which might have heralded the development of thyroid cancer (10).
Eight cases of thyroid carcinoma occurring in association with osteosarcoma have been reported to date (11-15). Of the eight, four patients had genetic abnormalities (most commonly the Werner syndrome). The Werner syndrome is a hereditary systemic disease characterized by premature senility. The clinical characteristics of the syndrome include small stature, scleroderma-like skin alterations, juvenile cataracts, premature facial aging, ectopic calcification, refractory ulcers, and joint contracture. The most problematic complication of Werner's syndrome is malignant tumors. Thyroid cancer, osteosarcoma, and malignant melanoma are frequently associated with this syndrome (16). In our series, no patients showed the clinical features of Werner's syndrome.
Among the remaining four patients, two underwent radiation therapy, which might have exerted deleterious effects of radiation scatter on the thyroid area, and the other two patients did not have genetic abnormalities or risk factors for SMN's. The two patients documented in previous reports and the second patient of the present report would be good candidates for the screening of unknown genetic predisposition, including single nucleotide pleomorphism. In conclusion, vigilant surveillance and long-term follow-up should be emphasized in all survivors of osteosarcoma.
Figures and Tables
Fig. 1
(A) A plain radiograph showed pathologic fracture around the surgical neck of the right humerus. The incisional biopsy confirmed the diagnosis of osteosarcoma. (B) Pathologic examination revealed a papillary carcinoma in the right lobe of thyroid. The tumor cells were tall and their cytoplasm contained eosinophilic granules and pseudostratified nuclei in several areas (stain, H&E; original magnification, ×100).

Fig. 2
(A) An anteroposterior radiograph showed pasteurized autograft-prosthesis composite reconstruction of the proximal tibial osteosarcoma. (B) Five years after the index operation, a follow-up CT scan shows a calified nodule in the left lobe of the thyroid. (C) The tumor cells showed typical overlapping, grooved, and ground glass nuclei (stain, H&E; original magnification, ×200).
References
1. Aung L, Gorlick RG, Shi W, Thaler H, Shorter NA, Healey JH, Huvos AG, Meyers PA. Second malignant neoplasms in long-term survivors of osteosarcoma: Memorial sloan-kettering cancer center experience. Cancer. 2002. 95:1728–1734.
2. Bacci G, Ferrari C, Longhi A, Ferrari S, Forni C, Bacchini P, Palmerini E, Briccoli A, Pignotti E, Balladelli A, Picci P. Second malignant neoplasm in patients with osteosarcoma of the extremities treated with adjuvant and neoadjuvant chemotherapy. J Pediatr Hematol Oncol. 2006. 28:774–780.

3. Hauben EI, Arends J, Vandenbroucke JP, van Asperen CJ, Van Marck E, Hogendoorn PC. Multiple primary malignancies in osteosarcoma patients. Incidence and predictive value of osteosarcoma subtype for cancer syndromes related with osteosarcoma. Eur J Hum Genet. 2003. 11:611–618.

4. Pratt CB, Meyer WH, Luo X, Cain AM, Kaste SC, Pappo AS, Rao BN, Fleming ID, Jenkins JJ 3rd. Second malignant neoplasms occuring in survivors of osteosarcoma. Cancer. 1997. 80:960–965.

5. Crom DB, Kaste SC, Tubergen DG, Greenwald CA, Sharp GB, Hudson MM. Ultrasonography for thyroid screening after head and neck irradiation in childhood cancer survivors. Med Pediatr Oncol. 1997. 28:15–21.

6. Farahati J, Demidchik EP, Biko J, Reiners C. Inverse association between age at the time of radiation exposure and extent of disease in cases of radiation-induced childhood thyroid carcinoma in Belarus. Cancer. 2000. 88:1470–1476.

7. Black P, Straaten A, Gutjahr P. Secondary thyroid carcinoma after treatment for childhood cancer. Med Pediatr Oncol. 1998. 31:91–95.

8. De Keyser LF, Van Herle AJ. Differentiated thyroid cancer in children. Head Neck Surg. 1985. 8:100–114.

9. Smith MB, Xue H, Strong L, Takahashi H, Jaffe N, Ried H, Zietz H, Andrassy RJ. Forty-year experience with second malignancies after treatment of childhood cancer: Analysis of outcome following the development of the second malignancy. J Pediatr Surg. 1993. 28:1342–1348.

10. Neglia JP, Meadows AT, Robison LL, Kim TH, Newton WA, Ruymann FB, Sather HN, Hammond GD. Second neoplasms after acute lymphoblastic leukemia in childhood. N Engl J Med. 1991. 325:1330–1336.

11. Goto M, Miller RW, Ishikawa Y, Sugano H. Excess of rare cancers in werner syndrome (adult progeria). Cancer Epidemiol Biomarkers Prev. 1996. 5:239–246.
12. Jimenez M, Leon P, Castro L, Azcona C, Sierrasesumaga L. Second tumors in pediatric oncologic patients. report of 5 cases. Rev Med Univ Navarra. 1995. 40:72–77.
13. Tsuchiya H, Tomita K, Ohno M, Inaoki M, Kawashima A. Werner's syndrome combined with quintuplicate malignant tumors: a case report and review of literature data. Jpn J Clin Oncol. 1991. 21:135–142.

14. Verneris M, McDougall IR, Becton D, Link MP. Thyroid carcinoma after successful treatment of osteosarcoma: a report of three patients. J Pediatr Hematol Oncol. 2001. 23:312–315.

15. Yen BC, Kahn H, Schiller AL, Klein MJ, Phelps RG, Lebwohl MG. Multiple hamartoma syndrome with osteosarcoma. Arch Pathol Lab Med. 1993. 117:1252–1254.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download