Abstract
The aims of this study were to find an optimal basal infusion dose of fentanyl for parent-controlled analgesia (PrCA) in children undergoing cleft palate repair and the degree of parents' satisfaction with PrCA. Thirty consecutive children between 6 months and 2 yr of age were enrolled. At the end of surgery, a PrCA device with a basal infusion rate of 2 mL/hr and bolus of 0.5 mL with lockout time of 15 min was applied. Parents were educated in patient-controlled analgesia (PCA) devices, the Wong Baker face pain scoring system, and monitoring of adverse effects of fentanyl. Fentanyl was infused 0.3 µg/kg/hr at first, and we obtained a predetermined fentanyl regimen by the response of the previous patient to a larger or smaller dose of fentanyl (0.1 µg/kg/hr as the step size), using an up-and-down method. ED50 and ED95 by probit analysis were 0.63 µg/kg/hr (95% confidence limits, 0.55-0.73 µg/kg/hr) and 0.83 µg/kg/hr (95% confidence limits, 0.73-1.47 µg/kg/hr), respectively. Eighty seven percent of the parents were satisfied with participating in the PrCA modality. PrCA using fentanyl with a basal infusion rate of 0.63 µg/kg/hr can be applied effectively for postoperative pain management in children undergoing cleft palate repair with a high level of parents' satisfaction.
Children undergoing operations may suffer from severe pain as well as fear and anxiety even after minor surgery; therefore, inadequate analgesia may cause greater physical and emotional stress on children than adults (1). In the past, the conventional pain management was achieved with the intermittent injection of analgesics. Concerns about opioid overdose often result in suboptimal analgesia due to dose errors and dosage interval errors. Lack of experience and inability to assess pain in non-verbal children has contributed to the inadequate provision of analgesia in this group. Though patient-controlled analgesic (PCA) device has now become the primary modality for the management of moderate to severe postoperative pain in older children and adolescents (2, 3), continuous intravenous opioid infusions are still reserved these days for preverbal children who cannot handle the PCA devices. Recently, parent- or nurse-controlled analgesia with opioid showed some advantages over the continuous opioid infusion (4). Since adequate assessment of pain and analgesic response is a critical component of pain management in preverbal children, parent-controlled analgesia (PrCA) still remains as a practical challenge in pediatric anesthesia.
Cleft palate repair common in 1-2 yr old children, involving the soft and hard palate, requires postoperative pain management (5). Therefore, it is worthwhile to develop a procedure-specific postoperative pain management regimen for these preverbal patients (6).
The aims of this study were to find an optimal basal infusion dose of fentanyl for PrCA in preverbal patients undergoing cleft palate repair and the level of parents' satisfaction with participating in PrCA for their children.
This study was approved by the institutional review board, and informed consent was obtained from parents after explaining the study protocol. On the day of pre-anesthetic visit, the parents were taught the principles of PCA devices and their role in the study; such as how to give bolus doses, how to monitor the efficacy of analgesia, and also how to identify adverse effects during the study periods. Parents were well-educated and tested how to handle the PCA device for this study.
Thirty consecutive children between 6 months and 2 yr of age who underwent cleft palate repair were enrolled in this study. All children were ASA physical status I or II, and born at full term. Children with apnea history, Pierre-Robin syndrome, or any congenital heart or neurological diseases were excluded (7). Premedication was not prescribed. Intravenous catheterization was performed at ward. All patients were monitored with electrocardiography, noninvasive blood pressure, and pulse oximetry when they arrived in the operating room. Anesthesia was induced with thiopental sodium 5 mg/kg, and rocuronium 0.6 mg/kg was given intravenously for neuromuscular blockade. After endotracheal intubation, the lungs were ventilated with 50% air in oxygen and sevoflurane. For intraoperative pain control, the incision sites were infiltrated with lidocaine by the surgeon. After the completion of the operation, neuromuscular block was reversed with neostigmine 0.03 mg/kg and atropine 0.01 mg/kg.
Before sending the children to the post-anesthetic care unit, the PCA pump (Accufuser®, Woo Young Medical, Seoul, Korea) with a fixed basal infusion rate of 2 mL/hr and bolus of 0.5 mL with lockout time of 15 min as rescue therapy was attached to a continuously infusing intravenous catheter. The fentanyl regimen was coded on the basal infusion rate of fentanyl: for example, 'fentanyl regimen 0.3' notes a basal infusion of 0.3 µg/kg/hr and bolus injections on demand, dose of quarter of basal infusion with lockout time of 15 min. PCA pump was set initially as 'fentanyl regimen 0.3', and the next regimen was predetermined by the response of the previous patient to a larger or smaller dose (with 'fentanyl regimen 0.1' as a step size), using a modification of the Dixon's up-and-down method (8). The patient's response to the fentanyl regimen was evaluated by parents according to the Wong-Baker face pain rating scale of 10 at resting state, as being 10 with maximal pain and 0 with no pain (9). Pain score was recorded by parents at 2-hr intervals for the first 12-hr, at 6-hr intervals for the second 12-hr and every 12-hr thereafter until 48 hr. We defined the patient's response to the PCA regimen as 'Effective' or 'Not effective'. 'Effective' refers to average pain score less than 5 for 2 days and 'Not effective' refers to greater than or equal to 5. If further analgesia is required, ibuprofen syrup (5 mg/kg) was administered on demand.
The observed Effective Dose50 (EDo50) for the fentanyl regimen was estimated by calculating the average of cross-over midpoints of fentanyl regimens of all independent pairs of patients involving a cross-over (i.e. 'Effective' to 'Not effective').
The degree of sedation was assessed by parents, by using four-point patient sedation score (PSS) at 6-hr intervals (10). The PSS was assigned as follows: 1=asleep, not arousal by
verbal contact; 2=asleep, arousal by verbal contact; 3=drowsy/ not sleeping; and 4=alert/aware. The PSS was used to quantify sedation and also help identify side effects, such as respiratory depression from excessive sedation. Occurrences of side effects such as vomiting or respiratory depression were recorded at 6-hr intervals. If the patient had side effects, infusion would be immediately stopped and the appropriate management would be taken and recorded. Because of concerns about the potential for respiratory depression, supplemental oxygen and naloxone were prepared on an as-needed basis for all patients. If the patient had vomiting, ondansetron 0.1 mg/kg was administered. At the completion of study, a questionnaire on the satisfaction of parents was recorded with four-point rating scale (excellent=1, good=2, fair=3, and poor=4).
For statistical analysis, analysis of variance and multiple comparisons using Bonferroni's correction were used. We also used a probit analysis (SPSS 12.0; SPSS Inc., Chicago, IL, U.S.A.) in order to obtain the probability of 50% and 95% effectiveness of pain relief (predicted Effective Dose EDp50 and EDp95) and 95% confidence limits. For sample size calculation, we estimated that a minimum of 25 patients would be required to maintain the limit of error of estimated EDp50 <0.2 for an up-and-down sequential allocation design. All data were expressed as mean±SD or number of responses, as appropriate. A p value <0.05 was considered as statistically significant.
The mean age of the patients was 1.2±0.2 yr old, mean body weight was 10.2±1.1 kg, and the gender ratio was 14:16 (male:female). The observed ED50 (EDo50) was 0.66± 0.08 µg/kg/hr (Fig. 1), and the dose-response plot, constructed on the basis of probit analysis data (Fig. 2), showed that the EDp50 and EDp95 of the fentanyl regimen were 0.63 µg/kg/hr (95% confidence limits, 0.55-0.73 µg/kg/hr) and 0.83 µg/kg/hr (95% confidence limits, 0.73-1.47 µg/kg/hr) along with an equation plot of probit (response=-1.54+3.1×'fentanyl regimen' and r2=0.95), respectively. Maximum likelihood estimators of the probit model variables showed a p value of 0.593 and a goodness of fit chi-square of 0.964. EDo50 was similar to EDp50. Most of bolus injections were administered only during the first postoperative day, and the total dose of fentanyl consumption during the first day increased proportionally to fentanyl regimens (p<0.05) (Table 1). Three patients (25%) managed with fentanyl regimen 0.7 (one) or 0.8 (two), experienced vomiting on the day of surgery and were effectively treated with ondansetron 0.1 mg/kg. None of the patients was apneic or over-sedated (PSS <2). Eighty seven percent of parents were satisfied with the participation in the PrCA modality (excellent or good) (Table 2).
The framework of PrCA using PCA devices consists of continuous basal infusions and bolus injections on a demand basis by parents. The role of parents in this study was to evaluate the analgesic response of their child to the basal infusion of fentanyl, administer bolus injections on a demand basis, and also to monitor the appearance of adverse effects such as respiratory depression, nausea, and vomiting. We employed the Wong-Baker face pain rating scale (8) as the pain assessment tool for parents because of its simplicity and non-reliance on confusing physiological parameters which would be inappropriate for parents (11).
With regard to the agent of PrCA regimen for preverbal children, avoidance of the adverse effects of opioid is as important as relief of pain. A short-acting opioid such as fentanyl is preferred to long-acting opioid such as morphine and hydromorphone, because fentanyl does not have any significant adverse effects on the cardiovascular system and its metabolites do not include active forms.
In our study, EDo50 and EDp50 were similar. The EDp50 and EDp95 of the fentanyl regimen were 0.63 and 0.83 µg/kg/hr, respectively. The ED50 in our study was different from the median infusion dose (fentanyl 0.86 µg/kg/hr) of surgical patients less than 6 yr of age (12). This difference could be explained by pharmacokinetic differences of fentanyl by age (13), different types of surgery and statistical parameters. We also measured the number of bolus injections and total consumption dose of fentanyl. Most patients were administered with bolus injections only during the first 12 hr. The total consumption dose of fentanyl was increased proportionally, and the bolus doses were decreased proportionally, to fentanyl regimens (Table 1). This implies optimal basal infusion could decrease the bolus requirements and improve overall quality of analgesia (14). As the confidence limits of ED95 were in a wide range, the ED50 of fentanyl regimen was recommended for children undergoing cleft palate repair. Considering that there are no reports on procedure-specific postoperative pain management regimens available for preverbal children, our results may suggest a fentanyl regimen for PrCA for preverbal children undergoing cleft palate repair as procedure-specific pain management (6).
There were some limitations in our study, particularly in the pain assessment. The parents evaluated the analgesic responses by Wong-Baker faces pain rating scale (9), which is usually suitable for the age of 3 and over. Pain assessment of the children by their parents might correlate only moderately with the children's pain score and shows a poor level of agreement (15). We only adjusted the fentanyl regimen according to the pain score evaluated by the parents. Another potential pitfall exists in our study. Although we applied pulse oximetry to the patients during the early study periods, frequent alarms due to technical problems such as motion artifacts or dislodgements of sensor probe made parents anxious and nervous and we abandoned to monitor pulse oximetry. Therefore, for the patient's safety, we informed parents how to monitor respiratory patterns and rate, and recognize appearance of cyanosis. Also, we asked nurse staff in ward to take care of patient's postoperative care as usual.
Since the incidence of vomiting seemed to be related to the total fentanyl consumption dose, PrCA in preverbal patients is still challenging and needs further evaluation before recommending on a wider scale.
Apart from the analgesic responses of patient to the PrCA modality, we got questionnaires on parents' satisfaction of participating in the PrCA modality after completion of the study. Interestingly, 87% of parents were satisfied with their participating in their children's postoperative pain management even though the majority of parents whose children managed with the fentanyl regimen less than 0.5 assessed 'Non-effective' response. This suggested that the most of parents were willing to be involved in the postoperative management for their children and, in particular, with PrCA.
In conclusion, the ED50 and ED95 of the fentanyl regimen for PrCA were 0.63 and 0.83 µg/kg/hr, respectively. PrCA using fentanyl can be applied effectively for postoperative pain management in preverbal children undergoing cleft palate repair with a high level of parents' satisfaction.
Figures and Tables
Fig. 1
The responses of 30 consecutive patients by the parent-controlled analgesic (PrCA) modality with different fentanyl regimens. Patient's response to the PrCA regimen was described as 'Effective' (open circle) or 'Not effective' (close circle). Fentanyl regimen was coded by the numeric of the basal infusion rate ( µg/kg/hr). Arrows indicate the midpoint of fentanyl regimens of all independent pairs of patients, involving a crossover from 'Not effective' to 'Effective'.

Fig. 2
Probit analysis of fentanyl regimen. Triangles in the bottom represent the patients of 'Not effective', and reverse triangles in the top represent the patients of 'Effective'. Regression plot and line were displayed according to probit analysis.
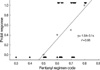
Table 1
Total consumption dose of fentanyl with different fentanyl regimens

Values are mean±SD (total dose) and the number of patients. *p<0.05 vs. fentanyl regimen 0.5; †p<0.001 vs. fentanyl regimen 0.5 and 0.6; ‡p<0.001 vs. fentanyl regimen 0.5, 0.6 and 0.7. Data were obtained during the first postoperative day, and the fentanyl regimen 0.3 and 0.4 were excluded from statistical comparison because of the small sample size.
References
1. Munro HM, Malviya S, Lauder GR, Voepel-Lewis T, Tait AR. Pain relief in children following outpatient surgery. J Clin Anesth. 1999. 11:187–191.

2. Peters JW, Bandell Hoekstra IE, Huijer Abu-Saad H, Bouwmeester J, Meursing AE, Tibboel D. Patient controlled analgesia in children and adolescents: a randomized controlled trial. Paediatr Anaesth. 1999. 9:235–241.

3. Verghese ST, Hannallah RS. Postoperative pain management in children. Anesthesiol Clin North America. 2005. 23:163–184.

4. Kanagasundaram SA, Cooper MG, Lane LJ. Nurse-controlled analgesia using a patient-controlled analgesia device: an alternative strategy in the management of severe cancer pain in children. J Paediatr Child Health. 1997. 33:352–355.

5. Roulleau P, Gall O, Desjeux L, Dagher C, Murat I. Remifentanil infusion for cleft palate surgery in young infants. Paediatr Anaesth. 2003. 13:701–707.

6. Kehlet H. Procedure-specific postoperative pain management. Anesthesiol Clin North America. 2005. 23:203–210.

7. Dell'Oste C, Savron F, Pelizzo G, Sarti A. Acute airway obstruction in an infant with Pierre Robin syndrome after palatoplasty. Acta Anaesthesiol Scand. 2004. 48:787–789.
9. Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988. 14:9–17.
10. Klimscha W, Chiari A, Michalek-Sauberer A, Wildling E, Lerche A, Lorber C, Brinkmann H, Semsroth M. The efficacy and safety of a clonidine/bupivacaine combination in caudal blockade for pediatric hernia repair. Anesth Analg. 1998. 86:54–61.

11. Buttner W, Finke W. Analysis of behavioural and physiological parameters for the assessment of postoperative analgesic demand in newborns, infants and young children: a comprehensive report on seven consecutive studies. Paediatr Anaesth. 2000. 10:303–318.
12. Monitto CL, Greenberg RS, Kost-Byerly S, Wetzel R, Billett C, Lebet RM, Yaster M. The safety and efficacy of parent-/nurse-controlled analgesia in patients less than six years of age. Anesth Analg. 2000. 91:573–579.

13. Katz R, Kelly HW. Pharmacokinetics of continuous infusions of fentanyl in critically ill children. Crit Care Med. 1993. 21:995–1000.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download